Key Message
Using evidence from other successful childhood vaccination programs and from behavioural science, we identify four broad evidence-based strategies for increasing COVID-19 vaccination uptake in children and youth: 1) School-based vaccination, 2) Healthcare provider recommendation, 3) Reminders and recall systems, and 4) Public health communication campaigns.
Across each intervention, behavioural science principles can be used to optimize COVID-19 vaccination uptake amongst children and youth including leveraging recommendations from trusted sources; tailoring messaging and experience to children, youth, and their parents/caregivers through individual and population-based approaches; and ensuring special considerations for reaching at-risk and racialized communities.
Summary
Background
Recognition of effective strategies and early collaborative planning is essential to ensure optimal uptake and engagement of all children and youth eligible for COVID-19 vaccination. At the time of writing, Health Canada has authorized two mRNA vaccines for use in youth born in 2009 or earlier (i.e., Pfizer-BioNTech Comirnaty and Moderna Spikevax), receiving a strong recommendation from the National Advisory Committee on Immunization (NACI).
Questions
What influences vaccination behaviour in children and youth?
What strategies are effective for increasing vaccination in children and youth?
What behavioural science principles can be used to support vaccination in children and youth?
Findings
By leveraging behavioural sciences to promote vaccine uptake in children and youth we can understand key influences on vaccination such as threat perception, leadership, individual and collective interests, science communication, social context, and stress and coping.
School-based vaccination programs are a high-impact and effective approach for increasing uptake that address many practical issues (e.g., reach, convenience, feasibility, accessibility, equity). Healthcare provider recommendation is a well-researched strategy for increasing vaccine uptake in children. Reminder systems are among the most effective strategies to improve vaccine coverage in the Canadian context, including reminders for the next vaccine dose and recall for missed vaccination.
Healthcare providers are trusted sources for assessing and addressing the informational, logistical, and practical barriers to vaccination. School-based and community health communication campaigns are effective if delivered by authoritative sources and included parents. Efforts should be made to address misinformation, reduce risk perception, promote positive attitudes towards vaccines (e.g., including in needle phobia campaigns), and stimulate action (i.e., vaccination).
There are four behavioural science-informed principles to support COVID-19 vaccination: build and leverage trust; avoid one-size-fits-all approaches; ensure special considerations for reaching at-risk populations; and ensure special considerations for reaching black, indigenous and all racialized communities.
Interpretation
Given ongoing implementation of the youth COVID-19 vaccination program in Ontario and pending Health Canada approval of COVID-19 vaccines for children aged 5-11, increasing COVID-19 vaccine acceptance and uptake in children and youth will help allow them to continue safely returning to pre-pandemic activities by reducing transmission, hospitalizations, and severe outcomes.
Full Text
Background
The Rationale for Vaccinating Children and Youth with COVID-19 Vaccines
There is much to draw from behavioural science to continue to optimize the ongoing youth (12-17 years) vaccination program. Recognition of effective strategies and early collaborative planning is essential to ensure optimal uptake and engagement of all children and youth eligible for COVID-19 vaccination. At the time of writing, Health Canada has authorized two mRNA vaccines for use in youth born in 2009 or earlier (i.e., Pfizer-BioNTech Comirnaty and Moderna Spikevax), receiving a strong recommendation from NACI: “NACI recommends that a complete series with an mRNA COVID-19 vaccine should be offered to adolescents 12 to 17 years of age who do not have contraindications to the vaccine.”1
The Canadian Paediatric Society has advocated for vaccination of individuals aged 12 years or over.2 As of October 20, 2021, 83% of youth aged 12-17 in Ontario received at least one dose of a COVID-19 vaccine, and 76% are fully vaccinated (e.g., received two doses).3 Evidence on COVID-19 vaccination in children 11 years and younger is now emerging from clinical trials and being shared with regulators in Canada and the United States. Pfizer-BioNTech has submitted initial trial data for its COVID-19 vaccine in 5–11-year-olds to Health Canada and the U.S. Food and Drug Administration.4 Clinical trials for Moderna’s vaccine are ongoing in 6-11 year-olds.5
COVID-19 vaccination in children and youth is important for multiple reasons. First and foremost: to prevent SARS-CoV-2 infection and the risk of rare complications of SARS-CoV-2 (e.g., multisystem inflammatory syndrome),6 hospitalization, post-COVID condition,7,8 and also to prevent community spread as children have been shown to transmit SARS-CoV-2 to other children or adults.2,9 Vaccination against COVID-19 has been shown to reduce SARS-CoV-2 viral shedding and the likelihood of SARS-CoV-2 transmission within household thus vaccinating children and youth will decrease their likelihood of transmitting SARS-CoV-2,10 leading to reduced overall transmission within school settings and in the community. Limiting the spread and number of outbreaks within schools will be a crucial part of a full- and long-term normalization of children’s education by avoiding school closures and cohort dismissal.11
Vaccination against COVID-19 presents benefits to individual Ontarians and the province overall. Vaccination reduces the risk of infection associated with close interactions and supports a safer return to socialization including with friends and family, participating in athletic or arts-based extracurricular activities, attending camps, recreational centres, and other community events. This enables children to have important educational and social experiences. In addition, a return to participation in these activities would accrue benefit for the mental health and psychosocial wellbeing of children, youth, and parents/caregivers (hereafter parents). Herein, we focus primarily on behavioural science consideration for children and youth vaccination, while recognizing that parents are centrally important to fostering vaccination acceptance and uptake and should be equally supported alongside children and youth.
Questions
What influences vaccination behaviour in children and youth?
What strategies are effective for increasing vaccination in children and youth?
What behavioural science principles can be used to support vaccination in children and youth?
Findings
Leveraging Behavioural Sciences to Promote Vaccine Uptake in Children and Youth
To increase vaccine acceptance and uptake, we must consider a wide range of factors linked to under-vaccination and their relative contributions to suboptimal coverage. Behavioural science combines methods and approaches from psychology, economics, and other social science disciplines that can help to identify and reduce barriers to vaccine acceptance and uptake. By leveraging behavioural science, we can understand key influences on vaccination such as threat perception, leadership, individual and collective interests, science communication, social context, and stress and coping (see Figure 1).12 These insights can guide vaccination programs in developing strategies to improve uptake and prioritize interventions.
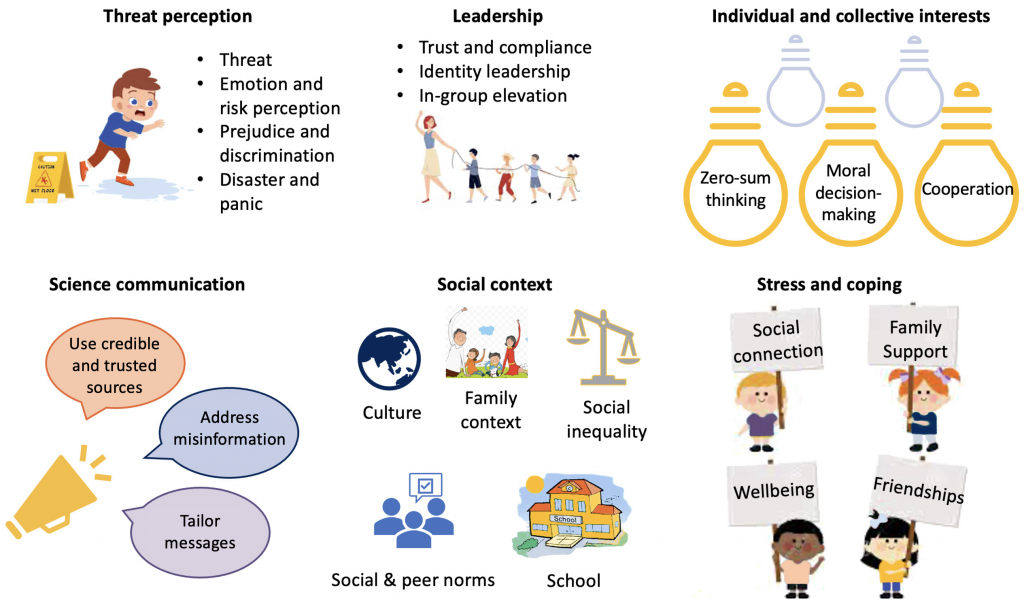
Figure adapted from van Bavel et al. 2020.12
The World Health Organization’s behavioural and social drivers (BeSD) is a useful framework for ensuring that strategies for increasing vaccination reflect four domains that drive vaccine acceptance and uptake: 1) Thinking and feeling (including individual cognitive and emotional responses), 2) Social processes (including people’s experiences related to vaccination when interacting with family, friends, and their broader social network), 3) Motivation (including people’s willingness or hesitancy to get a vaccine), and 4) Practical issues (including the experiences people have when trying to get vaccinated such as accessing vaccination services) (see Figure 2).13
The BeSD model was developed through a comprehensive process to ensure measurability in individuals, specificity to the drivers of vaccination, and modifiability by vaccination programs. It was developed for childhood vaccination,13,14and has already been adapted for COVID-19 vaccination in adults.15 The BeSD domains should be thoughtfully targeted, if they are creating barriers for vaccination, using evidence-based strategies tailored to children and youth. Research has shown that multi-component interventions are more effective than single-component interventions.16–18 Therefore, strategies that target multiple domains concurrently is likely to be most successful.19,20
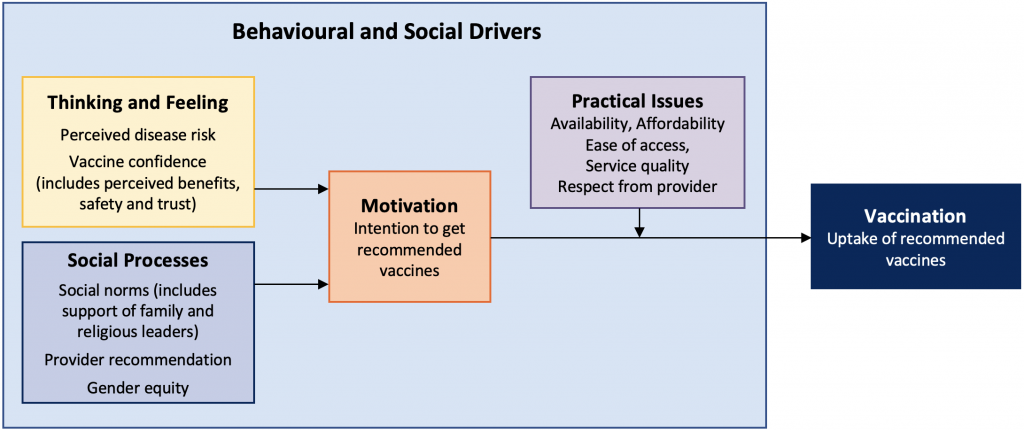
Figure adapted from the BeSD expert working group.13,14 Based on the Increasing Vaccination Model (IVM).19
Evidence-Based Strategies to Increase Vaccine Uptake in Children and Youth
In the last two decades, there has been an increase in the development of strategies aiming to promote vaccine uptake in children and youth. We highlight four key strategies below; however, there are also necessary but insufficient conditions that are pivotal to all of the following strategies such as the availability of free vaccination,21 the promotion of trust in vaccines and health services,22 tailoring clear messaging regarding risks and benefits to developmental ages, and surveillance systems to monitor vaccine safety and uptake.23 It is also important for any strategy to acknowledge and prepare for scenarios in which youth want to get vaccinated, but parents do not (or vice versa). For each of the outlined strategies, it is also crucial to consider different developmental stages within children and youth, and tailor the strategy accordingly (e.g., ability to consent). A one-size-fits-all approach risks leaving some behind.
School-Based Vaccination
School-based vaccination programs are a high-impact and effective approach for increasing uptake that address many practical issues (e.g., reach, convenience, feasibility, accessibility, equity)21,24 and social processes (e.g., promoting of social norms in favour of vaccination). Canadian schools are familiar locations for rolling out a number of youth vaccines (e.g., Hepatitis B, human papillomavirus (HPV) and meningococcal vaccines).25 In-school vaccination programs in Ontario have traditionally not been used for younger age groups, however, it may be possible in some cases to work with local public health units to deliver rollout in schools.
When school-based vaccination is not available, children and youth must receive vaccines at other locations in the community (e.g., primary care, walk-in clinics). This may lead to reduced access and uptake in individuals from lower social and economic groups.24 Although school-based programs may not be appropriate for all ages, schools can function as trusted and central locations for vaccination clinics after-school hours or on weekends to leverage the reach, equity, and safe space of schools while enabling parental presence if desired. This builds on the success of school-based vaccination programs.
Healthcare Provider Recommendation
Healthcare provider recommendation is a well-researched strategy for increasing vaccine uptake in children.22,26–29 In order for healthcare providers to make an effective vaccine recommendation, it is necessary to inform, prompt and provide educational training and resources to providers about evolving COVID-19 vaccine recommendations and the rationale for vaccinating children and youth.16,30–39 It may be helpful to partner with primary care providers to administer vaccines in their offices,40 and ensure parents are supported to have adequate paid time off for their children’s appointments.
Healthcare providers are trusted sources for assessing and addressing the informational, logistical, and practical barriers to vaccination.19 This may include addressing concerns about vaccination in children, youth, and parents,41 as well as providing practical support (e.g., understanding where to get vaccinated). To maximize impactful communication with parents, the use of shared decision-making and motivational interviewing techniques have been identified as useful strategies.17,29,42,43
Reminders for the Next Vaccine Dose and Recall for Missed Vaccination
Reminders for the next vaccine dose and recall for missed vaccination have also demonstrated impact.29,44–49Personalized reminders focused on children, youth, parents, or providers have been shown to be effective.17,49,50 In a vaccine registry, reminders can be sent directly to individuals who have received one COVID-19 vaccine dose to prompt individuals when they are due for their second dose. There are many modalities of reminders such as mail, letter, telephone, email, or text; yet, different modalities have shown efficacy.49,51
A recent systematic review of multiple strategies to increase acceptability of vaccines in the Canadian setting found that reminder systems are among the most effective strategies to improve vaccine coverage in the Canadian context.52Reminders and recall may be particularly important for the second dose when other barriers besides motivation to get vaccinated are at play.53 Reminders and recall strategies are acceptable and financially feasible solutions,51,54 and should work within available systems.
School-Based and Community Health Communication Campaigns
School-based and community health communication campaigns are effective if delivered by authoritative sources and included parents.55,56 Communication campaigns should consider children, youth, and parents as key audiences. Authoritative sources could include recognized institutions, organizations (e.g., the Canadian Paediatric Society), respected community leaders and local influencers. Community engagement is important to the success of such campaigns,57–59 especially in minority populations where trusted community leaders (e.g., clergy) and organizations (e.g., community centres) in diverse and racialized communities can help tailor the message appropriately.55 Delivering information in public health campaigns is not enough; efforts should be made to address misinformation, reduce risk perception, promote positive attitudes towards vaccines (e.g., including in needle phobia campaigns), and stimulate action (i.e., vaccination).
While there are increasing reports on the effectiveness of the four strategies listed above, some limitations to the existing literature should be acknowledged. First, it is important to understand the context of the jurisdictions in which these strategies have been implemented, as they may not be as effective in different settings. Thus, the effectiveness of strategies to increase vaccine uptake should always be assessed locally, in rural and urban environments, and across a diversity of parents and children. Different forms of incentives and rewards (e.g., stickers) tailored to children and youth may also improve vaccine uptake, whereas financial incentives (e.g., gift cards or lotteries) may also be effective in youth;34 however, greater evidence is required.
Behavioural Science Principles to Support Vaccination in Children and Youth
To optimize the impact of the four strategies above, we identify four behavioural science-informed principles to support COVID-19 vaccination in children (5-11 years) and youth (12-17 years) (see Table 1 for differential considerations for each group):
Build and Leverage Trust
Trust (or lack thereof) factors into vaccine acceptance and uptake in general and in parents/caregivers.60,61 Involve trusted sources and familiar spaces for supporting vaccination in children and youth. As these may differ between each group, involve a diversity of children and youth as well as parents in program planning as early as possible. Trusted sources include not only those in leadership roles in the community (e.g., teachers, health professionals, religious leaders, coaches) but also informal social connections. These include neighbours and friends (in person and online) as similarity and relatedness are often key in influential social connections.62–64
Avoid One-Size-Fits-All Approaches
The vaccination experience should be tailored to children, youth, and parents, and disseminated by trusted sources (see point 1). This can be done by highlighting the benefits of vaccines, ensuring a mechanism exists to address specific vaccine safety and efficacy concerns as they arise, reassuring the robustness of monitoring adverse events following immunization in Ontario, and tapping into motivation by tying vaccination to personal values and priorities. We recommend tailoring risk and benefit communication to children’s developmental stage and to varying health literacy and health numeracy by drawing on best practices in risk communication. We also recommend eliciting the involvement of children, youth, and parents (as appropriate) in designing and sustaining public campaign messages. Invest early in infrastructure, education, and resources to empower trusted sources (e.g., community leaders, teachers, health professionals)65 and settings (e.g., schools, clinics, community health centres) to have effective, empathetic conversations about vaccine questions that children, youth, or parents may have.
Ensure Special Considerations for Reaching At-Risk Populations
Children with behavioural and physical disabilities, youth experiencing homelessness, and other at-risk populations are deserving of additional consideration to optimize vaccination experience.66 This includes partnering with organizations such as shelters that support precariously housed and homeless children and youth in receiving vaccinations. It also includes ensuring accessible information, accessible physical locations for vaccinations, wheelchair access, offering free or accessible transportation to vaccination sites for those who need it, and providing information about vaccination in multiple formats and languages.
Ensure Special Considerations for Reaching Black, Indigenous and All Racialized Communities
Surveys data from Black, Indigenous and other racialized communities have shown lower vaccine confidence. Trust-building strategies with community leaders and trusted partners to tailor messaging and build trust have been demonstrated to be effective.67 To this end, special efforts should be made to engage religious and spiritual leaders and highly respected elders, given the important leadership roles that they have in these communities.68

Interpretation
Given ongoing implementation of the youth COVID-19 vaccination program in Ontario and pending Health Canada approval of COVID-19 vaccines for children aged 5-11, increasing COVID-19 vaccine acceptance and uptake in children and youth will help allow them to continue safely returning to pre-pandemic activities by reducing transmission, hospitalizations, and severe outcomes. Evidence from other childhood and youth vaccination programs to increase COVID-19 vaccine uptake in children and youth suggests a combination of school-based vaccination programs and/or clinics, healthcare provider recommendations, reminders and recall strategies, and appropriately messaged school-based, community-specific, and public health campaigns. These strategies should be tailored to children’s age, feasibility, and acceptability in children, youth, and their parents. Prioritizing research and evaluation to determine which strategies for encouraging vaccine acceptance and uptake work, for whom, and in what circumstances, will continue to be crucial to further develop evidence-based strategies that would in turn inform vaccination strategies. Based on existing evidence, the Behavioural Science Working Group developed key principles to support COVID-19 vaccination in children and youth that include leveraging recommendations from trusted and familiar sources tailored to the group; tailoring messaging and experience to children, youth, and parents through individual-and population-based approaches; and ensuring special consideration for reaching at-risk and racialized communities as well as those in under-vaccinated communities.
References
1. Public Health Agency of Canada. Recommendation on the use of mRNA COVID-19 vaccines in adolescents 12 to 17 years of age. Published August 27, 2021. https://www.canada.ca/en/public-health/services/immunization/national-advisory-committee-on-immunization-naci/recommendations-use-covid-19-vaccines/mrna-adolescents.html
2. Canadian Paediatric Society. COVID-19 vaccine for children. Published 2021. https://www.cps.ca/en/documents/position/covid-19-vaccine-for-children
3. Government of Ontario. COVID-19 vaccinations data. COVID-19 (coronavirus) in Ontario. Published 2021. https://covid-19.ontario.ca/data
4. Health Canada. Health Canada receives submission from Pfizer-BioNTech to authorize the use of Comirnaty COVID-19 vaccine in children 5 to 11 years of age. Published October 18, 2021. https://www.canada.ca/en/health-canada/news/2021/10/health-canada-receives-submission-from-pfizer-biontech-to-authorize-the-use-of-comirnaty-covid-19-vaccine-in-children-5-to-11-years-of-age.html
5. ModernaTX, Inc. A study to evaluate safety and effectiveness of MRNA-1273 COVID-19 vaccine in healthy children between 6 months of age and less than 12 years of age. clinicaltrials.gov; 2021. https://clinicaltrials.gov/ct2/show/NCT04796896
6. Go E, El Tal T, Tsoukas P, et al. Comparing apples to apples in post-COVID-associated multisystem inflammatory syndrome in children (MIS-C). Social Science Research Network; 2021. https://doi.org/10.2139/ssrn.3894907
7. Drouin O, Hepburn CM, Farrar DS, et al. Characteristics of children admitted to hospital with acute SARS-CoV-2 infection in Canada in 2020. Can Med Assoc J. 2021;193(38):E1483-E1493. https://doi.org/10.1503/cmaj.210053
8. Lewis D. Long COVID and kids: Scientists race to find answers. Nature. 2021;595(7868):482-483. https://doi.org/10.1038/d41586-021-01935-7
9. Gouvernment of Ontario. Health care consent act. Ontario.ca. Published 1996. https://www.ontario.ca/laws/statute/96h02
10. Harris RJ, Hall JA, Zaidi A, Andrews NJ, Dunbar JK, Dabrera G. Effect of vaccination on household transmission of SARS-CoV-2 in England. N Engl J Med. Published online June 23, 2021. https://doi.org/10.1056/NEJMc2107717
11. Ministry of Health. COVID-19 guidance: School case, contact, and outbreak management. Government of Ontario; 2021:27. https://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/COVID-19_school_outbreak_guidance.pdf
12. Bavel JJV, Baicker K, Boggio PS, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav. 2020;4(5):460-471. https://doi.org/10.1038/s41562-020-0884-z
13. Shapiro GK, Kaufman J, Brewer NT, et al. A critical review of measures of childhood vaccine confidence. Curr Opin Immunol. 2021;71:34-45. https://doi.org/10.1016/j.coi.2021.04.002
14. Brewer N, Leask J, Shapiro G, Wiley K. Development of tools to measure behavioural and social drivers (BeSD) of vaccination: Progress report. World Health Organization; 2020. https://cdn.who.int/media/docs/default-source/immunization/besd_progress_report_june2020.pdf?sfvrsn=10a67e75_3
15. World Health Organization. Data for action: Achieving high uptake of COVID-19 vaccines. World Health Organization. Published 2021. https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-vaccination-demand-planning-2021.1
16. Frew PM, Lutz CS. Interventions to increase pediatric vaccine uptake: An overview of recent findings. Hum Vaccines Immunother. 2017;13(11):2503-2511. https://doi.org/10.1080/21645515.2017.1367069
17. Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ, SAGE Working Group on Vaccine Hesitancy. Strategies for addressing vaccine hesitancy – A systematic review. Vaccine. 2015;33(34):4180-4190. https://doi.org/10.1016/j.vaccine.2015.04.040
18. Acampora A, Grossi A, Barbara A, et al. Increasing HPV vaccination uptake among adolescents: A systematic review. Int J Environ Res Public Health. 2020;17(21):7997. https://doi.org/10.3390/ijerph17217997
19. Brewer NT, Chapman GB, Rothman AJ, Leask J, Kempe A. Increasing vaccination: Putting psychological science into action. Psychol Sci Public Interest. 2018;18(3):149-207. https://doi.org/10.1177/1529100618760521
20. Vaccination programs: Community-based interventions implemented in combination. The Guide to Community Preventive Services (The Community Guide). Published February 25, 2015. https://www.thecommunityguide.org/findings/vaccination-programs-community-based-interventions-implemented-combination
21. What works fact sheet: Increasing appropriate vaccination. The Guide to Community Preventive Services (The Community Guide). Published October 15, 2021. https://www.thecommunityguide.org/resources/what-works-increasing-appropriate-vaccination
22. Schellenberg N, Crizzle AM. Vaccine hesitancy among parents of preschoolers in Canada: A systematic literature review. Can J Public Health Rev Can Sante Publique. 2020;111(4):562-584. https://doi.org/10.17269/s41997-020-00390-7
23. Wilson K, Sher G, Philpott J. Preparing for the next pandemic by creating Canadian Immunization Services. Can Med Assoc J. 2021;193(28):E1092-E1093. https://doi.org/10.1503/cmaj.210670
24. Musto R, Siever JE, Johnston JC, Seidel J, Rose MS, McNeil DA. Social equity in human papillomavirus vaccination: A natural experiment in Calgary Canada. BMC Public Health. 2013;13:640. https://doi.org/10.1186/1471-2458-13-640
25. Public Health Agency of Canada. Canada’s provincial and territorial routine (and catch-up) vaccination programs for infants and children.; 2016. https://healthycanadians.gc.ca/healthy-living-vie-saine/immunization-immunisation/schedule-calendrier/alt/infants-children-vaccination-enfants-nourrissons-eng.pdf
26. Oh NL, Biddell CB, Rhodes BE, Brewer NT. Provider communication and HPV vaccine uptake: A meta-analysis and systematic review. Prev Med. 2021;148:106554. https://doi.org/10.1016/j.ypmed.2021.106554
27. Shapiro GK, Tatar O, Amsel R, et al. Using an integrated conceptual framework to investigate parents’ HPV vaccine decision for their daughters and sons. Prev Med. 2018;116:203-210. https://doi.org/10.1016/j.ypmed.2018.09.017
28. Braun C, O’Leary ST. Recent advances in addressing vaccine hesitancy. Curr Opin Pediatr. 2020;32(4):601-609. https://doi.org/10.1097/MOP.0000000000000929
29. Cataldi JR, Kerns ME, O’Leary ST. Evidence-based strategies to increase vaccination uptake: A review. Curr Opin Pediatr. 2020;32(1):151-159. https://doi.org/10.1097/MOP.0000000000000843
30. CDC. How to talk with parents about COVID-19 vaccines. Centers for Disease Control and Prevention. Published October 13, 2021. https://www.cdc.gov/vaccines/covid-19/hcp/pediatrician.html
31. Canadian Paediatric Society. COVID-19 information and resources for paediatricians. Published 2021. https://www.cps.ca/en/tools-outils/covid-19-information-and-resources-for-paediatricians
32. Sabnis SS, Pomeranz AJ, Amateau MM. The effect of education, feedback, and provider prompts on the rate of missed vaccine opportunities in a community health center. Clin Pediatr (Phila). 2003;42(2):147-151. https://doi.org/10.1177/000992280304200208
33. Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents. JAMA Pediatr. 2014;168(1):76-82. https://doi.org/10.1001/jamapediatrics.2013.2752
34. Abdullahi LH, Kagina BM, Ndze VN, Hussey GD, Wiysonge CS. Improving vaccination uptake among adolescents. Cochrane Database Syst Rev. 2020;1:CD011895. https://doi.org/10.1002/14651858.CD011895.pub2
35. Atkinson KM, Mithani SS, Bell C, Rubens-Augustson T, Wilson K. The digital immunization system of the future: imagining a patient-centric, interoperable immunization information system. Ther Adv Vaccines Immunother. 2020;8:2515135520967203. https://doi.org/10.1177/2515135520967203
36. Canada PHA of. COVID-19 for health professionals: Training. Published February 15, 2021. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/training.html
37. Temerty Faculty of Medicine, University of Toronto. COVID-19 vaccination in Canada: An educational series for primary care professionals. Department of Family & Community Medicine. Published August 12, 2020. https://www.dfcm.utoronto.ca/covid19-vaccination-modules
38. Resources for healthcare workers. 19 to Zero. Published 2021. https://www.19tozero.ca/healthcare-worker-resources
39. Centre for Effective Practice. COVID-19: Vaccines. Published 2021. https://tools.cep.health/tool/covid-19-vaccines/
40. Partnering with primary care for local Covid-19 vaccine rollout in Ontario. Primary Care Collaborative; 2021. https://www.ontariofamilyphysicians.ca/tools-resources/covid-19-resources/covid-19-vaccines/partnering-primary-care-vax-rollout.pdf
41. Danchin M, Nolan T. A positive approach to parents with concerns about vaccination for the family physician. Aust Fam Physician. 2014;43(10):690-694. https://pubmed.ncbi.nlm.nih.gov/25286425/
42. Sanftenberg L, Kuehne F, Anraad C, Jung-Sievers C, Dreischulte T, Gensichen J. Assessing the impact of shared decision making processes on influenza vaccination rates in adult patients in outpatient care: A systematic review and meta-analysis. Vaccine. 2021;39(2):185-196. https://doi.org/10.1016/j.vaccine.2020.12.014
43. Gagneur A. Motivational interviewing: A powerful tool to address vaccine hesitancy. Can Commun Dis Rep Releve Mal Transm Au Can. 2020;46(4):93-97. https://doi.org/10.14745/ccdr.v46i04a06
44. Eze P, Lawani LO, Acharya Y. Short message service (SMS) reminders for childhood immunisation in low-income and middle-income countries: A systematic review and meta-analysis. BMJ Glob Health. 2021;6(7):e005035. https://doi.org/10.1136/bmjgh-2021-005035
45. Yunusa U, Garba SN, Umar AB, et al. Mobile phone reminders for enhancing uptake, completeness and timeliness of routine childhood immunization in low and middle income countries: A systematic review and meta-analysis. Vaccine. 2021;39(2):209-221. https://doi.org/10.1016/j.vaccine.2020.11.043
46. Linde DS, Korsholm M, Katanga J, Rasch V, Lundh A, Andersen MS. One-way SMS and healthcare outcomes in Africa: Systematic review of randomised trials with meta-analysis. PloS One. 2019;14(6):e0217485. https://doi.org/10.1371/journal.pone.0217485
47. Sondaal SFV, Browne JL, Amoakoh-Coleman M, et al. Assessing the effect of mHealth interventions in improving maternal and neonatal care in low- and middle-income countries: A systematic review. PloS One. 2016;11(5):e0154664. https://doi.org/10.1371/journal.pone.0154664
48. Chao C, Preciado M, Slezak J, Xu L. A randomized intervention of reminder letter for human papillomavirus vaccine series completion. J Adolesc Health Off Publ Soc Adolesc Med. 2015;56(1):85-90. https://doi.org/10.1016/j.jadohealth.2014.08.014
49. Vann JCJ, Jacobson RM, Coyne‐Beasley T, Asafu‐Adjei JK, Szilagyi PG. Patient reminder and recall interventions to improve immunization rates. Cochrane Database Syst Rev. 2018;(1). https://doi.org/10.1002/14651858.CD003941.pub3
50. Lott BE, Okusanya BO, Anderson EJ, et al. Interventions to increase uptake of human papillomavirus (HPV) vaccination in minority populations: A systematic review. Prev Med Rep. 2020;19:101163. https://doi.org/10.1016/j.pmedr.2020.101163
51. Szilagyi PG, Albertin C, Humiston SG, et al. A randomized trial of the effect of centralized reminder/recall on immunizations and preventive care visits for adolescents. Acad Pediatr. 2013;13(3):204-213. https://doi.org/10.1016/j.acap.2013.01.002
52. Gates A, Gates M, Rahman S, et al. A systematic review of factors that influence the acceptability of vaccines among Canadians. Vaccine. 2021;39(2):222-236. https://doi.org/10.1016/j.vaccine.2020.10.038
53. Kaufman J, Ryan R, Walsh L, et al. Face-to-face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst Rev. 2018;5:CD010038. https://doi.org/10.1002/14651858.CD010038.pub3
54. Suh CA, Saville A, Daley MF, et al. Effectiveness and net cost of reminder/recall for adolescent immunizations. Pediatrics. 2012;129(6):e1437-1445. https://doi.org/10.1542/peds.2011-1714
55. Rani U, Darabaner E, Seserman M, Bednarczyk RA, Shaw J. Public education interventions and uptake of human papillomavirus vaccine: A systematic review. J Public Health Manag Pract JPHMP. Published online November 16, 2020. https://doi.org/10.1097/PHH.0000000000001253
56. Flood T, Wilson IM, Prue G, McLaughlin M, Hughes CM. Impact of school-based educational interventions in middle adolescent populations (15-17yrs) on human papillomavirus (HPV) vaccination uptake and perceptions/knowledge of HPV and its associated cancers: A systematic review. Prev Med. 2020;139:106168. https://doi.org/10.1016/j.ypmed.2020.106168
57. Deardorff KV, Rubin Means A, Ásbjörnsdóttir KH, Walson J. Strategies to improve treatment coverage in community-based public health programs: A systematic review of the literature. PLoS Negl Trop Dis. 2018;12(2):e0006211. https://doi.org/10.1371/journal.pntd.0006211
58. Oyo-Ita A, Wiysonge CS, Oringanje C, Nwachukwu CE, Oduwole O, Meremikwu MM. Interventions for improving coverage of childhood immunisation in low- and middle-income countries. Cochrane Database Syst Rev. 2016;7:CD008145. https://doi.org/10.1002/14651858.CD008145.pub3
59. Glenton C, Scheel IB, Lewin S, Swingler GH. Can lay health workers increase the uptake of childhood immunisation? Systematic review and typology. Trop Med Int Health TM IH. 2011;16(9):1044-1053. https://doi.org/10.1111/j.1365-3156.2011.02813.x
60. Crawshaw J, Konnyu K, Castillo G, et al. Factors affecting COVID-19 vaccination acceptance and uptake among the general public: A living behavioural science evidence synthesis (v5, Aug 31st, 2021).; 2021:75. https://www.mcmasterforum.org/docs/default-source/product-documents/living-evidence-syntheses/covid-19-living-evidence-synthesis-4.5—factors-affecting-covid-19-vaccination-acceptance-and-uptake-among-the-general-public.pdf?sfvrsn=33dc4261_5
61. The National Collaborating Centre for Methods and Tools. Rapid review: What is known about parents’ considerations for vaccine uptake for children and adolescents?; 2021. https://www.nccmt.ca/covid-19/covid-19-rapid-evidence-service/37
62. Fu LY, Haimowitz R, Thompson D. Community members trusted by African American parents for vaccine advice. Hum Vaccines Immunother. 2019;15(7-8):1715-1722. https://doi.org/10.1080/21645515.2019.1581553
63. Fu LY, Zimet GD, Latkin CA, Joseph JG. Social networks for human papillomavirus vaccine advice among African American parents. J Adolesc Health Off Publ Soc Adolesc Med. 2019;65(1):124-129. https://doi.org/10.1016/j.jadohealth.2019.01.029
64. Konstantinou P, Georgiou K, Kumar N, et al. Transmission of vaccination attitudes and uptake based on social contagion theory: A scoping review. Vaccines. 2021;9(6):607. https://doi.org/10.3390/vaccines9060607
65. Public Health Association of BC. Kids boost immunity. Kids Boost Immunity. Published 2021. https://kidsboostimmunity.com/front-page
66. Rotenberg S, Downer MB, Brown H, et al. COVID-19 vaccination for people with disabilities. Sci Briefs Ont COVID-19 Sci Advis Table. 2021;2(35). https://doi.org/10.47326/ocsat.2021.02.35.1.0
67. Canadian Paediatric Society. COVID-19 and Indigenous children in Canada: What can paediatricans do? Published May 27, 2020. https://www.cps.ca/en/blog-blogue/covid-19-indigenous-children-in-canada-what-can-paediatricans-do
68. City of Toronto. COVID-19 guidance: Faith-based organizations. City of Toronto. Published July 18, 2020. https://www.toronto.ca/home/covid-19/covid-19-reopening-recovery-rebuild/covid-19-reopening-guidelines-for-businesses-organizations/covid-19-guidance-faith-based-organizations/
69. A patient-oriented research program in children’s pain management. It Doesn’t Have to Hurt. Published 2021. https://itdoesnthavetohurt.ca/resources/
70. Solutions for Kids in Pain. Needle pain & vaccine fear / Douleur et peur des aiguilles & vaccin. Solutions for Kids in Pain (SKIP). Published 2021. https://kidsinpain.ca/category/skipresources/covidresources/page/2/
Document Information & Citation
Author Contributions: GKS, LD, JP conceived the Science Brief. GKS, AW, JP wrote the first draft of the Science Brief. All authors revised the Science Brief critically for important intellectual content and approved the final version.
The authors would like to thank Dr. Noah Ivers for sharing resources developed to help primary care physicians and staff address questions and hesitancy in parents for the paediatric COVID-19 vaccines.
Citation: Shapiro GK, Presseau J, Weerasinghe A, et al. Behavioural science-informed strategies for increasing COVID-19 vaccine uptake in children and youth. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;2(50). https://doi.org/10.47326/ocsat.2021.02.50.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners can be found at https://covid19-sciencetable.ca/. The declarations of interest of external authors can be found under Additional Resources.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners.
