Key Message
Ontario long-term care (LTC) home residents have experienced disproportionately high morbidity and mortality, both from COVID-19 and from the conditions associated with the COVID-19 pandemic.
There are several measures that could be effective in preventing COVID-19 outbreaks, hospitalizations, and deaths in Ontario’s LTC homes, if implemented.
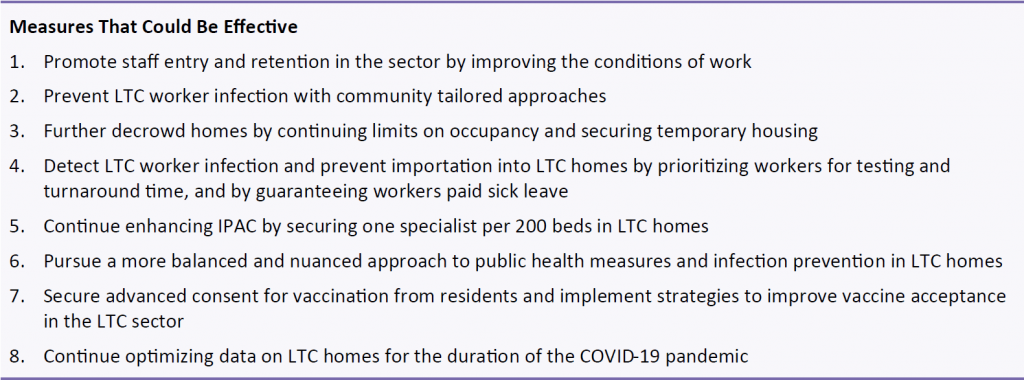
First, temporary staffing could be minimized by improving staff working conditions. Second, homes could be further decrowded by a continued disallowance of three- and four-resident rooms and additional temporary housing for the most crowded homes. Third, the risk of SARS-CoV-2 infection in staff could be minimized by approaches that reduce the risk of transmission in communities with a high burden of COVID-19.
Summary
Background
The Province of Ontario has 626 licensed LTC homes and 77,257 long-stay beds; 58% of homes are privately owned, 24% are non-profit/charitable, 16% are municipal. LTC homes were strongly affected during Ontario’s first wave of the COVID-19 pandemic.
Questions
What do we know about the first and second waves of COVID-19 in Ontario LTC homes?
Which risk factors are associated with COVID-19 outbreaks in Ontario LTC homes and the extent and death rates associated with outbreaks?
What has been the impact of the COVID-19 pandemic on the general health and wellbeing of LTC residents?
How has the existing Ontario evidence on COVID-19 in LTC settings been used to support public health interventions and policy changes in these settings?
What are the further measures that could be effective in preventing COVID-19 outbreaks, hospitalizations, and deaths in Ontario’s LTC homes?
Findings
As of December 12, 2020, a total of 2,479 Ontario LTC home residents have died of COVID-19, totaling 63% of all COVID-19 deaths in Ontario to date. Fewer LTC home outbreaks have occurred to date during the second wave as compared with the first wave. The infection and death rates among LTC residents have been lower during the second wave, as compared with the first wave, and a greater number of LTC outbreaks have involved only staff infections.
The growth rate of SARS-CoV-2 infections among LTC residents was slower during the first two months of the second wave in September and October 2020, as compared with the first wave. However, the growth rate after the two-month mark is comparatively faster during the second wave. The majority of second wave infections and deaths in LTC homes have occurred between November 1 and December 12, 2020. This highlights the recent intensification of the COVID-19 pandemic in LTC homes that has mirrored the recent increase in community transmission of SARS-CoV-2 across Ontario.
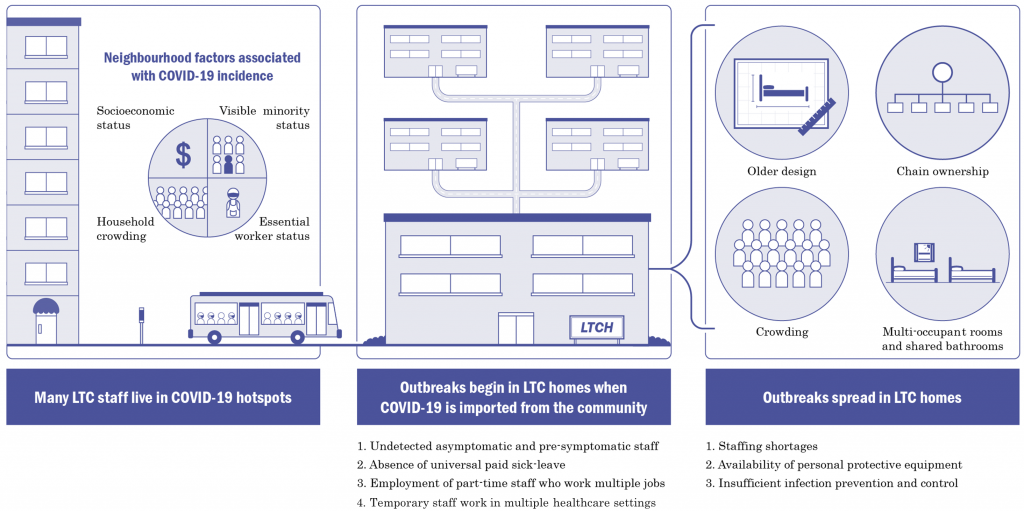
Evidence from Ontario demonstrates that the risk factors for SARS-CoV-2 outbreaks and subsequent deaths in LTC are distinct from the risk factors for outbreaks and deaths in the community (Figure 1). The most important risk factors for whether a LTC home will experience an outbreak is the daily incidence of SARS-CoV-2 infections in the communities surrounding the home and the occurrence of staff infections. The most important risk factors for the magnitude of an outbreak, and the number of resulting resident deaths are older design, chain ownership, and crowding.
Many Ontario LTC home residents have experienced severe and potentially irreversible physical, cognitive, psychological, and functional declines as a result of precautionary public health interventions imposed on homes, such as limiting access to general visitors and essential caregivers, resident absences, and group activities. There has also been an increase in the prescribing of psychoactive drugs to Ontario LTC residents.
The accumulating evidence on COVID-19 in Ontario’s LTC homes has been leveraged in several ways to support public health interventions and policy during the pandemic. Ontario evidence showed that SARS-CoV-2 infections among LTC staff was associated with subsequent COVID-19 deaths among LTC residents, which motivated a public order to restrict LTC staff from working in more than one LTC home in the first wave.
Emerging Ontario evidence on risk factors for LTC home outbreaks and deaths has been incorporated into provincial pandemic surveillance tools. Public health directives now attempt to limit crowding in LTC homes by restricting occupancy to two residents per room. The LTC visitor policy was also revised to designate a maximum of two essential caregivers who can visit residents without time limits, including when a home is experiencing an outbreak.
Several further measures could be effective in preventing COVID-19 outbreaks, hospitalizations, and deaths in Ontario’s LTC homes. First, temporary staffing could be minimized by improving staff working conditions. Second, the risk of SARS-CoV-2 infection in staff could be minimized by measures that reduce the risk of transmission in communities with a high burden of COVID-19. Third, LTC homes could be further decrowded by a continued disallowance of three- and four-resident rooms and additional temporary housing for the most crowded homes.
Other important issues include improved prevention and detection of SARS-CoV-2 infection in LTC staff, enhanced infection prevention and control (IPAC) capacity within the LTC homes, a more balanced and nuanced approach to public health measures and IPAC strategies in LTC homes, strategies to promote vaccine acceptance amongst residents and staff, and further improving data collection on LTC homes, residents, staff, visitors and essential caregivers for the duration of the COVID-19 pandemic.
Interpretation
Comparisons of the first and second waves of the COVID-19 pandemic in the LTC setting reveal improvement in some but not all epidemiological indicators. Despite this, the second wave is now intensifying within LTC homes and without action we will likely experience a substantial additional loss of life before the widespread administration of COVID-19 vaccines.
The predictors of outbreaks, the spread of infection, and deaths in Ontario’s LTC homes are well documented and have remained unchanged between the first and the second wave. Some of the evidence on COVID-19 in Ontario’s LTC homes has been effectively leveraged to support public health interventions and policies. Several further measures (Box 1), if implemented, have the potential to prevent additional LTC home COVID-19 outbreaks and deaths.
Slide Deck & Video Presentation
Document Information & Citation
Citation: Stall NM, Brown KA, Jones A, et al. COVID-19 and Ontario’s long-term care homes. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2020;1(5). https://doi.org/10.47326/ocsat.2020.01.05.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Copyright: 2020 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table and its partners.
