Key Message
Primary care is a crucial component of pandemic and health emergency preparedness, response, and recovery. It is also essential to continued health system improvement, person-centred care in communities, and optimal population health for Ontarians. A capacity crisis in primary care has deepened during the COVID-19 pandemic. Urgent efforts are needed to address the factors that limit primary care provision. This will include ensuring an infrastructure that supports coordinated and integrated primary care. It will also include ensuring the training, support, and retention of interdisciplinary health human resources (HHR) that comprise teams providing care associated with patient enrolment models (PEMs), so they are equitable and accessible for all Ontarians before, during, and after public health emergencies.
Summary
Background
More than two years of ongoing COVID-19 response has changed the practice and capacity of primary care in Ontario. These changes have important implications that impact ongoing response and recovery. During the COVID-19 pandemic, preventive and ongoing care have been deferred and delayed for multiple reasons, causing patients to present later to primary care with greater acuity and complexity. Managing these increasingly complex care needs falls on primary care clinicians (PCCs) as increasing wait times for tests, procedures, and specialized care further contribute to the erosion of primary care capacity. COVID-19 has added stress to a system already experiencing considerable strain, with longstanding pressures and intersecting factors undermining the quality of primary care in Ontario. Understanding the most pressing factors that currently limit primary care provision in Ontario requires an exploration of three key critical domains – health human resources (HHR), models of care, and infrastructure for coordinated and integrated care – that shape the way primary care is delivered by PCCs, and that have been affected by the COVID-19 pandemic.
Questions
In what ways do current trends in HHR for primary care affect primary care provision?
In what ways can different models of primary care support pandemic response and recovery?
How can infrastructure support coordinated and integrated primary care moving forward?
Findings
Primary care is facing an accelerating capacity crisis driven by limited HHR, varying models of care delivery, and an information and communication infrastructure that is inadequate to support the coordination of care and the integration of primary care with other health (including public health) and social services. Important trends affecting primary care HHR capacity include the growing and aging population, changing physician demographics, impending retirements, shifts away from comprehensive family practice, and burnout across PCC professions. A lack of PCCs across the health professions that work in primary care threatens the success of Family Health Teams (FHTs), which have proven to be an important model of primary care in Ontario. Patient enrolment models (PEMs) that formally attach patients to a regular primary care source, patient attachment to interprofessional teams, and practice variation have been important determinants of access, continuity, and outcomes throughout the COVID-19 pandemic with implications for primary care capacity moving forward. Support for coordinated and integrated primary care in Ontario is a pressing need; however, currently, there is no governance model, accountability framework, or overarching system to provide that support. Further, high-quality primary care provision in Ontario will require more equitable, coordinated, and integrated collection and use of data to inform both pandemic responses and health system improvements. These complex factors, coupled with and amplified by longstanding health system challenges, pose an ongoing threat not only to a coordinated pandemic response but to routine health system functioning, quality, and future pandemic preparedness.
Interpretation
Primary care is crucial to ongoing pandemic preparedness, response, and recovery. As the capacity crisis in primary care deepens and demand continues to increase, there is a pressing need to address the factors that limit primary care provision before, during, and after pandemics. This requires training, supporting, and retaining the interdisciplinary HHR that comprises team-based models of care. It also requires supporting PEMs that are effective, equitable, and accessible to all Ontarians, aligned with the Quadruple Aim outlined in Ontario Health’s Vision for Health Care in Ontario: improving the patient and caregiver experience, improving the health of populations, reducing the per capita cost of health care, and improving the work life of clinicians. Collaborative, cross-sectoral efforts based on existing relationships will be key to strengthening primary care. PEMs, patient attachment to team-based models of care, and practice variation have been important determinants of access, continuity, and outcomes throughout the COVID-19 pandemic. Addressing the issues that limit these will continue to be crucial to addressing gaps in care during recovery and for future preparedness. More coordinated and integrated care in Ontario will also require more coordinated and integrated collection and use of data to drive both pandemic responses and health system improvements. Health systems with stronger primary care have better population health outcomes, improved health equity, and lower overall costs. Addressing the significant primary care capacity gaps described in this Brief will not only result in better population outcomes but will also strengthen pandemic preparedness, response, and recovery in Ontario.
Full Text
Background
Primary care offers a critical entry point into both COVID-19 and non-COVID-19-related care, and health systems around the world with strong primary care achieve better health outcomes and improved health equity at lower cost.1–3 Primary care clinicians (PCCs) have played an integral and varied role in the pandemic response in Ontario. More than two years of ongoing COVID-19 response have changed the practice and capacity of primary care in Ontario. These changes have important implications that impact ongoing response and recovery.
During the COVID-19 pandemic, some preventive and ongoing services have been deferred or delayed. This has led to people presenting to primary care later, with multiple acute and chronic concerns, a high level of mental health comorbidity, substance use, and worsening of major mental illness.4 Navigation of our complex health system, often coordinated by PCCs, is needed for patients who require tests, procedures, and specialist consultation, which in turn have become more difficult to access.5 While patients await access to or are discharged from more specialized care, the management of increasingly complex care needs falls largely to PCCs. This increases stress among primary care patients and their PCCs, adds to workload and the complexity of that workload, and erodes primary care capacity and, in turn, access to care for all patients.6 At the same time, accessibility to primary care physicians for comprehensive care may have been reduced during the pandemic due to reduced clinical service hours among some physicians and a shift towards virtual care, including among a very small subset of physicians who went to a nearly entirely virtual model.7
The shift toward increasing complexity is occurring while PCCs have been playing a key role in pandemic response, and against a further-reaching background of increasing workload and complexity pre-pandemic. Preliminary results from the early-career primary care (ECPC) study found that in British Columbia, the per-visit workload for community-based family physicians has gone up by 35-50% (1999/00 to 2017/18) based on prescriptions, referrals, and investigations generated by each visit.8,9 It is important to note that the support for PCCs varies significantly geographically. The average specialist to family physician ratio in Ontario is 1:1, but in several regions, including the North, the ratio is significantly smaller, meaning family physicians are likely managing a significantly greater degree of complexity without ready access to specialists than is the case in the rest of the province.10
Understanding the most pressing factors that currently limit primary care provision in Ontario requires an exploration of three key critical domains that shape the way primary care is delivered by PCCs, and that have been affected by the COVID-19 pandemic: health human resources (HHR), primary care practice structures (models), and health system infrastructure for integrated and coordinated care. In this context, PCCs refer primarily to family physicians/general practitioners and primary care nurse practitioners. PCCs also include nurses, physician assistants, pharmacists, social workers, and other interprofessional health care providers working in primary care teams in Ontario. In this Brief, we explore HHR trends that affect the provision of primary care, challenges, and opportunities in different models of primary care provision, and the infrastructure needed to support integrated and coordinated care.
Questions
In what ways do current trends in HHR for primary care affect primary care provision?
In what ways can different models of primary care support pandemic response and recovery?
How can infrastructure support coordinated and integrated primary care moving forward?
Findings
In What Ways Do Current Trends in Health Human Resources (HHR) For Primary Care Affect Primary Care Provision?
Ontario’s growing, multimorbid, and aging population needs increased access to primary care, but this demand cannot be met by current numbers of PCCs.11,12 Shifting physician demographics, impending retirements, shifts away from comprehensive family practice, limited service provision by some PCCs during the pandemic, and burnout across PCCs pose an accelerating threat to the provision of primary care in Ontario. On the other hand, the COVID-19 pandemic brought to the forefront collaborations and initiatives amongst PCCs across Ontario and Canada related to equity, diversity, and inclusion in both medical education and practice that are likely to shape primary care provision in the future.
In keeping with national labour and demographic trends,13 Ontario’s family physician workforce is aging, with an increasing proportion of Ontario family physicians nearing retirement. As of 2019, 1.7 million Ontarians were attached to a family physician aged 65 years or older.14,15 This is more than double the proportion of Ontarians who were attached to family physicians in this age group in 2008. In the context of previous research on the average retirement age of an Ontario family physician (70.5 years old), these 1.7 million Ontarians may lose their family physician to retirement by 2025.16
Yet these figures are likely underestimates. An average retirement age of 70.5 years old is based on a study period from 1992-2013 when the workforce was predominantly male.16 The same study found that women family physicians retire approximately five years sooner than their male counterparts. With the 2019 workforce at a 50/50 male to female ratio, the retirement age (pre-pandemic) may therefore be closer to 65 years.15Second, the pandemic appears to have hastened retirements. Three percent of family physicians ceased clinical work entirely during the pandemic, an almost doubling of the usual rate of 1.6% per year.7
In addition, an increasing proportion of Ontario family physicians in every age group and at every career stage is shifting away from comprehensive practice and into focused scopes of practice (such as emergency medicine, sports medicine, palliative care, and more). “Comprehensive practice” is the provision of a broad range of services on a longitudinal basis to a defined panel of patients of all ages, backgrounds, and health conditions.17,18 Comprehensive care is the type of primary care that is most strongly associated with better health outcomes and lower health system costs.1,18–23 As a result of shifts away from comprehensiveness, the overall proportion of Ontario family physicians providing this type of care has dropped from 77.2% in 2008 to 70.7% in 2019.15
Further exacerbating these challenges is the declining proportion of graduating medical students ranking family medicine as their first choice of specialty when applying to residency. Among Ontario graduates, the Canadian Resident Matching Service (CaRMS) has reported a decline from 40.2% in 2015 to 33.3% in 2022, and among Canadian graduates, a decline from 38.5% (2015) to 30.7% (2022) – the lowest since 2008.24
The reasons for shifts away from comprehensive primary care are numerous and complex. Early results from Canadian research have shown they include:9,25
- Lack of the interprofessional team-based supports necessary to respond to trends in older patient age, increasing patient complexity independent of age, and increasing complexity in managing chronic diseases.
- Lack of administrative and operational supports, with the costs and time commitments of running a business seen as drawbacks by many new physicians who would prefer to focus on patient care.
- Difficulty accessing predictable forms of compensation, particularly in provinces that remain predominantly “fee-for-service” (pay-per-visit) in their physician payment structures. This is especially a consideration given that 45% of new graduates carry over $100,000 in medical school debt in addition to their undergraduate education debt, which is, on average, $28,000.26,27
Additionally, the pandemic appears to have exacerbated burnout rates across all physician groups, including family physicians. Earlier this year, the College of Family Physicians Canada (CFPC) reported that the rate of burnout among family physicians tripled in 2021 compared with the previous year, with 51% of family physicians indicating they were working beyond capacity.28 The Canadian Medical Association’s 2021 survey found family physicians are disproportionately negatively impacted by administrative burdens, with nearly half (45%) of all family physicians surveyed in 2021 spending, on average, 10-19 hours per week on administrative tasks (i.e., between one and two full work days), compared with 33% of medical specialists, 37% of surgical specialists, and 32% of other physicians/administrators.29
In the pandemic, most COVID-19 infections have been diagnosed and managed in the community. During that time, beyond ongoing primary care services for their patients, family physicians have taken on multiple roles, including managing infections in the office and through remote care; supporting public health (e.g., by staffing assessment and vaccination centres); providing surge capacity in acute care settings; and supporting outreach to equity-deserving populations.30 In the later and ongoing stages of the pandemic, there has been extraordinary pressure to keep emergency departments (EDs) open. To this end, in many rural communities, family physicians practicing in the local primary care practice also provide ED services. Many rural family physicians have been asked to prioritize the ED and forego their offices to keep EDs open, further impacting workload and primary care delivery in many rural settings (Sarah Newbery, personal communication).
Also of concern is that 21.9% of Ontario nurses in primary care report an intention to retire within four years.31,32 Based on the unfilled positions in Family Health Teams (FHTs) for nursing and other interprofessional health care providers, the declining interest in comprehensive primary care likely extends beyond the physician workforce, signaling a need for a comprehensive approach to address shortages in all areas of HHR in the primary care sector (Kavita Mehta, personal communication).
In What Ways Can Different Models of Primary Care Support Pandemic Response and Recovery?
Health systems with stronger primary care have better population health outcomes, and evidence indicates this is likely facilitated by a core set of mechanisms commonly termed “the Four C’s”: first contact, continuity, comprehensiveness, and coordination.33 Models of care, or the way in which health services are organized and delivered, are important for realizing these “Four C’s”. Although there is limited research available, this Brief discusses how patient enrolment models (PEMs) that formally attach patients to a regular source of primary care, patient attachment to team-based models of care, and inter-physician practice variations, have been important determinants of access, continuity, and outcomes throughout the COVID-19 pandemic, with implications for primary care capacity moving forward.
In Ontario, there are many practice models. These range from solo, fee-for-service physicians to team-based, capitated FHTs, community-governed Community Health Centres (CHCs), Nurse Practitioner-led clinics (NPLCs), and various other models. There is no easily accessible central registry of PCCs or clinics in Ontario, which impairs communications to and between PCCs. There are also no clear governance structures at the regional level, although this may be addressed by the emerging structure of Ontario Health Teams (OHTs), where groups of clinicians and organizations aim to become clinically and fiscally accountable for delivering care to a defined geographic population.34 Ontario’s current fragmented primary care landscape stands in contrast to greater coordination across the sector in other Canadian jurisdictions, such as Alberta, and in many international comparators, such as the UK, the Netherlands, and Australia, which perform well on both established primary care quality indices (e.g., access to health care, person-centred care, coordination of care, and cost barriers to care), and on pandemic indices (e.g., policy and vaccination).35–43 While these realities pre-date the pandemic, they have also shaped the primary care response and have important future implications.37
Patient Enrolment Model (PEM) And Continuity of Care
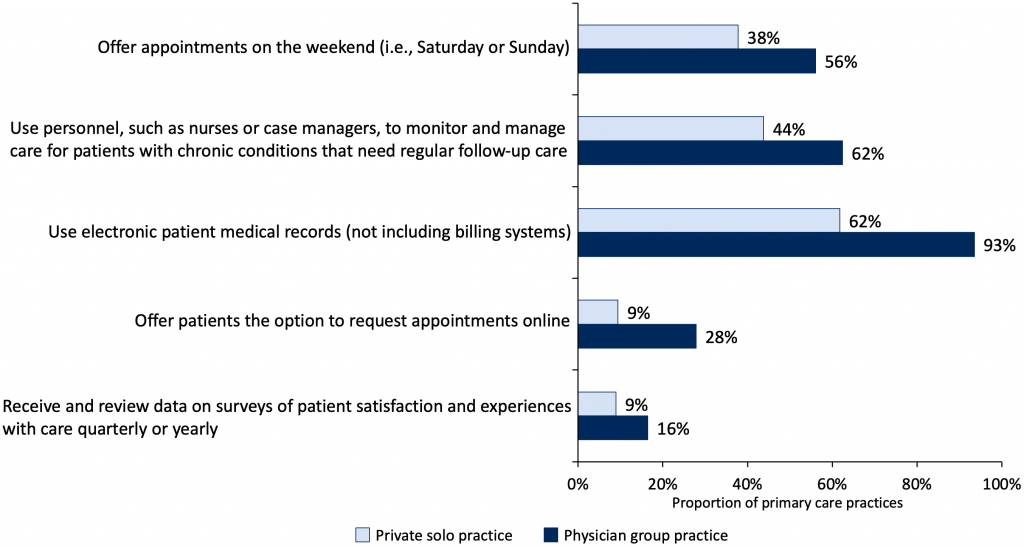
Continuity of care with a primary care professional or team is associated with improved access, better preventive care, decreased utilization, decreased health care costs, improved health, decreased mortality, and improved patient satisfaction.44 Continuity of care can also foster more person-centred care, including greater trust and confidence in a person’s medical care, as well as joy and meaning in a clinician’s work.45 In the Ontario context, a PEM is a model in which there is a formal relationship attaching the patient to a PCC (“rostering”). In most PEMs, primary care physicians work in groups which have some accountability for after-hours access. Overall, evidence indicates physicians participating in group practices such as PEMs are more likely to offer after-hours appointments, use an electronic medical record (EMR), and participate in quality improvement initiatives (Figure 1).43
During the pandemic, formal attachment has been protective of continuity, whereas patients without a formal attachment were less likely to experience continuity.46 Visits to one’s own PCC remained high for people rostered to a PEM but declined significantly for people not formally rostered, including both office and virtual visits.46
Possible reasons for the decline in continuity for people loosely attached to primary care might include greater availability of virtual care through episodic providers (virtual “walk-in” clinics). This raises concerns about fragmented care, duplication of services, and lack of relational and informational continuity. In addition, patients not enrolled in a PEM are more likely to be low-income, urban, new immigrants, and have more complex health and social needs that appear, based on care quality indicators, more difficult to meet without the support of interprofessional teams; in Ontario, however, interprofessional teams are only available to patients in PEMs.47
Given the HHR constraints described above, the ability of Ontario’s primary care sector to support universal attachment is limited by a mismatch between the size and distribution of the workforce and population needs. As of 2020, nearly 1.8 million people are either completely unattached or only loosely connected to a regular primary care source.48 The needs are not equitably distributed, with particular challenges experienced by structurally marginalized populations. For example, a lower proportion of new immigrants are attached to a PCC compared to those who are not new immigrants (77.5% vs 88.2%), fewer Ontarians in the lowest income quintile are attached compared to those in the highest (83.9% vs 89.9%), and fewer with the highest degree of family or housing instability (residential instability) are attached compared to those with the lowest level of residential instability (83.8% vs. 90.3%) (Table 1).48 Further, attachment rates are expected to fall due to trends outlined above in the primary care workforce. In addition, population growth and disproportionate geographic and social determinant of health disparities in COVID-19-related burden49–51 may create further challenges attaching patients to primary care.
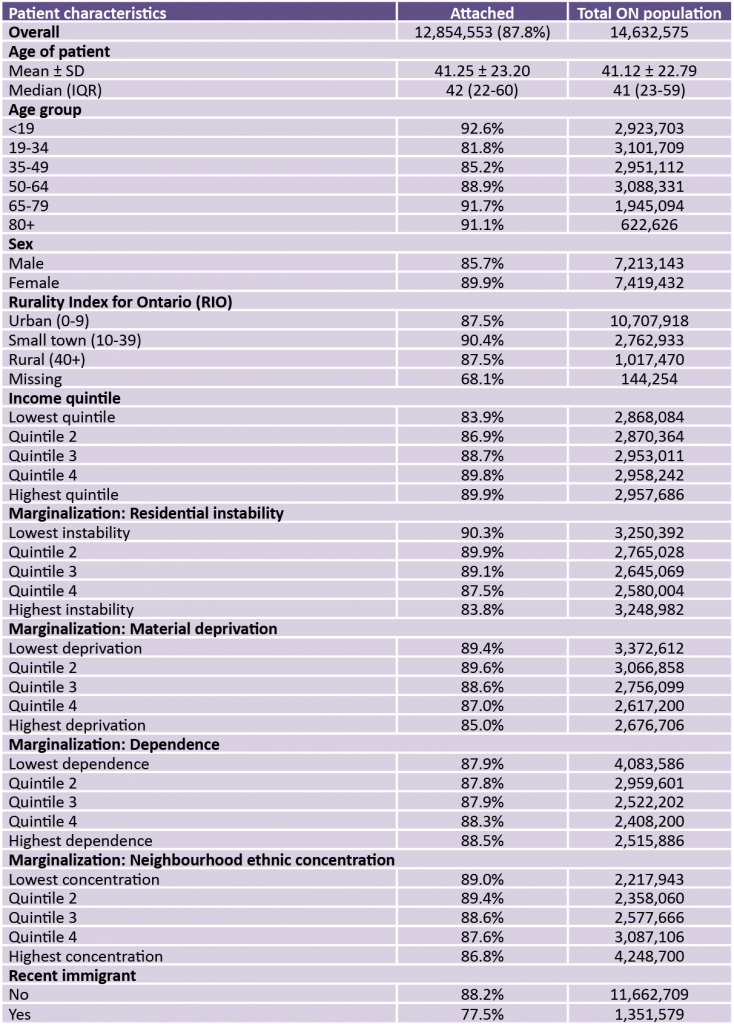
Attachment rates calculated using the methods described in https://inspire-phc.org/.52 This may produce different results than other methods for calculating attachment. Adapted from Green et al.48 These data include attachments to primary care pediatricians. ON, Ontario.
Access to Team-Based Primary Care Models
Team-based care builds on the concept of the PEM. In a team, as with a PEM, the patient is formally attached to a regular source of primary care. In addition, primary care teams include interprofessional health care providers (e.g., nurse practitioners, nurses, physician assistants, social workers, dietitians, pharmacists, physiotherapists, occupational therapists, etc.) who collaborate with primary care physicians to serve patients’ health and social needs. Evidence indicates that health care teams, aligned to the needs of the population (the “medical home”) and networked/integrated within the health system, support the best health outcomes.53 The mechanism is likely the enhancement of the “comprehensiveness” described in the “four C’s”.33 Prior to the pandemic, these benefits were contested in some Ontario models. While an early evaluation of team-based care (the FHT model) suggested few benefits,54 a more recent review conducted by a third party for the Ministry of Health found that FHTs improved patient and clinician experience and improved quality of care (better after-hours access, better quality, and cost neutral).55 A systematic review of CHCs, another team-based model used in Ontario, found that they provide care for a large socially and clinically complex population and that overall, they consistently demonstrate superior chronic disease management, patient experience, and provider/team satisfaction, as well as fewer emergency room visits than expected.56
The benefits associated with team-based care have been prominent throughout the pandemic. As described in detail in part 1 of this Ontario Science Table Brief,57 throughout COVID-19, teams have inherently had the flexibility and interprofessional resources to meet their patients’ and communities’ needs to a greater extent than have non-team-based primary care practices. This has included the redeployment of staff to perform outreach services to people with greater needs, such as those experiencing mental illness and homelessness, and the redesign of health promotion and social support programs to ensure their ongoing availability to the community at large. It has also included the provision of effective remote and in-person care for symptomatic COVID-19 patients and participation in regional planning efforts.57,58
In view of the evidence to date on the benefits of teams, the increasingly complex needs of Ontario’s aging patient population, and rising concerns around the added strain of the possible long-term, disabling effects of COVID-19,59 it seems clear that teams will play a key role in pandemic recovery, future preparedness, and ongoing health system functioning. Despite this, the availability of teams in Ontario remains persistently low. In general, Canadian primary care physicians are less likely than physicians in other countries to work in interprofessional models. Ontario is on the low end of Canadian jurisdictions for the proportion of primary care physicians who use personnel, such as nurses or case managers, to monitor and manage care of patients with chronic conditions that need regular follow-up care (Figure 2).43 Across Canada, the proportion of physicians in solo practice varies from 9% to 25%; at 17%, Ontario is in line with the average.
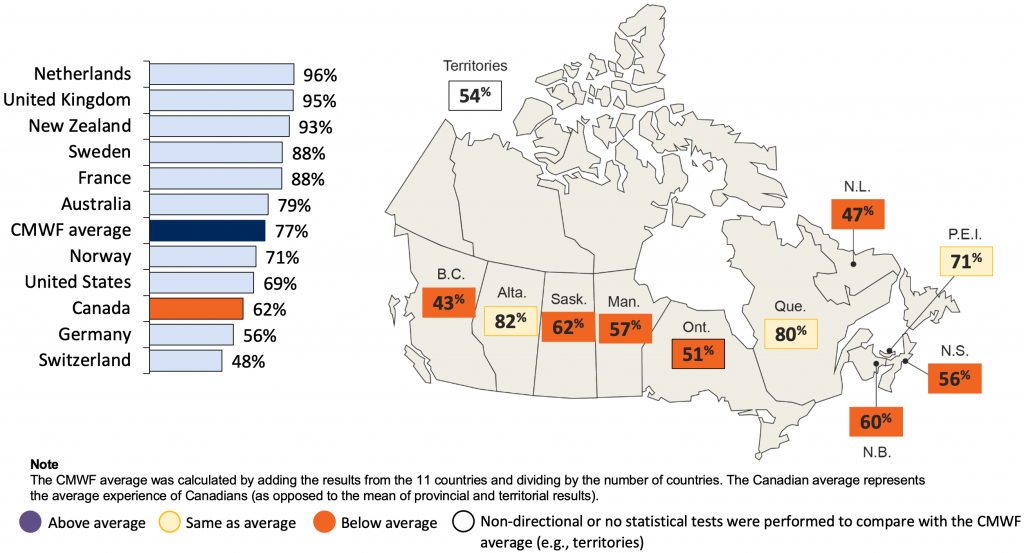
Fewer Canadian Primary Care Physicians Use Personnel to Care for Patients with Chronic Conditions Compared with Commonwealth Fund (CMWF) Average.43
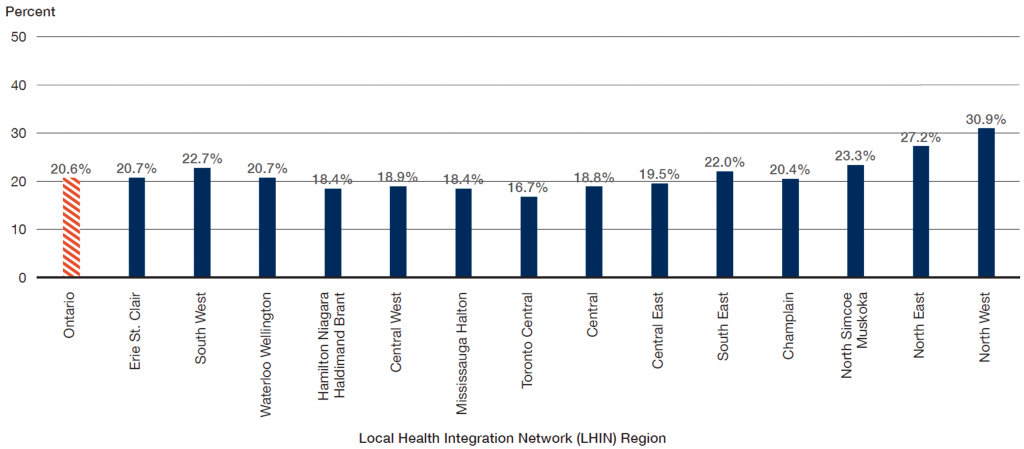
Within the context of the general trend towards teams, team composition in Ontario has been variable in terms of team size, membership, funding models and structure, and allocation to populations who will benefit the most. Ontario currently has 101 CHCs, 25 NPLCs, 184 FHTs (72 rural and 44 Northern) and 10 Aboriginal Health Access Centres.60–63 The vast majority of team-based care in Ontario is delivered by FHTs, who serve approximately 3.4 million Ontarians,61 or less than 25% of the population. As is the case for attachment in general, access to teams is inequitably distributed in Ontario and does not align with needs. Patients living in urban areas, new immigrants, and sicker patients are less likely to be in an FHT.47,51,64 Figure 3, which depicts patient attachment to a FHT based on their local OHT catchment area, demonstrates that access to team-based care is highly dependent upon where one lives.
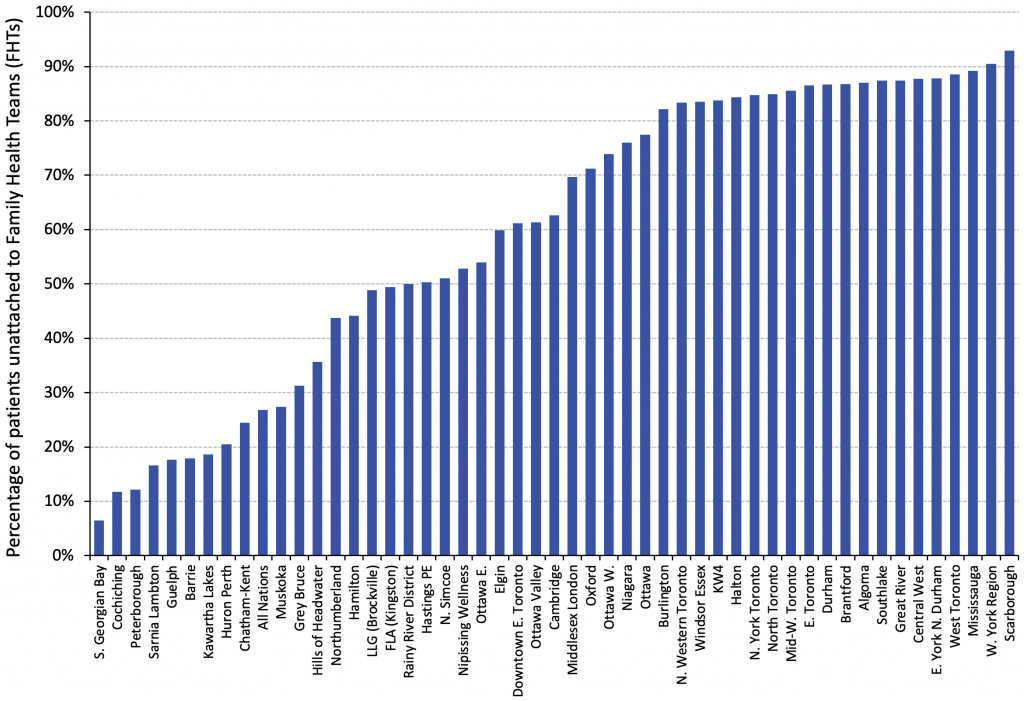
Ontario’s ability to meet its primary care HHR needs during the recovery phase of the pandemic will depend, to some extent, on PCCs’ ability to work in team-based models of care. Access to teams is likely to be a determining factor in medical students’ decision to enter the specialty of family medicine, practicing physicians’ decision to provide comprehensive primary care, and the ability to retain PCCs in the coming decade. Longitudinal data indicates an increasing preference among family physicians of all age groups to practice in team-based models of care.15 Capitation models provide income security and better align payment with the principles of continuity and comprehensiveness compared to fee-for-service models.65
FHT-based models also support interprofessional PCCs to help physicians manage increasingly complex patient care.53 These models also represent the practice environment in which medical students and residents learn the required competency of collaborative, team-based care as part of their family medicine training.66Newer primary care models (capitation models with or without team-based care, i.e., not fee-for-service) are associated with lower total health care costs for patients compared to the traditional fee-for-service model, despite higher primary care costs in some models.67 This adds to national and international literature supporting investment in primary care as a means to reduce overall health system spending.1,68 Recent Ontario data also suggests that primary care teams have led to reductions in ED use, which may be a surrogate for improved chronic disease management, as suggested by data finding that team-based care improved diabetes care.54 Similar effects of team-based care on reducing ED use have been seen in other provinces.20,69,70
Work satisfaction, examined separately from financial satisfaction, has also been found to be higher among family physicians working in non-fee-for-service settings, a finding that is highly relevant to HHR recruitment and retention.71 Further work is needed to determine the optimal model (roles, composition, and teamwork) that best aligns with the Quadruple Aim in Ontario Health’s Vision for Health Care in Ontario; that is, improving the patient and caregiver experience, improving the health of populations, reducing the per capita cost of health care, and improving the work life of clinicians.72 All of these factors will have important effects on primary care capacity.
In early 2015, limitations were introduced that reduced eligibility for physicians to enter capitation models.73Although Ontario recently loosened these restrictions,74 there remain logistical requirements, such as group co-location, that may impede entry in some communities, particularly for physicians where operational considerations (e.g., existing building leases) affect their mobility. Further, insufficient team-based care remains unaddressed, with no significant expansion of FHT numbers since fiscal year 2011/12.61 The result is that substantial segments of the workforce and their patients remain in non-capitation, non-team-based models, unable to access the range of benefits of team-based care during the pandemic that are described above and in part 1 of this Brief. These patients, who have experienced inequitable care during the pandemic, are equally vulnerable to care inequities during the recovery phase and in future pandemics and emergencies. Of imminent concern is that non-capitation, non-team-based models include 47% of the comprehensive family physicians aged 65 years or older. This proportion of older physicians corresponds to 761,648 patients15 and the trends in care model preference outlined above indicate new graduates may not be willing to take over these near-retirement physicians’ practices, a need which will likely occur during the recovery phase of the pandemic.
Practice Variation
There is a high level of variation in the quality of care provided within the primary care sector. In the case of virtual care in the pandemic, there has been a high degree of variation across all care models, and the proportion of virtual care also varied over time, with higher proportions coinciding with higher COVID-19 case counts in the community.75 Some Ontario family physicians have done almost no virtual care, while others have maintained extremely high levels of virtual practice. This variation occurs primarily at the level of the individual physician and the physician’s practice, rather than by model of care.75 As discussed in part 1 of this Brief, a very small number of family physicians shifted their practices entirely to virtual care. Between Feb and Oct 2021, 400 family physicians (2.6%) had 100% of visits that were virtual; this included physicians in focused practice, such as general practitioner (GP) psychotherapists.75
Further detailed data on virtual care is provided in part 1 of this Ontario Science Table Brief.57 As discussed in that section of the Brief, the ideal proportion of virtual care in primary care is unknown. Family physicians who provided a higher proportion of virtual care did not have higher ED visit rates among their patients compared to those who provided less virtual care overall.75 Models of “virtual-only” care provided by corporate entities that have grown in the pandemic and are uncoupled from continuity of care, however, require evaluation to understand their impacts on patients and health system outcomes, including costs. Compared to Ontarians having any virtual family physician visit, virtual “walk-in” patients were significantly more likely to have a subsequent virtual visit (30.3% vs. 21.9%, standardized mean difference = 0.19) and twice as likely to have an emergency department visit within 30 days.76
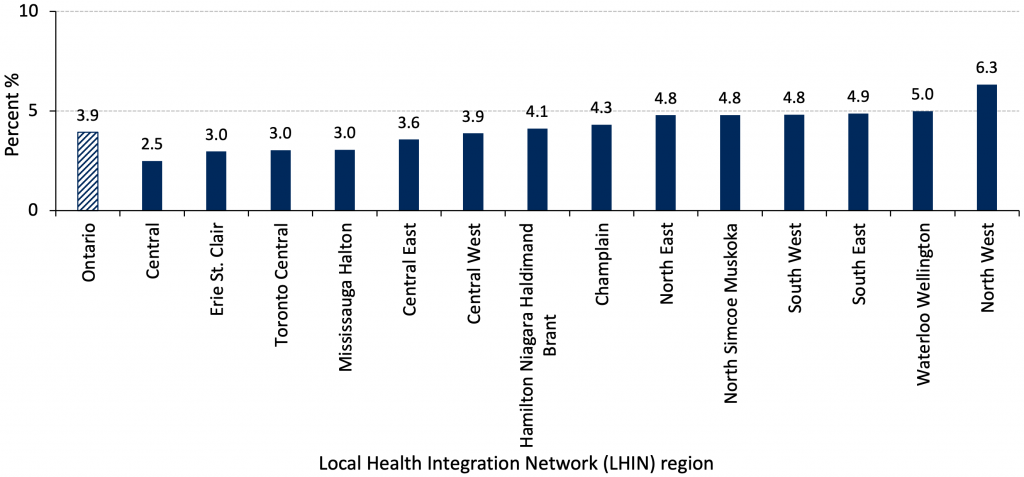
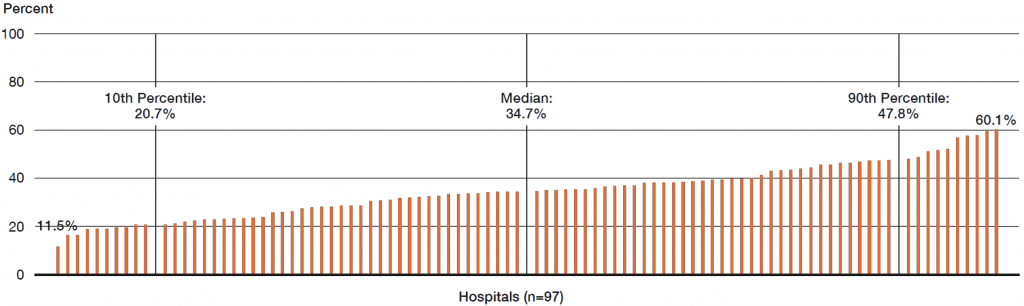
These findings around virtual care practice variation are consistent with previous work on primary care quality variation in Ontario. For example, in 2019, the proportion of people able to access a same-day or next-day appointment with their PCC ranged from 19.1% in the North East of the province to 49.5% in Central West.77Many other quality metrics likewise show a high degree of variation. For example, in 2019, the percentage of people aged 16 and older who reported that their PCC always or often involves them in decisions regarding their care ranges from 74.6% to 94.1%, and the rate of serious complications among people living with diabetes ranges from 3.57 per 1000 to 6.67 per 1000.78,79 While there are many factors that might contribute to these variations in outcomes, some of which are outside the control of the primary care team, unwanted variation is an obvious target for quality improvement efforts, which requires data, feedback, and quality improvement infrastructure and supports.80–82 Figure 483–85 below depicts care variations across common conditions managed in primary care in Ontario (depression/anxiety; diabetes; asthma; chronic obstructive pulmonary disease), both across geography and income. Patients with these conditions are at increased risk of complications from COVID-19 infection compared to the general population,86 and are more susceptible to the effects of delayed or deferred care during the pandemic as well as care inequity. Indeed, in Ontario primary care patients, multimorbidity is significantly associated with both frailty and lower socio-economic status.87,88Achieving consistently high quality of care for these patients must therefore be an important feature of ongoing pandemic response and recovery.
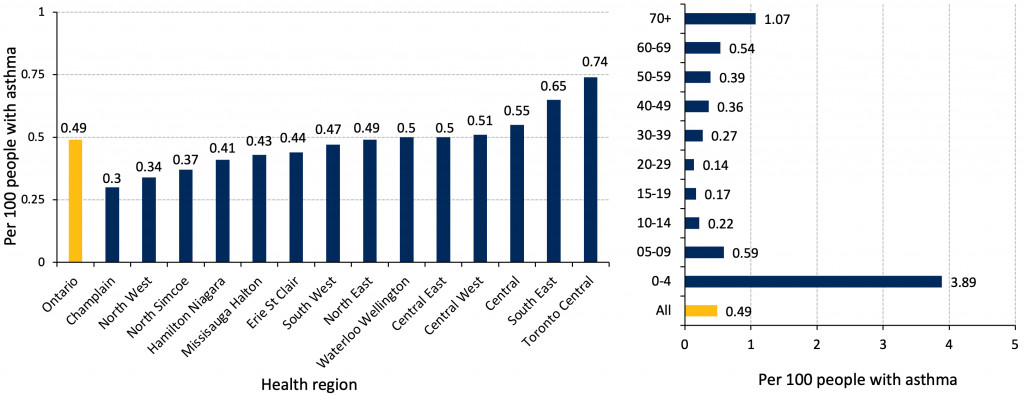
*Data for 2018 may be incomplete due to the two-year algorithm to identify asthma, and numbers are subject to change.
How Can Infrastructure Support Coordinated and Integrated Primary Care Moving Forward?
Ontario does not have a coordinated primary care “system.” It is a sector with thousands of independent practices which, over time, have become increasingly disintegrated from the acute care sector.47 Canadian programs of research and policy documents in Ontario support more active, explicit integration between primary care and public health, and emphasize the need for greater connection between primary care and the acute care sector.89–91 A report on the integration of care by the Kings Fund states that success depends on relationships: “a really effective system is all about building relationships, trust, knowledge and confidence in one another”.92 Research focused on integration between primary care and hospitals likewise states that “integration is about relationships between people”.93,94 Canada’s experience during the pandemic has also shown that integration of care extends beyond primary care offices and hospitals to communities, particularly where there is a higher risk of transmission of the SARS-COV-2 virus. Value-based care and relationship-building are particularly important in reaching structurally marginalized communities with long-rooted historical racism and lived experiences in health care causing mistrust.95,96
The Canadian health care system exhibited extensive resource mobilization and rapid integration efforts during the pandemic, including collaborative teamwork to support testing, treatment, and vaccination in First Nations, Inuit, and Metis (FNIM) communities, Black communities and other groups experiencing structural marginalization. Collaborations led by community leaders, CHCs, and allies across the health system led to the use of culturally safe approaches that were successful in engaging communities.97–101 Moreover, PCC collaborations with and learning from FNIM and Black community leaders informed continuing professional development, medical education, and academic teaching related to the pandemic response.102 However,continuing barriers to integrated systems, coupled with data limitations on COVID-19 outcomes in equity-deserving communities, continue to pose challenges to both coordinated pandemic response and routine health system functioning.
Health Systems Infrastructure
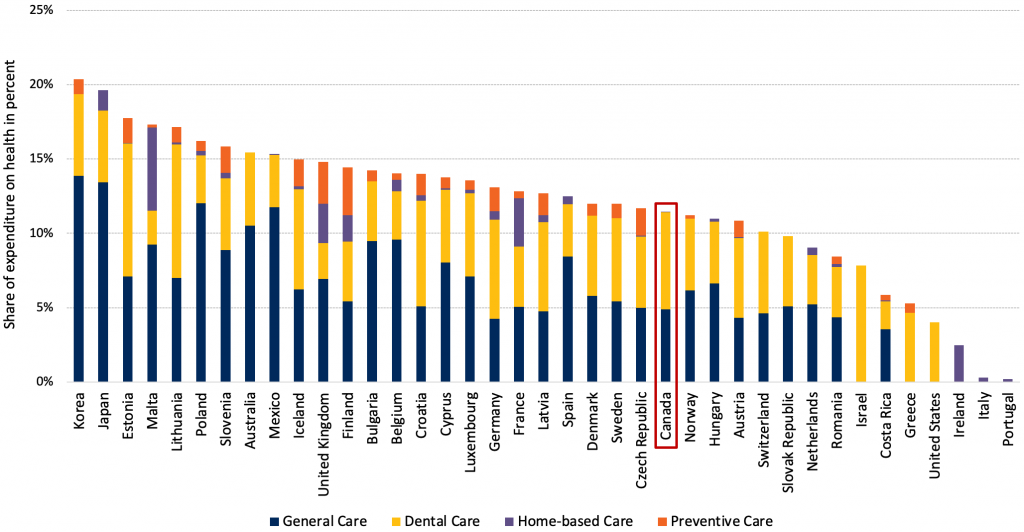
Compared with other high-performing jurisdictions internationally, Canadian primary care is less organized in terms of regional infrastructure to support communication, quality improvement, and system integration.39,40,103 Figure 5 shows that Canada spends substantially less on primary health care services than most comparable countries as a proportion of total health expenditure.104
Previously established relationships have been a key facilitator of collaborations during the pandemic.105 One review conducted in 2021 found that organizations were able to draw on OHT structures and processes where these existed, but they retreated from integrated approaches otherwise.105 The same review found that proactive outreach to those with the greatest needs through partners that have the right relationships and capacities should be systematized as part of an overall population-health management approach to COVID-19 recovery. Hospital leaders reported new relationships with primary care as a result of the pandemic. A survey conducted by the Ontario Hospital Association in August 2022 received responses from 80 Ontario hospitals. Two-thirds reported new investments in primary care engagement and the majority (53%) reported involvement of local primary care professionals in local decision-making for COVID-19 (e.g., chairs or co-chairs of committees).106
Data to Drive Pandemic Responses and System Improvements
More coordinated and integrated care in Ontario will require more coordinated and integrated collection and use of data to drive both pandemic responses and health system improvements. Data collection instituted partway through the pandemic was critical for the development and rollout of primary care initiatives.107 The World Health Organization has urged such data collection, stating that developing effective prevention strategies requires countries to improve their information.108 Worldwide and in Ontario, the pandemic brought to light many deeply embedded social and health inequities. People living on low incomes, people experiencing homelessness, newcomers, racialized populations, and others affected by the social determinants of health experienced a much higher burden of disease.109 However, little routine socio-demographic data was being collected. Data reports were developed using area-level data to fill this gap and these demonstrated gross inequities, with COVID-19 rates ten times higher than the general population in some populations.107 This information was critical to inform testing and vaccine rollout in priority communities which included community outreach, increased testing, and wraparound supports. The Ontario Government’s High Priority Community Strategy provided increased funding to support tailored outreach, community ambassadors, increased access to testing, isolation facilities, and vaccine outreach (pop-up clinics, mobile units, and more).110 CHCs and other community organizations played a key role in this strategy, which was embedded in communities and represented deep partnerships with primary care. Ensuring a community-led response will continue to be critical for reaching the most at-risk populations due to existing trust and relationships.107
Interpretation
The practice and capacity of primary care in Ontario have changed since the start of the COVID-19 pandemic. Primary care is facing an accelerating capacity crisis driven by trends in HHR, varying models of care, and gaps in integration and coordination. These complex factors, when coupled with longstanding health system challenges, pose an ongoing threat not only to coordinated pandemic response and future pandemic preparedness, but also to routine health system functioning.
Changing physician demographics, impending retirements, shifts away from comprehensive family practice, and burnout across the professions that comprise PCCs are important trends undermining primary care HHR capacity. A lack of team-based supports, administrative and operational challenges for those starting their own practice, and unpredictability of fee-for-service compensation models, may all be contributing to the HHR crisis. These affect not only physicians but all PCCs. A lack of PCCs across the health professions that work in primary care threatens the success of FHTs, which have proven to be an important model of effective primary care in Ontario.
Formal patient attachment to a physician or team-based model of care through a PEM, and variations in PCC practices, have been important determinants of access, continuity, and outcomes throughout the COVID-19 pandemic, with implications for primary care capacity moving forward. Indeed, evidence during COVID-19 found that formal attachment was protective of continuity, whereas patients not formally attached were less likely to experience continuity.46 Even prior to the COVID-19 pandemic, those not formally attached were more likely to be low-income, urban, and new immigrants, and have complex needs that may be better met with the support of interdisciplinary teams.51 Access to teams is likewise inequitably distributed, with marginalized populations less likely to be served in these models of care despite their more complex medical and social needs.47,49,51 Another challenging factor is the high level of variation across the health system in the quality of primary care,83–85 which likely has been exacerbated during COVID-19. There has been a rapid inclusion of virtual care within primary care, but we do not know the optimal balance between virtual and in-person assessments nor the cost-effectiveness of virtual models. A very small percentage of primary care physicians have shifted towards a solely virtual model, and this is unlikely to be a high-value model of care. Models of corporate “virtual-only” care that have grown in the pandemic are not consistent with the core principle of continuity of care and require evaluation.
The need for coordinated and integrated primary care in Ontario is pressing. Throughout the COVID-19 pandemic, where relationships existed already, collaborative, cross-sectoral efforts were more successful. Further, more coordinated and integrated care in Ontario will also require more coordinated and integrated collection and use of data to drive both pandemic responses and health system improvements. Better data also creates a mechanism of accountability for PCCs and primary care practices.
Primary care is crucial to ongoing pandemic preparedness, response, and recovery, continued health system improvement, person-centred care in communities, and population health. As the capacity crisis in primary care deepens and demand continues to increase, efforts are needed to address the factors that limit equitable primary care provision. These include training, supporting, and retaining the interdisciplinary HHR that comprise team-based models of care, and supporting PEMs that are equitably accessible to all Ontarians and aligned with the Quadruple Aim outlined in Ontario Health’s Vision for Health Care in Ontario; that is, improving the patient and caregiver experience, improving the health of populations, reducing the per capita cost of health care, and improving the work life of clinicians. Appropriate governance models for data, quality, planning, and accountability are needed, as well as ensuring infrastructure and resources that support coordinated and integrated primary care. Evidence shows health systems with stronger primary care have better population health outcomes, improved health equity, and lower overall costs. Addressing the significant primary care capacity gaps described in this Brief will not only result in better population outcomes but will also strengthen pandemic preparedness, response, and recovery in Ontario.
Methods Used for This Science Brief
The following methods were used in a single common strategy to construct all three parts of this Science Brief; subsequent to the writing of the first draft of the Brief, a decision was taken to divide the content into three parts.
We sought peer-reviewed literature as well as relevant pre-prints, academic presentations, reports, manuals, and other grey literature in addition to data from media scans and health system sources to construct the fullest possible picture of the impact of COVID-19 pandemic on the state of primary care in Ontario and Canada.
We searched Ovid MEDLINE and limited the search strategy to studies from January 1, 2019 to July 27, 2022, using the COVID-19 filter adapted for search strategies created by Library and Knowledge Services of the National Health Services, using the key terms: “general practitioners or physicians”, “primary care, patient care team or hospital rapid response team or nursing”, “community health services or community health nursing or home care services”, “teams or attachment or universal or empanelment”, “interdisciplinary or multidisciplinary or system or primary or policy or service or delivery”, “delivery of health care”, “Ontario and Canada”. A grey literature search of relevant reports, manuals and policy papers was also done focusing on Primary care and COVID-19 pandemic response, Pandemic Recovery, Integration of care, and Team-Based Care. The grey literature search was not limited to the Canadian context and yielded seven primary reports. At the request of the authors, the Ontario Medical Association library team provided a scan of media and grey literature using the team’s daily in-house environmental scanning product, “The Scan”, focusing on articles and other materials addressing the “state of primary care in Ontario during the pandemic” from 2021 to 2022.
Our initial search results yielded a total of 215 reports and papers, which were shared in a common folder for review and analysis by study lead authors and co-authors. These were reviewed, with lead authors for each section using those papers relevant to their portion of the Brief, and reviewed several times to ensure inclusion of relevant evidence in each section of the Brief. Unpublished emerging data was sought out from relevant health system sources such as the Ministry of Health, Ontario Health, and the INSPIRE-Primary Health Care research team, with authors permission, to supplement published data.
Expert consensus was then sought on the basis of parts 1 and 2 to draw the “lessons learned” and recommendations outlined in part 3. This was an iterative process conducted with the six core co-authors representing family physician leaders and researchers affiliated with various academic institutions in Ontario. The process included virtual meetings, email communications and clarification of language. A simple analytical framework, Search, Appraisal, Synthesis and Analysis (SALSA) was employed, and a narrative summary was generated for each of three sections of this Brief.
Drafts of the Brief sections were shared with primary care stakeholders across the province, the country and internationally for feedback, including primary care clinicians and leaders associated with the Ontario Ministry of Health, Ontario Health, the Ontario Medical Association and Section of General and Family Practice, Alliance for Healthier Communities, Ontario College of Family Physicians, Association of Family Health Teams of Ontario, Seamless Care Optimizing the Patient Experience, Indigenous Primary Care Council and Black Physicians Association of Ontario. Based on the feedback, the project team and the COVID-19 Science Table provided additional comments and directions for policy recommendations.
References
1. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502. https://doi.org/10.1111/j.1468-0009.2005.00409.x
2. Starfield B. Is primary care essential? The Lancet. 1994;344(8930):1129-1133. https://doi.org/10.1016/S0140-6736(94)90634-3
3. Organisation for Economic Cooperation and Development. Primary health care is associated with reduced use of costly hospital and emergency department inputs. https://doi.org/10.1787/9789264266414-en
4. Robillard R, Daros AR, Phillips JL, et al. Emerging new psychiatric symptoms and the worsening of pre-existing mental disorders during the COVID-19 pandemic: A Canadian multisite study. Can J Psychiatry Rev Can Psychiatr. 2021;66(9):815-826. https://doi.org/10.1177/0706743720986786
5. Ministry of health: Spending plan review. Financial Accountability Office of Ontario (FAO). https://www.fao-on.org/en/Blog/Publications/2021-health-estimates
6. How difficult is it to find a family doctor? CBC Listen. Published June 15, 2022. https://www.cbc.ca/listen/live-radio/1-45-ontario-today
7. Kiran T, Green ME, Wu CF, et al. Family physicians stopping practice during the COVID-19 pandemic in Ontario, Canada. Ann Fam Med. 2022;20(5):460-463. https://doi.org/10.1370/afm.2865
8. Rudoler D, Peterson S, Stock D, et al. Do recent family physician graduates practice differently? A longitudinal study of primary care visits and continuity in four Canadian provinces. medRxiv. Published online March 22, 2022:2022.03.11.22272161. https://doi.org/10.1101/2022.03.11.22272161
9. DFP April Research Rounds: The “kids” are alright: Practice patterns among early-career family physicians and implications for primary care policy and workforce planning. Family Medicine. Published March 2022. https://www.familymed.ubc.ca/2022/03/14/dfp-april-research-rounds-the-kids-are-alright-practice-patterns-among-early-career-family-physicians-and-implications-for-primary-care-policy-and-workforce-planning/
10. A profile of physicians in Canada, 2020. Canadian Institute for Health Information. https://www.cihi.ca/en/a-profile-of-physicians-in-canada-2020
11. Stewart M, Ryan B. Ecology of health care in Canada. Can Fam Physician. 2015;61(5):449-453. https://www.cfp.ca/content/61/5/449
12. White KL, Williams TF, Greenberg BG. The ecology of medical care. Bull N Y Acad Med.1961;73(1):187-212. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2359390/
13. Statistics Canada Government of Canada. In the midst of high job vacancies and historically low unemployment, Canada faces record retirements from an aging labour force: Number of seniors aged 65 and older grows six times faster than children 0-14. Published April 27, 2022. https://www150.statcan.gc.ca/n1/daily-quotidien/220427/dq220427a-eng.htm
14. 1-in-5 Ontarians could be without a family doctor by 2025. OCFP. Published September 13, 2022. https://www.ontariofamilyphysicians.ca/news-features/family-medicine-news/~260-1-in-5-Ontarians-could-be-without-a-family-doctor-by-2025?resourceID=171
15. Premji K, Ryan B, Green M. HHR impacts of an aging family physician workforce. Presented at: Innovations Strengthening Primary Health Care Through Research (INSPIRE-PHC) Stakeholders Meeting (not poblished online).; 2022.
16. Simkin S, Dahrouge S, Bourgeault IL. End-of-career practice patterns of primary care physicians in Ontario. Can Fam Physician. 2019;65(5):e221-e230. https://www.cfp.ca/content/65/5/e221
17. Schultz SE, Glazier RH. Identification of physicians providing comprehensive primary care in Ontario: a retrospective analysis using linked administrative data. Can Med Assoc Open Access J. 2017;5(4):E856-E863. https://doi.org/10.9778/cmajo.20170083
18. Rosenthal TC. The medical home: Growing evidence to support a new approach to primary care. J Am Board Fam Med. 2008;21(5):427-440. https://doi.org/10.3122/jabfm.2008.05.070287
19. Bazemore A, Petterson S, Peterson LE, Bruno R, Chung Y, Phillips RL. Higher primary care physician continuity is associated with lower costs and hospitalizations. Ann Fam Med. 2018;16(6):492-497. https://doi.org/10.1370/afm.2308
20. McAlister FA, Bakal JA, Green L, Bahler B, Lewanczuk R. The effect of provider affiliation with a primary care network on emergency department visits and hospital admissions. CMAJ. 2018;190(10):E276-E284. https://doi.org/10.1503/cmaj.170385
21. OECD. Realising the potential of primary health care. Published 2020. https://www.oecd-ilibrary.org/social-issues-migration-health/realising-the-potential-of-primary-health-care_a92adee4-en
22. Jabbarpour Y, Coffman M, Habib A. Advanced primary care: A key contributor to successful ACOs. Patient-Centered Primary Care Collaborative; 2018. https://www.pcpcc.org/sites/default/files/resources/PCPCC%202018%20Evidence%20Report.pdf
23. Gray DJP, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors—a matter of life and death? A systematic review of continuity of care and mortality. BMJ Open. 2018;8(6):e021161. https://doi.org/10.1136/bmjopen-2017-021161
24. CaRMS R-1 data and reports: R-1 match reports. CaRMS. Published 2022. https://www.carms.ca/data-reports/r1-data-reports/
25. Kabir M, Randall E, Mitra G, et al. Resident and early-career family physicians’ focused practice choices in Canada: A qualitative study. Br J Gen Pract. 2022;72(718):e334-e341. https://doi.org/10.3399/BJGP.2021.0512
26. Graduation questionnaire. AFMC. https://www.afmc.ca/en/news-publications/graduation-questionnaire
27. Time to erase student debt in Canada. The Star. Published August 30, 2022. https://www.thestar.com/opinion/contributors/2022/08/30/time-to-follow-bidens-lead-but-go-further-and-erase-student-debt-in-canada.html
28. Lemire F. Addressing family physician shortages. Can Fam Physician Med Fam Can. 2022;68(5):392. https://doi.org/10.46747/cfp.6805392
29. Smith A. CMA 2021 national physician health survey. Canadian Medical Association; 2022:122. https://www.cma.ca/sites/default/files/2022-08/NPHS_final_report_EN.pdf
30. Mathews M, Meredith L, Ryan D, et al. The roles of family physicians during a pandemic. Healthc Manage Forum. Published online July 17, 2022:8404704221112311. https://doi.org/10.1177/08404704221112311
31. Statistics Canada Government of Canada. Experiences of health care workers during the COVID-19 pandemic, September to November 2021. Published June 3, 2022. https://www150.statcan.gc.ca/n1/daily-quotidien/220603/dq220603a-eng.htm
32. Zaidi D. Nurses more likely to quit in next 3 years, health worker survey finds. CTVNews. Published June 3, 2022. https://www.ctvnews.ca/health/nurses-more-likely-to-quit-in-next-3-years-health-worker-survey-finds-1.5932193
33. Bazemore A, Grunert T. Sailing the 7c’s: Starfield revisited as a foundation of family medicine residency redesign. Fam Med. 2021;53(7):506-515. https://doi.org/10.22454/FamMed.2021.383659
34. Ontario health teams: Guidance for health care providers and organizations. Ontario Health; :33. https://health.gov.on.ca/en/pro/programs/connectedcare/oht/docs/guidance_doc_en.pdf
35. Huston P, Campbell J, Russell G, et al. COVID-19 and primary care in six countries. BJGP Open. 2020;4(4). https://doi.org/10.3399/bjgpopen20X101128
36. Unruh L, Allin S, Marchildon G, et al. A comparison of 2020 health policy responses to the COVID-19 pandemic in Canada, Ireland, the United Kingdom and the United States of America. Health Policy. 2022;126(5):427-437. https://doi.org/10.1016/j.healthpol.2021.06.012
37. Desborough J, Dykgraaf SH, Phillips C, et al. Lessons for the global primary care response to COVID-19: A rapid review of evidence from past epidemics. Fam Pract. 2021;38(6):811-825. https://doi.org/10.1093/fampra/cmaa142
38. Tollinsky N. Canada’s healthcare system scores poorly against peers. Canadian Healthcare Technology. Published September 21, 2021. https://www.canhealth.com/2021/09/30/canadas-healthcare-system-scores-poorly-against-peers/
39. Schneider EC, Shah A, Doty MM, Tikkanen R, Fields K, II RDW. Mirror, mirror 2021 – Reflecting poorly: Health care in the U.S. compared to other high-income countries.; 2021:39. https://www.commonwealthfund.org/sites/default/files/2021-08/Schneider_Mirror_Mirror_2021.pdf
40. Philippon DJ, Marchildon GP, Ludlow K, Boyling C, Braithwaite J. The comparative performance of the Canadian and Australian health systems. Healthc Manage Forum. 2018;31(6):239-244. https://doi.org/10.1177/0840470418788378
41. Esmail N. Health Care Lessons from the Netherlands. Fraser Institute; 2014:67. https://www.fraserinstitute.org/sites/default/files/health-care-lessons-from-the-netherlands.pdf
42. Fuchs A. How is Alberta’s health system structured? Partners in Health; 2021. https://www.partnersinhealth.ca/2021/05/28/how-is-albertas-health-system-structured/
43. How Canada compares: Results from the commonwealth fund 2019 international health policy survey of primary care physicians. Chartbook. Canadian Institute for Health Information; 2020. https://www.cihi.ca/sites/default/files/document/cmwf-2019-chartbook-en-web.pptx
44. Evidence summary: The benefits of relational continuity in primary care. Alberta Medical Association; 2017. https://actt.albertadoctors.org/file/top–evidence-summary–value-of-continuity.pdf
45. Nowak DA, Sheikhan NY, Naidu SC, Kuluski K, Upshur REG. Why does continuity of care with family doctors matter? Review and qualitative synthesis of patient and physician perspectives. Can Fam Physician Med Fam Can. 2021;67(9):679-688. https://doi.org/10.46747/cfp.6709679
46. Glazier R, Kopp A, Kiran T, Green M, Howard M. Visits to own primary care physician: Comparing pre-pandemic and pandemic periods in 2019-2020, in Ontario, Canada. INSPIRE-PHC Presentation (Manuscript in preparation).; 2022.
47. Kiran T, Kopp A, Glazier RH. Those left behind from voluntary medical home reforms in Ontario, Canada. Ann Fam Med. 2016;14(6):517-525. https://doi.org/10.1370/afm.2000
48. Green M, Glazier R, Frymire E, et al. Primary care data reports for Ontario health teams (OHTs). OCHPP. https://www.ontariohealthprofiles.ca/ontarioHealthTeam.php
49. Xia Y, Ma H, Moloney G, et al. Geographic concentration of SARS-CoV-2 cases by social determinants of health in metropolitan areas in Canada: A cross-sectional study. CMAJ. 2022;194(6):E195-E204. https://doi.org/10.1503/cmaj.211249
50. Ravichandiran N, Mathews M, Ryan BL. Utilization of healthcare by immigrants in Canada: A cross-sectional analysis of the Canadian Community Health Survey. BMC Prim Care. 2022;23(1):69. https://doi.org/10.1186/s12875-022-01682-2
51. Glazier RH, Gozdyra P, Kim M, et al. Geographic variation in primary care need, service use and providers in Ontario, 2015/16. ICES; :150. https://maphealth.ca/wp-content/uploads/2019/10/Full-Report-Geographic-Variation-in-Primary-Care-Need-Service-Use-and-Providers-in-Ontario-August-2018.pdf
52. INSPIRE-PHC. INSPIRE-PHC. https://inspire-phc.org/
53. Best advice: Team-based care in the patient’s medical home. The College of Family Physicians of Canada; 2017:22. http://patientsmedicalhome.ca/files/uploads/BAG_TeamBasedCare_ENG-1.pdf
54. Kiran T, Kopp A, Moineddin R, Glazier RH. Longitudinal evaluation of physician payment reform and team-based care for chronic disease management and prevention. CMAJ. 2015;187(17):E494-E502.https://doi.org/10.1503/cmaj.150579
55. Final report: An external evaluation of the family health team (FHT) initiative. The Conference Board of Canada. Published 2014. https://www.conferenceboard.ca/e-library/abstract.aspx?did=6711
56. Bhuiya A, Scallan E, Alam S, Sharma K, Wilson M. Identifying the features and impacts of community health centres. McMaster Health Forum; 2020:46. https://www.mcmasterforum.org/docs/default-source/product-documents/rapid-responses/identifying-the-features-and-impacts-of-community-health-centres.pdf?sfvrsn=234559d5_3
57. Kiran T, Eissa A, Mangin D, et al. Brief on Primary Care Part 1: The roles of primary care clinicians and practices in the first two years of the COVID-19 pandemic in Ontario. Sci Briefs Ont COVID-19 Sci Advis Table. 2022;3(67). https://doi.org/10.47326/ocsat.2022.03.67.1.0
58. Evaluation: the Ontario COVID@Home clinical pathway for primary care of acute covid illness: A report for the Ontario ministry of health (not published online). Department of Family Medicine, McMaster University; 2022.
59. Lopez-Leon S, Wegman-Ostrosky T, Perelman C, et al. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. medRxiv. Published online January 30, 2021:2021.01.27.21250617.https://doi.org/10.1101/2021.01.27.21250617
60. Aboriginal health access centres. Alliance for Healthier Communities. https://www.allianceon.org/aboriginal-health-access-centres
61. Ministry of Health and Long-Term Care Government of Ontario. Family health teams. https://www.health.gov.on.ca/en/pro/programs/fht/
62. Ministry of Health and Long-Term Care Government of Ontario. Community health centres. https://www.health.gov.on.ca/en/common/system/services/chc/
63. Ministry of Health and Long-Term Care Government of Ontario. Nurse practitioner-led clinics. https://www.health.gov.on.ca/en/pro/programs/np_clinics/default.aspx
64. Glazier R, Zagorski B, Rayner J. Comparison of primary care models in Ontario by demographics, case mix and emergency department use, 2008/09 to 2009/10. Published 2012. https://www.ices.on.ca/Publications/Atlases-and-Reports/2012/Comparison-of-Primary-Care-Models
65. Mitra G, Grudniewicz A, Lavergne MR, Fernandez R, Scott I. Alternative payment models: A path forward. Can Fam Physician. 2021;67(11):805-807. https://doi.org/10.46747/cfp.6711805
66. Residency training profile for family medicine and enhanced skills programs leading to certificates of added competence. The College of Family Physicians of Canada; 2021:77. https://www.cfpc.ca/CFPC/media/Resources/Education/Residency-Training-Profile-ENG.pdf
67. Laberge M, Wodchis WP, Barnsley J, Laporte A. Costs of health care across primary care models in Ontario. BMC Health Serv Res. Published online 2017. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-017-2455-1
68. MacAdam M, Hollander MJ, Miller JA, Pedlar NC and D. Increasing value for money in the Canadian healthcare system: New findings and the case for integrated care for seniors. Healthc Q. 2009;12(1). https://www.longwoods.com/content/20414/healthcare-quarterly/increasing-value-for-money-in-the-canadian-healthcare-system-new-findings-and-the-case-for-integrat
69. Carter R, Riverin B, Levesque JF, Gariepy G, Quesnel-Vallée A. The impact of primary care reform on health system performance in Canada: A systematic review. BMC Health Serv Res. 2016;16(1):324. https://doi.org/10.1186/s12913-016-1571-7
70. Riverin BD, Li P, Naimi AI, Strumpf E. Team-based versus traditional primary care models and short-term outcomes after hospital discharge. CMAJ. 2017;189(16):E585-E593. https://doi.org/10.1503/cmaj.160427
71. Green ME, Hogg W, Gray D, et al. Financial and work satisfaction: Impacts of participation in primary care reform on physicians in Ontario. Healthc Policy. 2009;5(2):e161-e176. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805146/
72. A healthy Ontario: Building a sustainable health care system: Chapter 2: The vision for health care in Ontario. Ontario.ca. https://www.ontario.ca/document/healthy-ontario-building-sustainable-health-care-system/chapter-2-vision-health-care-ontario
73. INFOBulletin #11131: Supporting areas of high physician need: Changes to entry into Family Health Organizations and Family Health Networks. Ministry of Health and Long-Term Care; 2015. https://www.health.gov.on.ca/en/pro/programs/ohip/bulletins/11000/bul11131.pdf
74. Ontario’s doctors ratify new three-year agreement with province. Ontario Medical Association. Published May 2022. https://www.oma.org/newsroom/news/2022/march/ontarios-doctors-ratify-new-three-year-agreement-with-province/
75. Kiran T, Green ME, Strauss R, et al. Are primary care virtual visits associated with higher emergency department use? A cross-sectional analysis from Ontario, Canada. medRxiv. Published online September 9, 2022:2022.09.08.22278709. https://doi.org/10.1101/2022.09.08.22278709
76. Lapointe-Shaw L, Salahub C, Bhatia RS, et al. Characteristics and healthcare use of patients attending virtual walk-in clinics: A cross-sectional analysis. medRxiv. Published online March 1, 2022:2022.02.28.22271640. https://doi.org/10.1101/2022.02.28.22271640
77. Primary care performance. Health Quality Ontario (HQO). https://www.hqontario.ca/System-Performance/Primary-Care-Performance/Same-Day-or-Next-Day-Appo
78. Patient involvement in decisions about primary care Ontario. Health Quality Ontario (HQO). https://www.hqontario.ca/System-Performance/Primary-Care-Performance/Patient-Involvement-in-Decisions-about-Care
79. Diabetes complications in Ontario patients. Health Quality Ontario (HQO). https://www.hqontario.ca/System-Performance/Primary-Care-Performance/Diabetes-Complications
80. Foley TJ, Vale L. What role for learning health systems in quality improvement within healthcare providers? Learn Health Syst. 2017;1(4):e10025. https://doi.org/10.1002/lrh2.10025
81. Kuluski K, Guilcher SJT. Toward a person-centred learning health system: Understanding value from the perspectives of patients and caregivers. Healthc Pap. 2019;18(4). https://www.longwoods.com/content/26030/toward-a-person-centred-learning-health-system-understanding-value-from-the-perspectives-of-patient
82. Mondoux S, Thull-Freedman J, Dowling S, et al. Quality improvement in the time of coronavirus disease 2019 – A change strategy well suited to pandemic response. Can J Emerg Med. 2020;22(4):422-425. https://doi.org/10.1017/cem.2020.386
83. Quality standards: Asthma quality standard: Guiding evidence-based care for people 16 years of age and older in Ontario. Public Health Ontario. https://hqontario.ca/Portals/0/documents/evidence/quality-standards/qs-asthma-in-adults-case-for-improvement-en.pptx
84. Quality standards: Major depression: Care for adults and adolescents. Public Health Ontario. https://www.hqontario.ca/Portals/0/documents/evidence/quality-standards/qs-depression-information-data-1609-en.pptx
85. Quality standards: Chronic obstructive pulmonary disease: A quality standard for guiding evidence-based care for people living with COPD in Ontario. Public Health Ontario. https://www.hqontario.ca/Portals/0/documents/evidence/quality-standards/qs-chronic-obstructive-pulmonary-disease-case-for-improvement-en.pptx
86. Jordan RE, Adab P, Cheng KK. COVID-19: Risk factors for severe disease and death. BMJ. 2020;368:m1198. https://doi.org/10.1136/bmj.m1198
87. Mangin D, Laswon J, Risdon C. Association between frailty, chronic conditions and socio-economic status in community-dwelling older adults attending primary care: A cross-sectional study using practice-based research network data [in prep].; 2022.
88. Underlying medical conditions associated with higher risk for severe COVID-19: Information for healthcare professionals. Centers for Disease Control and Prevention. Published February 11, 2020.https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html
89. Strengthening primary health care through primary care and public health collaboration: Final report for CHSRF. McMaster University; 2012. https://neltoolkit.rnao.ca/sites/default/files/Strengthening%20Primary%20Health%20Care%20through%20Primary%20Care%20and%20Public%20Health%20Collaboration_CHSRF%20Final%20Report.pdf
90. Price D, Baker E, Golden B, Hannam R. Patient care groups: A new model of population based primary health care for Ontario.; 2015:41. https://www.health.gov.on.ca/en/common/ministry/publications/reports/primary_care/primary_care_price_report.pdf
91. Involving family physicians in health reform: Tips for Ontario health teams. Ontario College of Family Physicians; 2020. https://www.ontariofamilyphysicians.ca/tools-resources/timely-trending/ontario-health-team-oht-overview/tipsheet_oht_online-feb2020.pdf
92. Charles A, Wenzel L, Kershaw M, Ham C, Nicola Walsh. A year of integrated care systems: Reviewing the journey so far. The King’s Fund; 2018:112. https://www.kingsfund.org.uk/sites/default/files/2018-09/Year-of-integrated-care-systems-reviewing-journey-so-far-full-report.pdf
93. Nicholson C, Jackson C, Marley J. A governance model for integrated primary/secondary care for the health-reforming first world: Results of a systematic review. BMC Health Serv Res. 2013;13(1):528. https://doi.org/10.1186/1472-6963-13-528
94. Integrated care: Our position. The King’s Fund. Published May 17, 2022. https://www.kingsfund.org.uk/projects/positions/integrated-care
95. Mosby I, Swidrovich J. Medical experimentation and the roots of COVID-19 vaccine hesitancy among Indigenous Peoples in Canada. CMAJ. 2021;193(11):E381-E383. https://doi.org/10.1503/cmaj.210112
96. Eissa A, Lofters A, Akor N, Prescod C, Nnorom O. Increasing SARS-CoV-2 vaccination rates among Black people in Canada. CMAJ. 2021;193(31):E1220-E1221. https://doi.org/10.1503/cmaj.210949
97. Public Health Agency of Canada. From risk to resilience: An equity approach to COVID-19.; 2020. https://www.canada.ca/content/dam/phac-aspc/documents/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19/cpho-covid-report-eng.pdf
98. Family doctors help lead black health vaccine initiative. University of Toronto: Temerty Faculty of Medicine. Published May 2021. https://temertymedicine.utoronto.ca/news/family-doctors-help-lead-black-health-vaccine-initiative
99. Bhatti S, Rayner EC and J. A rapid primary healthcare response to COVID-19: An equity-based and systems – thinking approach to care ensuring that no one is left behind. Healthc Q. 2020;23(3). https://www.longwoods.com/content/26336/healthcare-quarterly/a-rapid-primary-healthcare-response-to-covid-19-an-equity-based-and-systems-thinking-approach-to
100. Toronto black vaccine engagement team. Black Health Alliance. https://covid.blackhealthalliance.ca/bvet
101. Ndumbe-Eyoh S. “We were out ahead of public health”: Leading COVID-19 vaccine equity for black communities across Canada. National Collaborating Centre for Determinants of Health. https://nccdh.ca/images/uploads/COVID-19_vaccine_equity_for_Black_communities_EN_Nov24.pdf
102. Dye A, Eissa A, Esho D. Black patients experiencing vaccine distrust : The LEAPS of care framework can help address concerns about the COVID-19 vaccine among Black patients experiencing hesitancy.Ontario Medical Association; 2022. https://www.oma.org/member/practice-professional-support/patient-care/vaccines/vaccine-hesitancy/black-patients-experiencing-vaccine-distrust/
103. How Canada compares: Results from the commonwealth fund’s 2020 international health policy survey of the general population in 11 countries. Canadian Institute for Health Information; 2021:119. https://secure.cihi.ca/free_products/how-canada-compares-cmwf-survey-2020-chartbook-en.pdf
104. Health expenditure and financing. OECD. https://stats.oecd.org/Index.aspx?DataSetCode=SHA
105. OHT Learnings through COVID-19. Ministry of Health; 2021:37. https://www.health.gov.on.ca/en/pro/programs/connectedcare/oht/docs/OHT%20VES_covid_learnings.pdf
106. Ontario Hospital Association internal survey of members (not published online). OHA; 2022.
107. Enhanced epidemiological summary: COVID-19 in Ontario – a focus on neighbourhood diversity, February 26, 2020 to December 13, 2021. Public Health Ontario; 2022:26. https://www.publichealthontario.ca/-/media/documents/ncov/epi/2020/06/covid-19-epi-diversity.pdf
108. Data collection tools. World Health Organization. https://www.who.int/data/data-collection-tools
109. Horton R. Offline: COVID-19 is not a pandemic. The Lancet. 2020;396(10255):874. https://doi.org/10.1016/S0140-6736(20)32000-6
110. Government of Ontario. Ontario supporting high priority communities. Ontario Newsroom. Published December 21, 2020. https://news.ontario.ca/en/backgrounder/59793/ontario-supporting-high-priority-communities
Document Information & Citation
Author Contributions: This section applies across all three parts of the Brief. DaM (Danielle Martin) and FR co-conceived the Science Brief with guidance and input from KB. The approach and design were developed together with TK, AE, SN, DM, NI, IB, AP. This core author group also led the data collection, analysis and interpretation with input from the rest of the authorship team, particularly KP, LJ, JN, OB, BCF, DN, AG, MG, EM, JR, FR.
DaM, IB, AE, NI, TK, DM, SN, AP, KP wrote the first draft of the Science Brief with significant contributions from KB, AG, MG, LJ, DK, EM, DN, JR, FR. All authors revised the Science Brief critically for important intellectual content and approved the final version, and extensive work on references and figures was led by SB, AE, NSB and AP. International unpublished data were provided by MK and SH.
Robust external review was then conducted and feedback incorporation and further revision were led by TK (part 1), DM and KP (part 2), and NI (part 3), with support from SB, AE and DaM. All authors revised the parts of the Science Brief on which they are named for critically for important intellectual content.
The authors would like to thank Joanne Sung, Karen Lee, Pat Buczkowski, Mahta Norouzi, Roisin McElroy, Kieran Quinn and the University of Toronto library service for their contributions to the literature review, reference checking, assistance with figures, formatting, and copyediting of this Science Brief; Dan Warshafsky, Zahra Ismail, and the teams at INSPIRE-PHC, and the Ontario Hospital Association for the provision of data; the team at the Ontario Science Advisory Table secretariat as well as Karla Freeman and Rebecca Clark at the Department of Family Medicine McMaster University for their assistance and support with editing, formatting, and supporting review of the brief; Alisa Kim and the Department of Family and Community Medicine at the University of Toronto for support throughout the process.
Citation: Mangin D, Premji K, Bayoumi I, et al. Brief on Primary Care Part 2: Factors affecting primary care capacity in Ontario for pandemic response and recovery. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2022;3(68). https://doi.org/10.47326/ocsat.2022.03.68.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners can be found at https://covid19-sciencetable.ca/. The declarations of interest of external authors can be found under Additional Resources.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners.
