Key Message
Ontario long-term care (LTC) home residents have experienced disproportionately high morbidity and mortality, both from COVID-19 and from the conditions associated with the COVID-19 pandemic.
There are several measures that could be effective in preventing COVID-19 outbreaks, hospitalizations, and deaths in Ontario’s LTC homes, if implemented.
First, temporary staffing could be minimized by improving staff working conditions. Second, homes could be further decrowded by a continued disallowance of three- and four-resident rooms and additional temporary housing for the most crowded homes. Third, the risk of SARS-CoV-2 infection in staff could be minimized by approaches that reduce the risk of transmission in communities with a high burden of COVID-19.
Summary
Background
The Province of Ontario has 626 licensed LTC homes and 77,257 long-stay beds; 58% of homes are privately owned, 24% are non-profit/charitable, 16% are municipal. LTC homes were strongly affected during Ontario’s first and second waves of the COVID-19 pandemic.
Questions
What do we know about the first and second waves of COVID-19 in Ontario LTC homes?
Which risk factors are associated with COVID-19 outbreaks in Ontario LTC homes and the extent and death rates associated with outbreaks?
What has been the impact of the COVID-19 pandemic on the general health and wellbeing of LTC residents?
How has the existing Ontario evidence on COVID-19 in LTC settings been used to support public health interventions and policy changes in these settings?
What are the further measures that could be effective in preventing COVID-19 outbreaks, hospitalizations, and deaths in Ontario’s LTC homes?
Findings
As of January 14, 2021, a total of 3,211 Ontario LTC home residents have died of COVID-19, totaling 60.7% of all 5,289 COVID-19 deaths in Ontario to date. There have now been more cumulative LTC home outbreaks during the second wave as compared with the first wave. The infection and death rates among LTC residents have been lower during the second wave, as compared with the first wave, and a greater number of LTC outbreaks have involved only staff infections.
The growth rate of SARS-CoV-2 infections among LTC residents was slower during the first two months of the second wave in September and October 2020, as compared with the first wave. However, the growth rate after the two-month mark is comparatively faster during the second wave. The majority of second wave infections and deaths in LTC homes have occurred between December 1, 2020, and January 14, 2021 (most recent date of data extraction prior to publication). This highlights the recent intensification of the COVID-19 pandemic in LTC homes that has mirrored the recent increase in community transmission of SARS-CoV-2 across Ontario. Evidence from Ontario demonstrates that the risk factors for SARS-CoV-2 outbreaks and subsequent deaths in LTC are distinct from the risk factors for outbreaks and deaths in the community (Figure 1). The most important risk factors for whether a LTC home will experience an outbreak is the daily incidence of SARS-CoV-2 infections in the communities surrounding the home and the occurrence of staff infections. The most important risk factors for the magnitude of an outbreak and the number of resulting resident deaths are older design, chain ownership, and crowding.
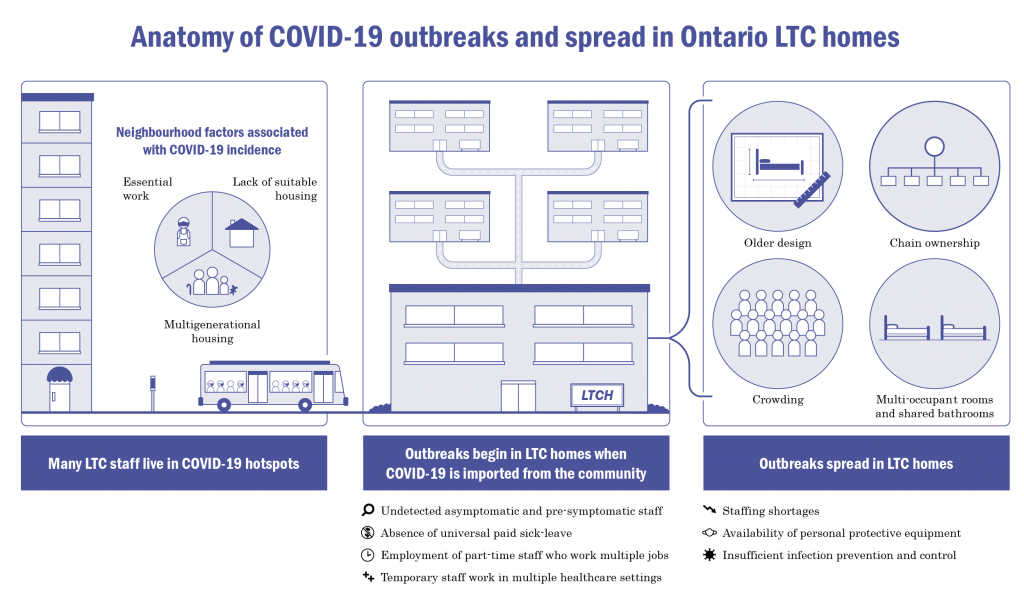
Figure from Peter Hamilton, personal communication.
Many Ontario LTC home residents have experienced severe and potentially irreversible physical, cognitive, psychological, and functional declines as a result of precautionary public health interventions imposed on homes, such as limiting access to general visitors and essential caregivers, resident absences, and group activities. There has also been an increase in the prescribing of psychoactive drugs to Ontario LTC residents.
The accumulating evidence on COVID-19 in Ontario’s LTC homes has been leveraged in several ways to support public health interventions and policy during the pandemic. Ontario evidence showed that SARS-CoV-2 infections among LTC staff was associated with subsequent COVID-19 deaths among LTC residents, which motivated a public order to restrict LTC staff from working in more than one LTC home in the first wave.
Emerging Ontario evidence on risk factors for LTC home outbreaks and deaths has been incorporated into provincial pandemic surveillance tools. Public health directives now attempt to limit crowding in LTC homes by restricting occupancy to two residents per room. The LTC visitor policy was also revised to designate a maximum of two essential caregivers who can visit residents without time limits, including when a home is experiencing an outbreak.
Several further measures could be effective in preventing COVID-19 outbreaks, hospitalizations, and deaths in Ontario’s LTC homes. First, temporary staffing could be minimized by improving staff working conditions. Second, the risk of SARS-CoV-2 infection in staff could be minimized by measures that reduce the risk of transmission in communities with a high burden of COVID-19. Third, LTC homes could be further decrowded by a continued disallowance of three- and four-resident rooms and additional temporary housing for the most crowded homes.
Other important issues include improved prevention and detection of SARS-CoV-2 infection in LTC staff, enhanced infection prevention and control (IPAC) capacity within the LTC homes, a more balanced and nuanced approach to public health measures and IPAC strategies in LTC homes, strategies to promote vaccine acceptance amongst residents and staff, and further improving data collection on LTC homes, residents, staff, visitors and essential caregivers for the duration of the COVID-19 pandemic.
Interpretation
Comparisons of the first and second waves of the COVID-19 pandemic in the LTC setting reveal improvement in some but not all epidemiological indicators. Despite this, the second wave is now intensifying within LTC homes and without action we will likely experience a substantial additional loss of life before the widespread administration and time-dependent maximal effectiveness of COVID-19 vaccines.
The predictors of outbreaks, the spread of infection, and deaths in Ontario’s LTC homes are well documented and have remained unchanged between the first and the second wave. Some of the evidence on COVID-19 in Ontario’s LTC homes has been effectively leveraged to support public health interventions and policies. Several further measures, if implemented, have the potential to prevent additional LTC home COVID-19 outbreaks and deaths.
Full Text
Background
The Province of Ontario has 626 licensed LTC homes and 77,257 long-stay beds. 58% of homes are privately owned, 24% are non-profit/charitable, 16% are municipal.1,2 As of February 2019, the average time to LTC placement was 161 days and the waitlist had nearly 35,000 individuals. Approximately 300 of Ontario’s LTC homes, containing more than 30,000 beds, are outdated and slated for redevelopment.2
Ontario LTC residents receive personal and nursing care as well as subsidized accommodation under a publicly funded LTC program. Most direct care in Ontario LTC homes is provided by personal support workers (PSWs) who account for 58% of the LTC workforce, with nurses accounting for an additional 25% of LTC staff.3 LTC homes were strongly affected during Ontario’s first and second waves of the COVID-19 pandemic.
Questions
What do we know about the first and second waves of COVID-19 in Ontario LTC homes?
Which risk factors are associated with COVID-19 outbreaks in Ontario LTC homes and the extent and death rates associated with outbreaks?
What has been the impact of the COVID-19 pandemic on the general health and wellbeing of LTC residents?
How has the existing Ontario evidence on COVID-19 in LTC settings been used to support public health interventions and policy changes in these settings?
What are the further measures that could be effective in preventing COVID-19 outbreaks, hospitalizations, and deaths in Ontario’s LTC homes?
Findings
As of 2018, Ontario LTC homes reported an average of 3.7 hours of paid direct care per resident per day, including all worked hours, vacations, statutory holidays, and benefits.3 The actual number of direct hours of direct care received per resident per day is approximately 2.7 hours.4
The majority (90%) of LTC home residents live with some form of cognitive impairment and 86% need extensive help with daily activities such as eating or toileting.2 Over the last several years, the complexity of residents living in Ontario LTC homes has substantially increased, with residents being older and having increased multimorbidity, polypharmacy and more extensive levels of physical and cognitive impairment.5 The average life expectancy of a LTC resident is approximately 18 months, and 11.7% of Ontario residents die within one year of admission to a LTC home.6
First and Second Waves of the COVID-19 Pandemic in Ontario’s LTC Homes
COVID-19 has taken a substantial toll on Ontario’s LTC homes. In the first wave of the COVID-19 pandemic in Ontario’s LTC homes, from March 17 to August 31, 2020, 34.0% (212/626) of LTC homes experienced COVID-19 outbreaks, resulting in 6,036 resident cases and 1,815 resident deaths. Ontario LTC home residents accounted for 64.5% (1,815/2,812) of the province’s COVID-19 deaths, the highest proportion among 16 other Organisation for Economic Co-operation and Development (OECD) countries (Figure 2).7–9
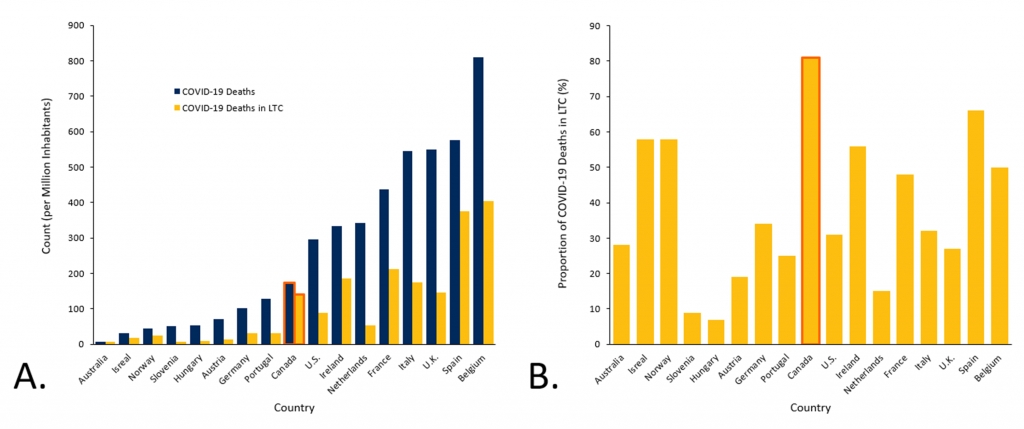
Bar graph A presents COVID-19 deaths among 16 OECD countries per million inhabitants as of May 25, 2020 in the population and in LTC. Bar graphs B presents the proportion of COVID-19 deaths in LTC among all COVID-19 deaths in the population. Canada, at 81%, has the highest proportion of COVID-19 deaths in LTC among the 16 other OECD countries. Figure adapted from the Canadian Institute for Health Information (CIHI).7
From April 14 to June 29, 2020, Ontario LTC homes were mandated to report all LTC resident deaths to the Office of the Chief Coroner. However, this data did not include LTC staff deaths or LTC residents who died in hospital. From April 14 to June 29, 2020, there was an excess of 1,589 deaths in Ontario LTC homes, as compared with the 5-year historical average for the same time period (Figure 3).
A study analyzing mortality in Ontario using cremation data reported an 89% increase in LTC home resident cremations in April 2020 compared to the month of April in the 2017-2019 period.10
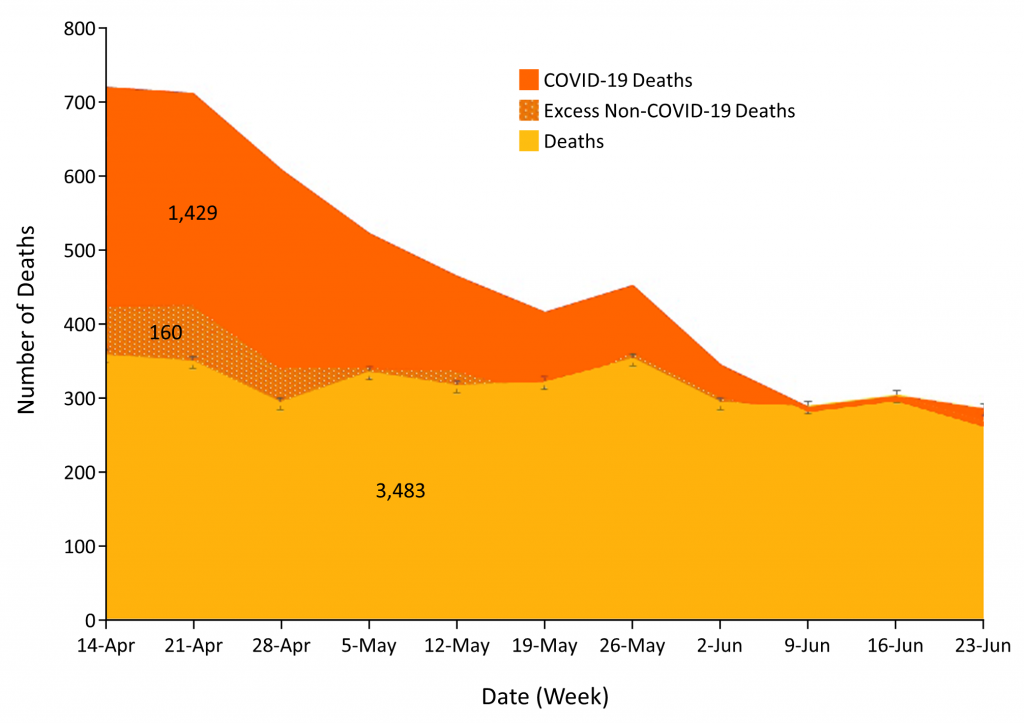
Graph presenting the excess mortality in Ontario’s LTC homes between April 14 and June 29, 2020. Excess mortality refers to the deaths beyond what would be expected in the absence of the COVID-19 pandemic, indicating the potential burden of mortality of the COVID-19 pandemic. Between April 14 and June 29, 2020, there was an excess of 1,589 deaths in Ontario’s LTC sector. Of these deaths, 1,429 were COVID-19 deaths. While the remaining 160 excess deaths were not COVID-19 deaths, they may be indirectly attributed to COVID-19 and the COVID-19 pandemic. Figure adapted from the Capacity Planning and Analytics Division, Ontario Ministry of Health (Kamil M, personal communication).
As of September 1, 2020, the beginning of the second wave in Ontario, the COVID-19 pandemic has been accelerating within LTC homes: 61% (4,321/7,090) of second wave resident cases and 68% (846/1,237) of second wave resident deaths have occurred between December 1, 2020 and January 14, 2021 (Figure 4). As of January 14, 2021, there have been 3,211 resident deaths, totaling to 60.7% of all 5,289 Ontario COVID-19 fatalities, and ten LTC worker deaths.
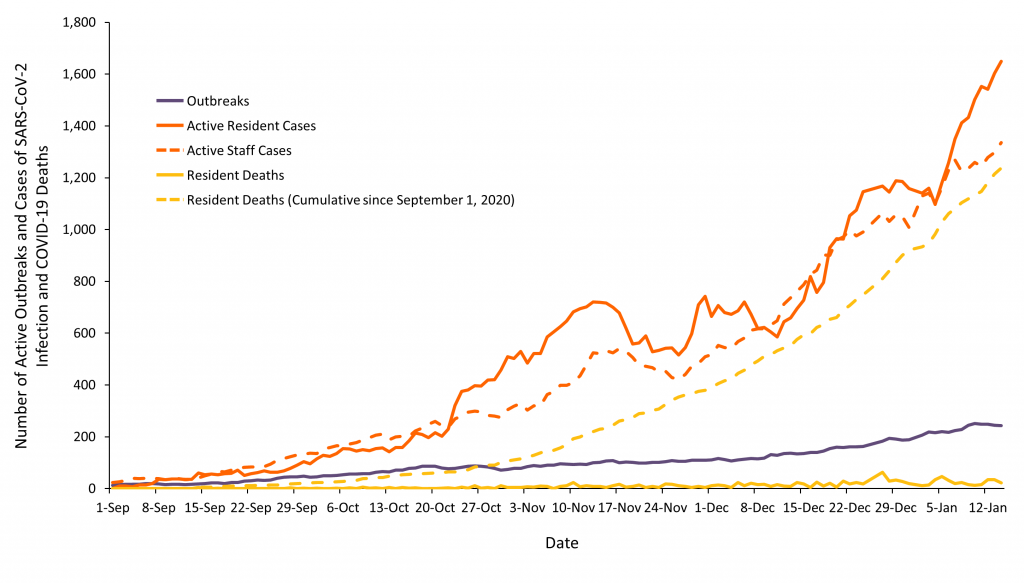
Graph presenting the number of active COVID-19 outbreaks, active cases of SARS-CoV-2 infection among staff and resident in Ontario LTC homes, and COVID-19 deaths among residents in Ontario LTC homes, between September 1 and January 14, 2021. Data from the Government of Ontario’s Long-Term Care Home COVID-19 Data, extracted January 18, 2021.11
The first and second waves of the COVID-19 pandemic are distinct. More LTC home residents were infected in the first wave compared to community-dwelling adults aged 70 years and older, with the opposite phenomenon occurring in the second wave (Figure 5). Provincial SARS-CoV-2 testing capacity has improved, resulting in both improved and earlier case detection in the second wave. Finally, there is incomplete follow-up in the second wave due to the currently active LTC home outbreaks and unresolved resident COVID-19 cases.
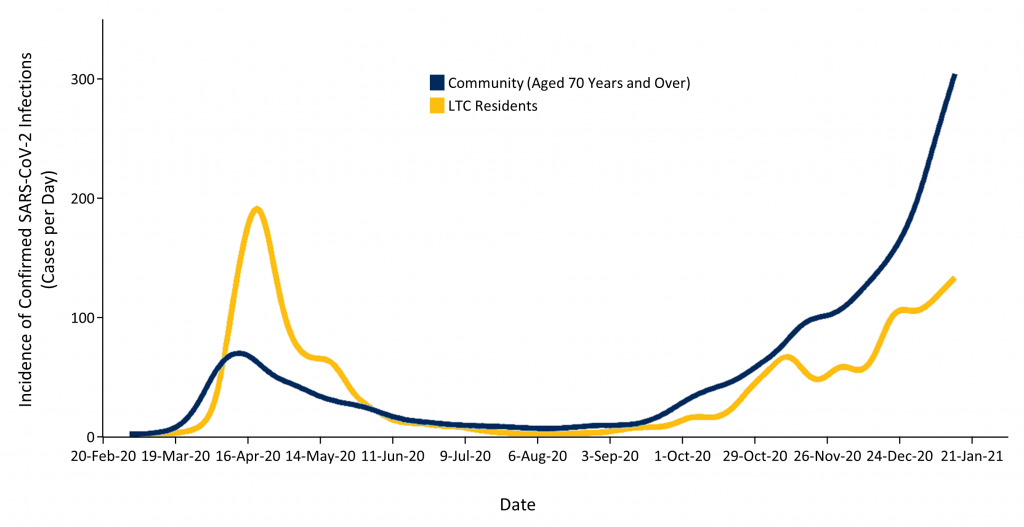
Graph presenting the daily incidence of confirmed SARS-CoV-2 infections in Ontario among community-dwelling residents aged 70 years and older and LTC home residents, from March to January 2021. The date is based on the date of reporting. Data sourced from the Case and Contact Management System (CCM Plus). Note that the number of community-dwelling adults aged 70 years and over (n= 1.7 million) is more than 20 times higher than the number of LTC residents (n= ~75,000). Therefore, the risk of confirmed SARS-CoV-2 infection is dramatically higher in LTC residents as compared with community-dwelling adults aged 70 years and over. Figure adapted from Public Health Ontario.12,13
With these differences in mind, the emerging data comparing the first and second waves reveals notable differences in key indicators in the LTC sector.
Compared to the first wave, the SARS-CoV-2 infection rate among LTC residents has been lower (Figure 6), and its doubling time has been longer (Figure 7) in the second wave. An increased doubling time indicates a slower growth rate of infections.
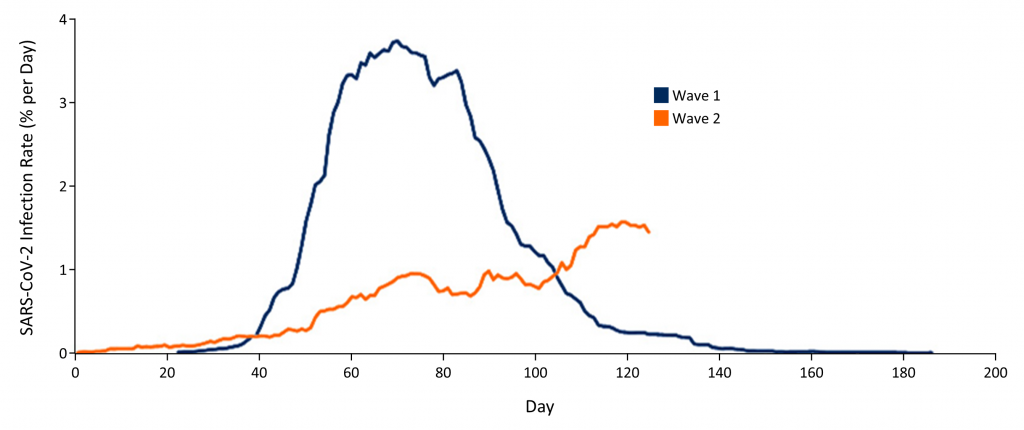
Graph presenting the rate of confirmed SARS-CoV-2 infections per day among LTC home residents in Ontario. Day 0 for Wave 1 is February 26, 2020; however, data collection began from March 17, 2020. Day 0 for Wave 2 is September 1, 2020. On January 6, 2021, the Wave 2 infection rate is higher than the Wave 1 infection rate. As of January 6, 2021, the Wave 1 maximum infection rate is higher than the Wave 2 maximum infection rate, but the Wave 1 infection rate peaked after 70 days, while the Wave 2 infection rate continues to increase until the time of publication of this Science Brief. Data sourced from the integrated Public Health Information System (iPHIS), extracted December 16, 2020. Figure adapted from Malikov K (personal communication).
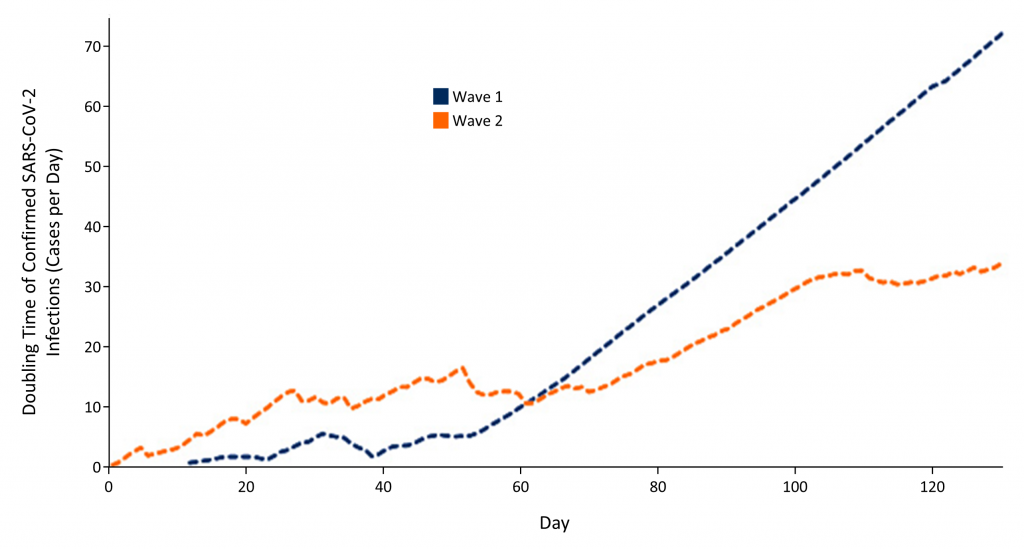
Graph presenting an analysis of the doubling time of SARS-CoV-2 infections among LTC home residents in Ontario. Day 0 for Wave 1 is February 26, 2020, however, data collection began from March 17, 2020. Day 0 for Wave 2 is September 1, 2020. The Wave 1 and Wave 2 doubling time curves cross at day 60, indicating that the growth rate of SARS-CoV-2 infections among LTC residents after 60 days from the onset of each wave is faster in Wave 2. Data sourced from the integrated Public Health Information System (iPHIS), extracted January 6, 2021. Figure adapted from Malikov K (personal communication).
There has also been a faster rate and greater number of LTC home COVID-19 outbreaks involving residents in the first wave, as compared to the second wave (Figure 8).
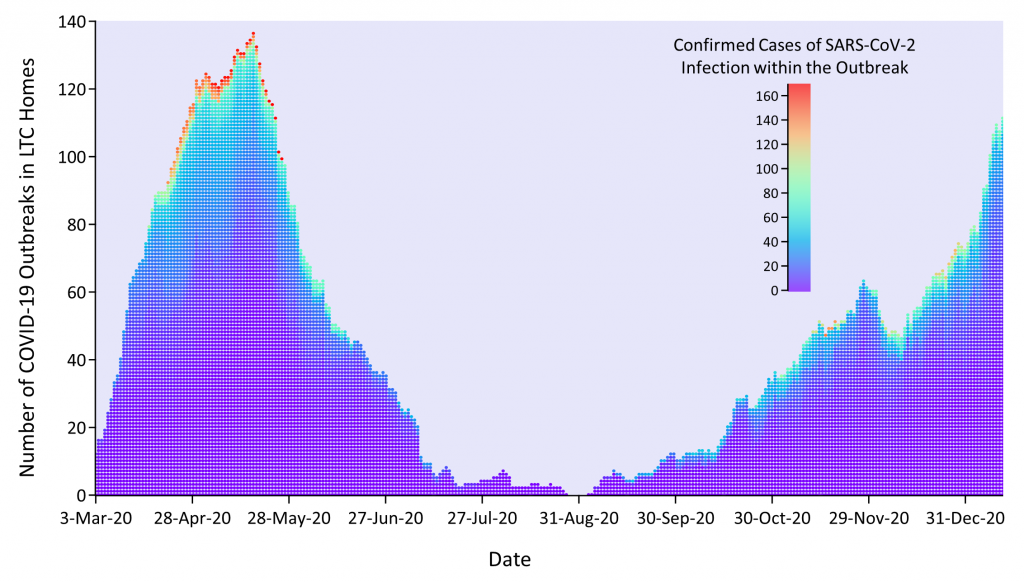
Graph presenting the number of COVID-19 outbreaks and number of SARS-CoV-2 infections within each outbreak in Ontario’s LTC homes, from March 29 to January 13, 2021. Presented outbreaks involve at least one LTC home resident. The date is based on the date of reporting. There are fewer outbreaks in the second wave that involve more than 100 cases of confirmed SARS-CoV-2 infections. Data sourced from the integrated Public Health Information System (iPHIS), extracted January 13, 2021. Figure adapted from Malikov K (personal communication).
The COVID-19 case fatality rate among LTC home residents over the first 127 days of the first and second waves has improved from 32.7% in the first wave to 17.4% in the second wave (Figure 9).
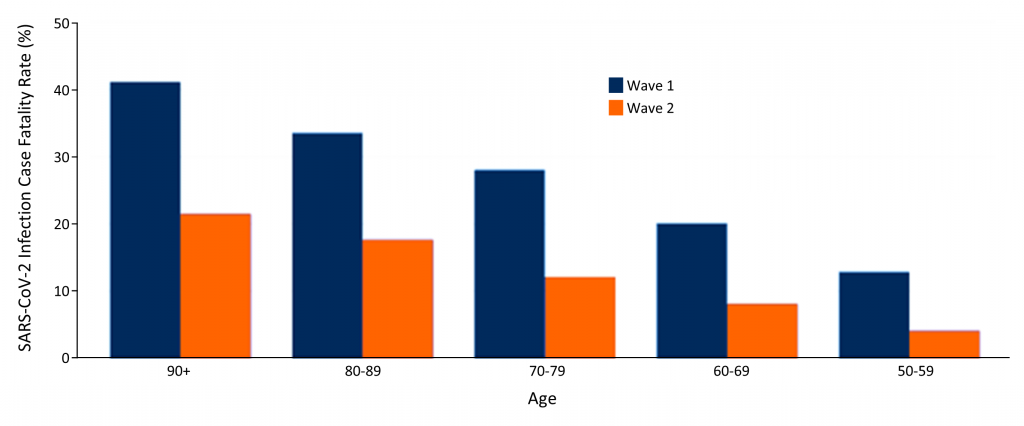
Bar graph presenting case fatality rates of confirmed SARS-CoV-2 infections among Ontario LTC home residents by age group. Wave 1 case fatality rates are from February 26to May 28, 2020. Wave 2 case fatality rates are from September 1 to January 6, 2021. Data sourced from the integrated Public Health Information System (iPHIS), extracted January 6, 2021. Figure adapted from Malikov K (personal communication).
This observed improvement is likely multifactorial in cause: As the pandemic progresses, there is now a much clearer understanding of asymptomatic and pre-symptomatic spread of SARS-CoV-2 infection, as well as atypical presentations of COVID-19, which are more common among LTC home residents.14–16 There is better access to SARS-CoV-2 testing and personal protective equipment (PPE), which were both severely restricted at the onset of the first wave in the LTC sector. Most homes have now implemented more robust IPAC measures, including universal masking of staff and enabling them to work at only one healthcare setting.17 There has also been an intensification of efforts to manage residents with SARS-CoV-2 infection in LTC homes, with interventions such as supplemental oxygen, subcutaneous hydration, and dexamethasone therapy.18–20 Finally, the LTC sector now receives greater attention, focus, and coordination in the overall provincial pandemic response, including the formation of acute care hospital partnerships in late April 2020, which may have improved access to hospitalization for LTC residents.20–22
An analysis of hospitalizations among all Ontarians who died of COVID-19 from March to November 2020 revealed that only a small proportion of Ontario LTC home residents were hospitalized prior to death. There were also substantial temporal variations, with hospitalizations paradoxically reaching their lowest point when the overall incidence of SARS-CoV-2 infections peaked in April, 2020 (Table 1).23 While many LTC home residents may have had pre-pandemic plans of care indicating that they should not be sent to an acute care hospital, the low admission rate of 15.5% observed between March and April 2020 was in contrast to higher admission rates of greater than 30% in subsequent months and comparatively stable admission rates among community-dwelling adults (Figure 10).
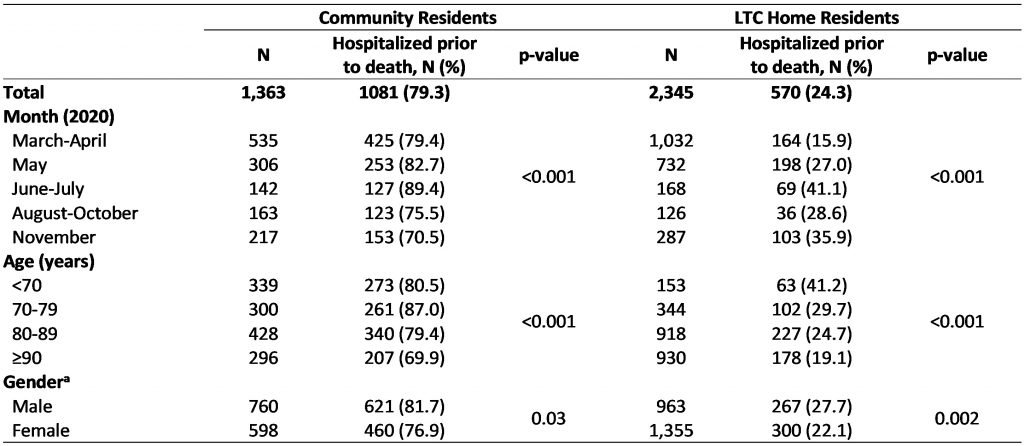
Table presenting hospital admissions prior to COVID-19 death among community and LTC home residents, from March to November 2020. aDeaths with unknown gender are not presented below due to small cell counts. Table adapted from Brown et al. medRxiv. 2020.23 The p-values are for differences across periods, age and gender.
There were also notable sex-based differences, with women dying of COVID-19 being less likely to receive hospitalization compared to men in both community (76.9% women vs 81.7% men) and LTC home (22.1% women vs 27.7% men) settings. These sex-based differences are consistent with earlier Ontario and international findings reporting increased rates of hospitalization among older men compared to older women.24,25 Further, the observed sex- and gender-based differences in end-of-life care for Ontario LTC home residents dying of COVID-19 are consistent with pre-pandemic evidence reporting that male residents with advanced dementia are much more likely than female residents to be transferred to hospital in their last 30 days of life.26
Overall, the findings of this analysis substantiate reports suggesting that hospitalizations for LTC home residents with COVID-19 were low during the peak of the pandemic’s first wave, which may have contributed to the particularly high COVID-19 mortality in Ontario’s LTC homes.
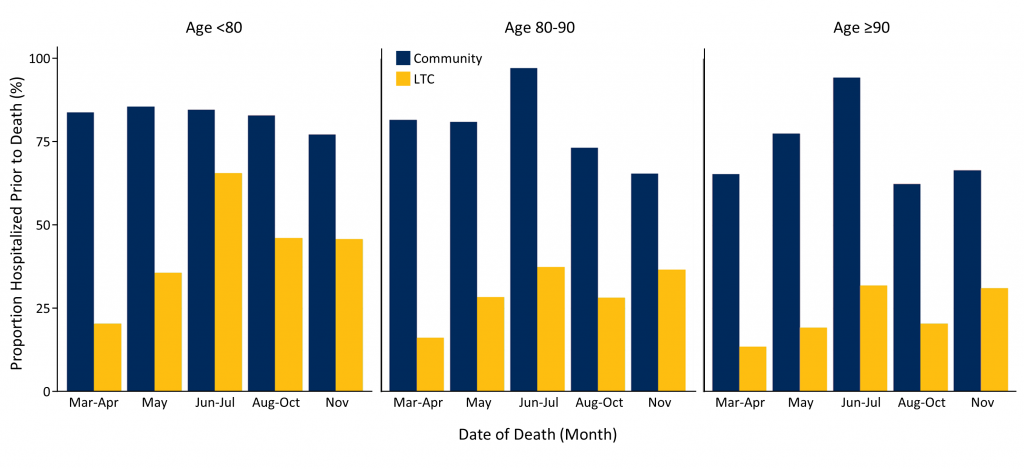
Bar graph presenting the proportion of hospitalization prior to COVID-19 death among community and LTC home residents by age group, from March through November 2020. Figure adapted from Brown et al. medRxiv. 2020.23
Risk Factors for COVID-19 Outbreaks and Resident Deaths in Ontario’s LTC Homes
The risk of COVID-19 outbreaks in LTC homes is strongly associated with the rate of SARS-CoV-2 infection in the communities surrounding them. However, the temporal relationship between rising rates of SARS-CoV-2 infection in the community and the risk threshold for subsequent LTC home outbreaks is not well defined.27,28
A population-based cohort study of all Ontario COVID-19 cases between March 1 and July 16, 2020 evaluated the temporal relationship between trends in the number of active community COVID-19 cases and the number of LTC home outbreaks.29 The average lag time between community cases and LTC home outbreaks was 23 days for Ontario overall, with substantial variability across geographic regions, ranging from 11 to 43 days (Figure 11). The longest lag was observed in the North Region, which has a low population density and reported a lower cumulative COVID-19 incidence of 0.3% in LTC home residents, compared to the provincial average of 7.5% over the study’s time period.
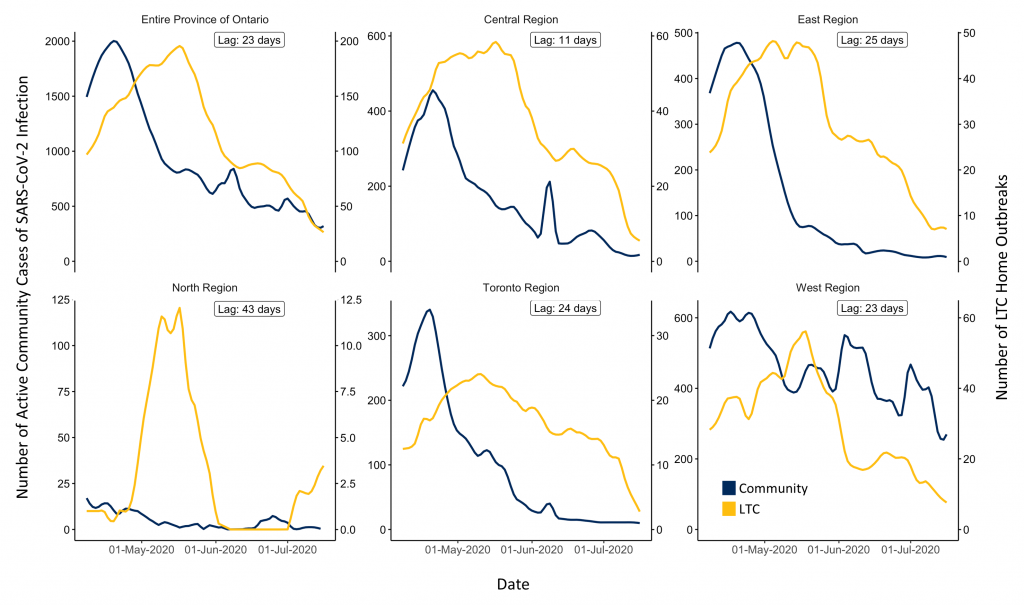
Graphs presenting the daily incidence of confirmed SARS-CoV-2 infections within communities and COVID-19 outbreaks in LTC homes in Ontario by region, from April 8 to July 16, 2020. Includes data on 623 LTC homes in Ontario. Lag refers to the lag time between community cases and LTC home outbreaks. Figure adapted from Malikov et al. medRxiv. 2020.29
The analysis also determined the levels of community incidence associated with a 75% probability of observing a LTC home outbreak within 5 days. For the province overall, a daily incidence of 2.30 SARS-CoV-2 infections per 100,000 inhabitants was associated with a 75% probability of a LTC home outbreak occurring five days later (Table 2).
The lag days estimate is a useful early warning indicator for surveillance systems, and provides a time window—23 days for Ontario overall—during which the LTC sector should rapidly mobilize and intensify occupational health and IPAC processes to both prevent and mitigate COVID-19 outbreaks, following an observed rise in community infections. The reported thresholds for community infections at which outbreaks in LTC homes first occur are useful both for guiding broader public health interventions to targeting community transmission—such as the province’s tiered response framework—and for guiding policies based on community incidence of SARS-CoV-2 infections that concern visitors to LTC homes as well as resident absences and congregate activities such as dining.30,31
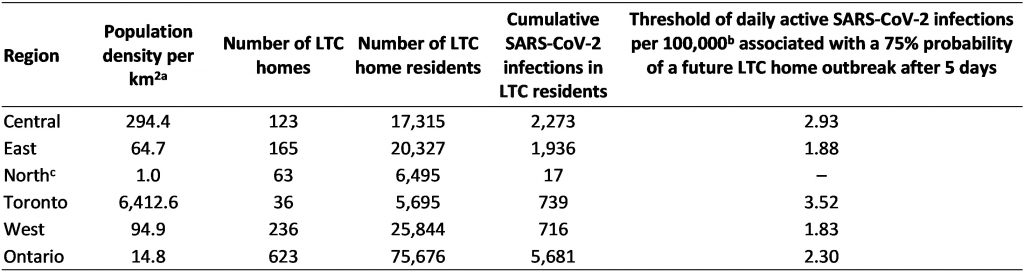
Table presenting characteristics of Ontario’s LTC homes and thresholds for community incidence of SARS-CoV-2 infections associated with a 75% probability of LTC home outbreaks after 5 days, from March 1 to July 16, 2020. aData sourced from Ontario Ministry of Finance, based on 2016 Canadian Census.32 bDaily active SARS-CoV-2 infections in the community per 100,000 inhabitants. cThreshold calculations for the North Region were suppressed due to the small numbers of reported cases and small population size. 623 of Ontario’s LTC homes are included. Table adapted from Malikov et al. medRxiv. 2020.29
The relationship between community incidence of SARS-CoV-2 infections and LTC home outbreaks is likely mediated by infected staff who are unknowingly importing virus in homes with asymptomatic or pre-symptomatic COVID-19.33,34 An Ontario study conducted in the early days of the first wave of the COVID-19 pandemic, from March 29 to April 7, 2020, reported that infection among LTC staff was associated with death among residents with a 6-day lag (Figure 12).35
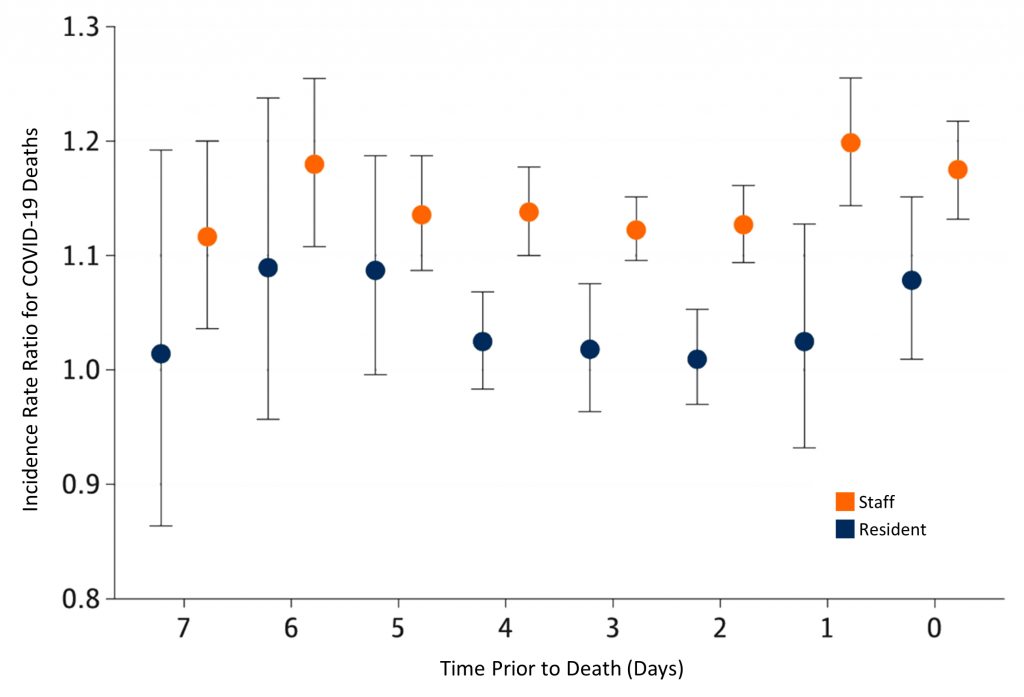
Graph presenting the incidence rate ratios for COVID-19 deaths by lagged confirmed SARS-CoV-2 infections among LTC residents and staff in Ontario, from March 29 to April 7, 2020. Circles represent incidence rate ratios. Vertical lines represent 95% confidence intervals (CI). An elevated risk of COVID-19 death is observed at all lag times after SARS-CoV-2 infection among LTC staff. Figure adapted from Fisman et al. Jama Netw Open. 2020.35
Additional Ontario studies from the first wave of the pandemic confirm that community incidence of SARS-CoV-2 infections is the strongest predictor of whether a LTC home is going to experience a COVID-19 outbreak.36,37
An earlier retrospective cohort study examining the impact of for-profit status on COVID-19 outcomes in 623 Ontario LTC homes, from March 29 to May 20, 2020, found that for-profit status had no significant association with the risk of outbreaks. However, the study found that each additional cumulative COVID-19 case per 1,000 individuals in the public health unit region surrounding the LTC care home was associated with nearly double the odds of an outbreak (adjusted odds ratio (OR) 1.91, 95% confidence interval (CI) 1.19–3.05).36
Homes with for-profit status had outbreaks with nearly twice as many residents infected (adjusted risk ratio (RR) 1.96, 95% CI 1.26–3.05) and 78% more resident deaths (adjusted RR 1.78, 95% CI 1.03–3.07), compared with non-profit homes.
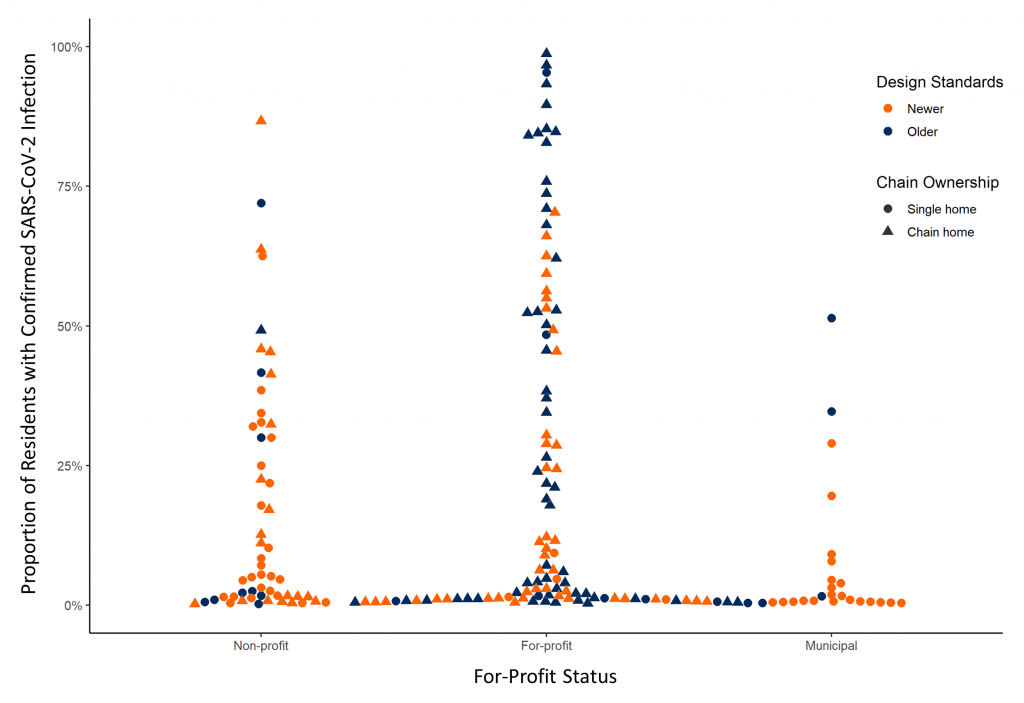
Graph presenting the extent (i.e. the percentage of confirmed SARS-CoV-2 infections among residents of a LTC home) of COVID-19 outbreaks in Ontario LTC homes by profit status, from March 29 to May 20, 2020. Homes with older design standards and chain ownership, which are more common among for-profit status homes, had the highest proportion of LTC residents with confirmed SARS-CoV-2 infections. Figure adapted from Stall et al. CMAJ. 2020.36
These associations were largely explained by the higher proportion of older design standards that meet or fall below design standards established in the year 1972, and chain ownership in homes with for-profit status (Figures 13 and 14).
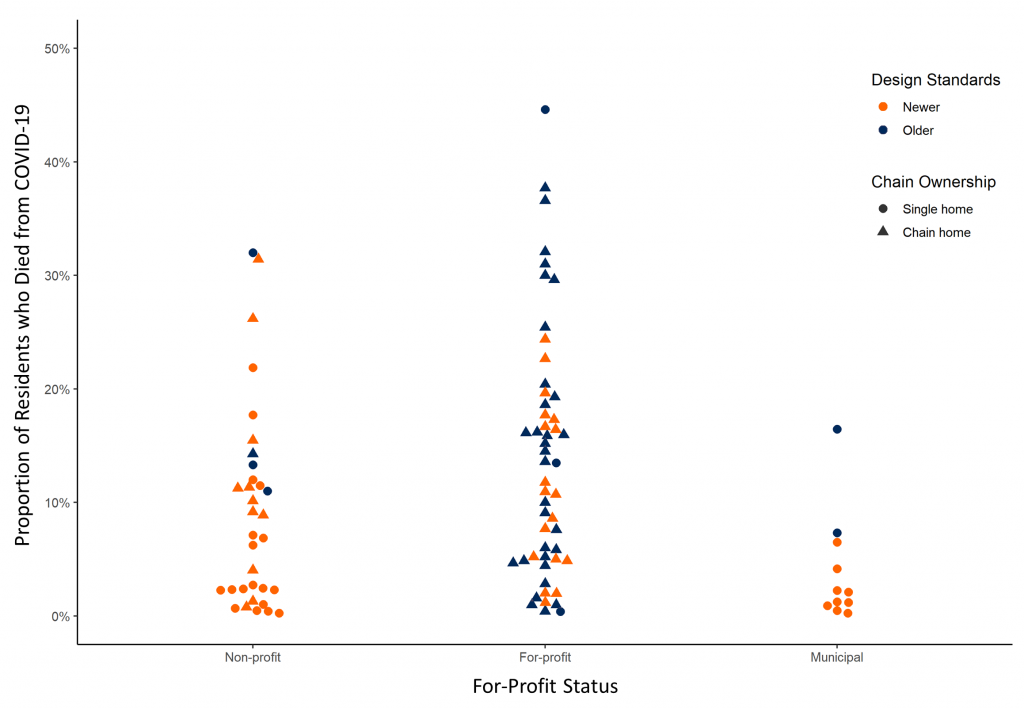
Graph presenting the percentage of COVID-19 deaths among LTC homes in outbreak by profit status in Ontario, from March 29 to May 20, 2020. Homes with older design standards and chain ownership, with are more common among for-profit status homes, had the highest proportion of LTC residents with confirmed SARS-CoV-2 infections. Figure adapted from Stall et al. CMAJ. 2020.36
Another retrospective population-based cohort study examined the association between LTC home crowding and SARS-CoV-2 infection and COVID-19 mortality in Ontario LTC homes from March 29 to May 20, 2020.37 As of March 29, 2020 there were 78,607 resident beds in Ontario’s LTC homes, with 36.9% in single-bedded rooms, 37.3% in double-bedded rooms, and 25.8% in quadruple-bedded rooms. 50.1% (310) of LTC homes had low crowding and 49.9% (308) of LTC homes had high crowding according to a crowding index (Figure 15).
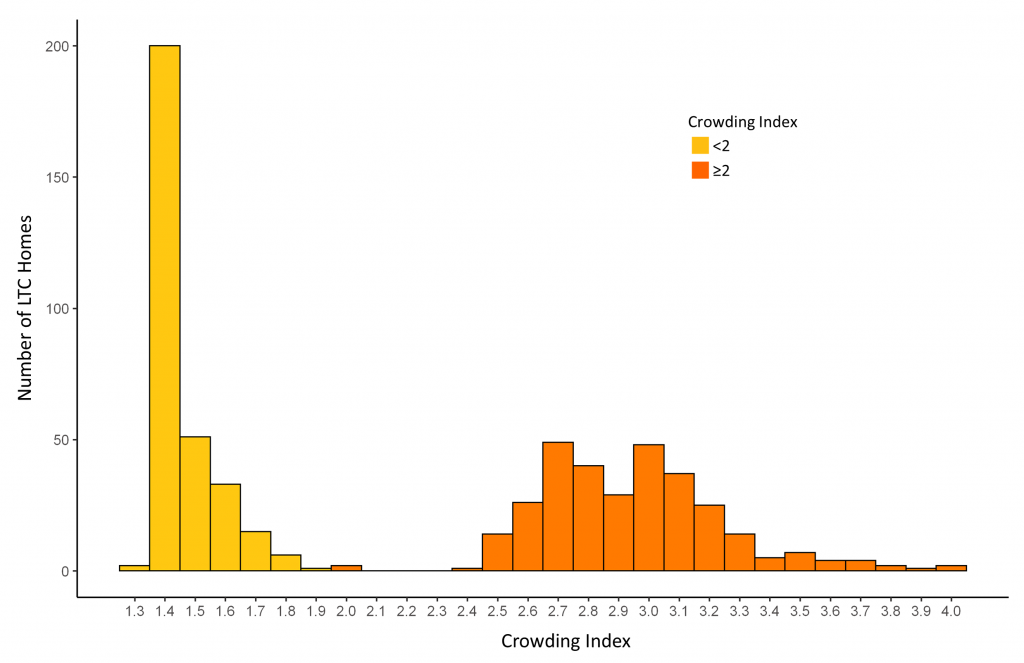
Bar graph presenting the distribution of Ontario LTC homes by crowding index across 618 LTC homes, as of March 29, 2020. The crowding index for Ontario’s LTC homes was derived by calculating the mean number of occupants per room and bathroom across an entire LTC home (Number of residents ÷ (½ Number of bedrooms + ½ Number of bathrooms)). Homes with a crowding index of less than 2 were defined as having low crowding, while homes with a crowding index greater or equal to 2 were defined as having high crowding. Figure adapted from Brown et al. JAMA Intern Med. 2020.37
As of May 20, 2020, SARS-CoV-2 infections were distributed unequally across Ontario’s LTC homes, with 86% (4,496) of infections occurring in just 10% (63) of homes. The incidence of SARS-CoV-2 infections in highly crowded homes was 9.7%, while the incidence of SARS-CoV-2 infection in less crowded homes was 4.5% (p-value < 0.001). Similarly, mortality was 2.7% in highly crowded homes and 1.3% in less crowded homes (p < 0.001).
The probability of SARS-CoV-2 infection introduction into a home did not differ according to the crowding index, with 31.3% in high crowding homes and 30.2% in low crowding homes (p = 0.79). Outbreaks in crowded LTC homes were also larger: 90% of the province’s LTC outbreaks involving more than 100 infected residents occurred in high crowding homes, as compared with only 10% that occurred in low crowding homes (Figure 16).
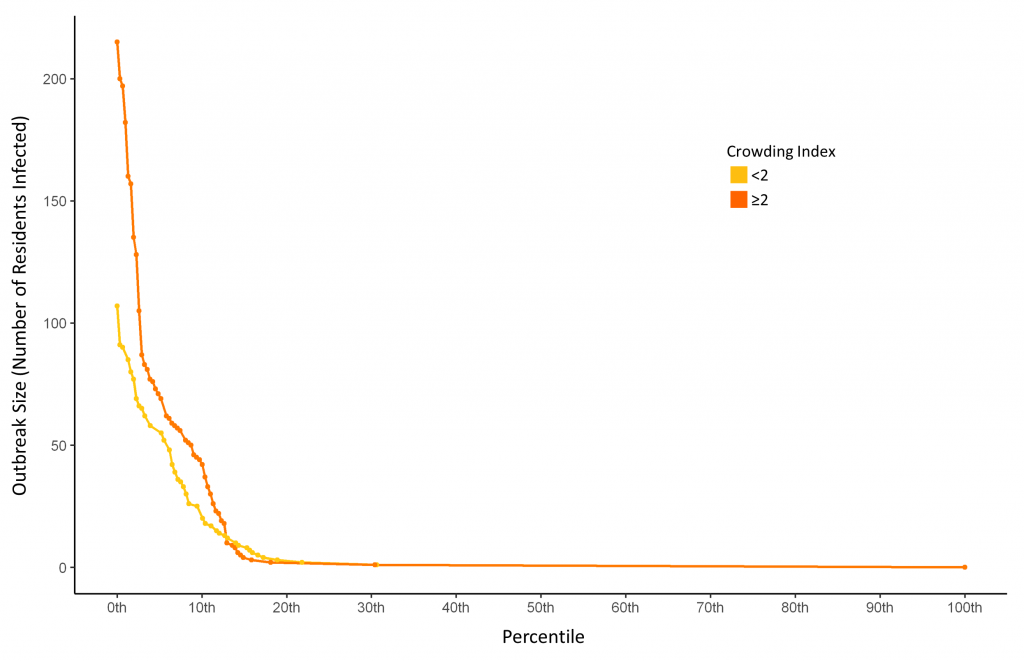
Graph presenting the size of COVID-19 outbreaks and percentile rank of outbreak size in Ontario LTC homes by crowding index, from March 29 to May 20, 2020. Includes 618 Ontario LTC Homes. The crowding index for Ontario’s LTC homes was derived by calculating the mean number of occupants per room and bathroom across an entire LTC home (Number of residents ÷ (½ Number of bedrooms + ½ Number of bathrooms)). Homes with a crowding index of less than 2 were defined as having low crowding, while homes with a crowding index greater or equal to 2 were defined as having high crowding. Nine out of the 10 largest outbreaks involving more than 100 residents occurred in LTC homes with a crowding index ≥2 (orange curve). Figure adapted from Brown et al. JAMA Intern Med. 2020.37
Unadjusted and adjusted regression models based on the crowding index suggested that, compared to a home with an index of 1.5, homes with an index of 3 had nearly double the incidence of SARS-CoV-2 infection (RR, 2.05; 95% CI, 1.49-2.70; adjusted RR, 1.73; 95% CI, 1.10-2.72) and COVID-19 mortality (unadjusted RR, 1.97; 95% CI, 1.36-2.84; adjusted RR, 1.69; 95% CI, 0.99-2.78) (Figure 17). The crowding index was not associated with the probability of introduction of SARS-CoV-2 infection in to a LTC home, with the incidence of SARS-CoV-2 infection in the region surrounding a LTC home remaining the most important predictor.
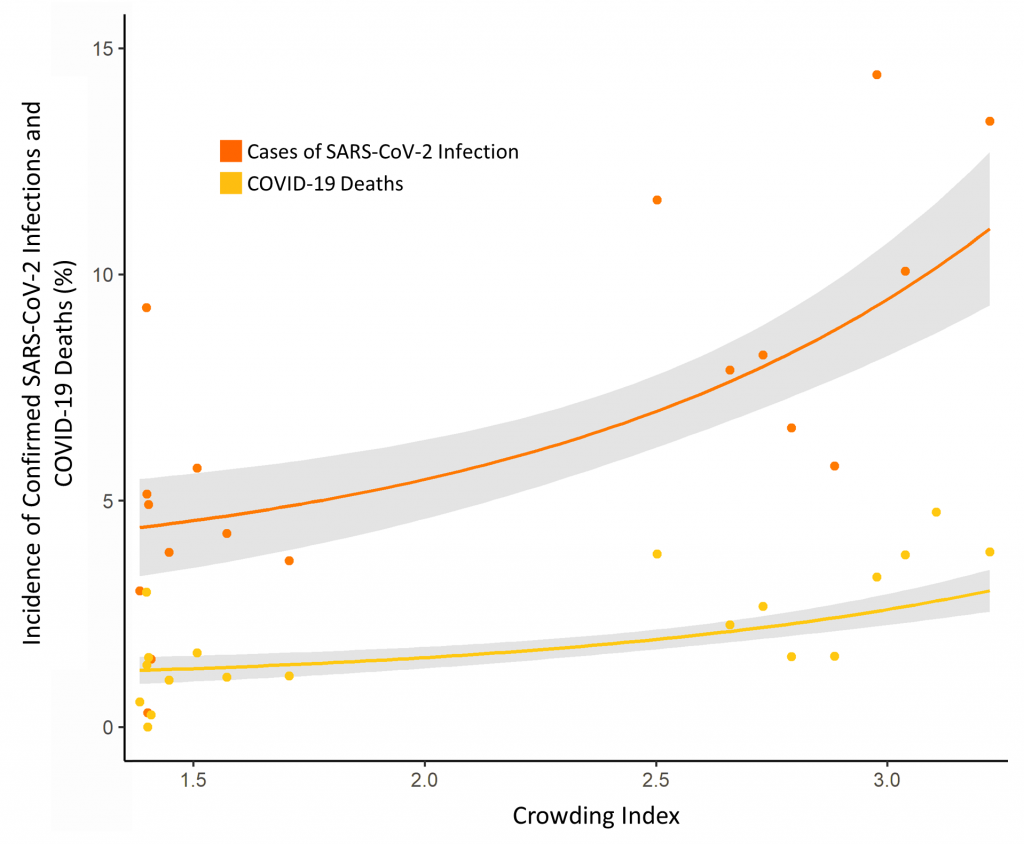
Graph presenting the incidence of SARS-CoV-2 infections and COVID-19 deaths in Ontario LTC homes by crowding index, March 29 to May 20, 2020. Grey area represents the 95% confidence interval (CI). The crowding index for Ontario’s LTC homes was derived by calculating the mean number of occupants per room and bathroom across an entire LTC home (Number of residents ÷ (½ Number of bedrooms + ½ Number of bathrooms)). Homes with a crowding index of less than 2 were defined as having low crowding, while homes with a crowding index greater or equal to 2 were defined as having high crowding. Figure adapted from Brown et al. JAMA Intern Med. 2020.37
Simulations suggested that 19.1% (998) of infections and 18.1% (263) of deaths in Ontario LTC homes may have been prevented if quadruple-bedded rooms had been converted to double-bedded rooms. In this simulation scenario, an additional 5,070 double-bedded rooms would have been needed to maintain capacity across the province of Ontario. In a simulation where all multiple-occupancy rooms were converted to single-occupancy rooms, it was estimated that 31.4% (1,641) infections and 30.1% (437) deaths may have been prevented. In this scenario, an additional 29,871 new single-occupancy rooms would have been required.37
Taken together, evidence from Ontario suggests that the risk factors for COVID-19 outbreaks are distinct from the risk factors for spread of SARS-CoV-2 infection and COVID-19 deaths within a home. The most important risk factors for whether a LTC home is going to experience a COVID-19 outbreak is the community incidence of SARS-CoV-2 infection surrounding a LTC home and staff SARS-CoV-2 infection.29,35 The most important risk factors for the size of a LTC home COVID-19 outbreak and the number of resident deaths are for-profit status and crowding. For-profit homes have a higher proportion of older design standards and chain ownership and crowded homes have an increased number of residents per room and bathroom (Figure 1).36,37
Impact of the COVID-19 Pandemic on the Health and Wellbeing of LTC Residents
In response to an intensifying COVID-19 crisis in Ontario LTC homes, Ontario implemented strict bans on visitors in mid-March 2020, with the goal of preventing the introduction of SARS-CoV-2 infection into the homes.17 These measures resulted in the immediate restriction of visitors, volunteers and non-essential personnel from entering LTC homes, which restricted entry for family caregivers who provide direct, complex, intense, and unpaid care for many LTC home residents.38–40
Additional restrictions resulted in the cancellation of group activities, communal dining and restricted residents from leaving the property of LTC homes, even for short walks and fresh air. As a result, countless LTC home residents experienced severe and potentially irreversible harm, with many sustaining physical, cognitive, psychological and functional declines.41–45 This constellation of resident clinical issues associated with restrictive IPAC measures in LTC homes has been termed “confinement syndrome”, a term appropriated from the medical literature describing the symptoms experienced by persons placed in solitary confinement from intense anxiety and sensory deprivation.46,47
One common concern regarding the mental health of LTC home residents during the COVID-19 pandemic is the increase in the use of psychoactive medications, which were frequently overprescribed prior to the pandemic.43,48 A previous report documented increased prescribing of antipsychotics during the COVID-19 pandemic to people living with dementia in the United Kingdom.49 A population-based study of all Ontario LTC home residents, found that prescribing of psychoactive drugs started in March 2020 during the onset of COVID-19 outbreaks and public health restrictions in LTC homes, which persisted through September 2020 (Figure 19). Increases in prescribing were out of proportion to expected trends over time, and distinct from observed prescribing changes in other drugs during the pandemic (Figure 19).50
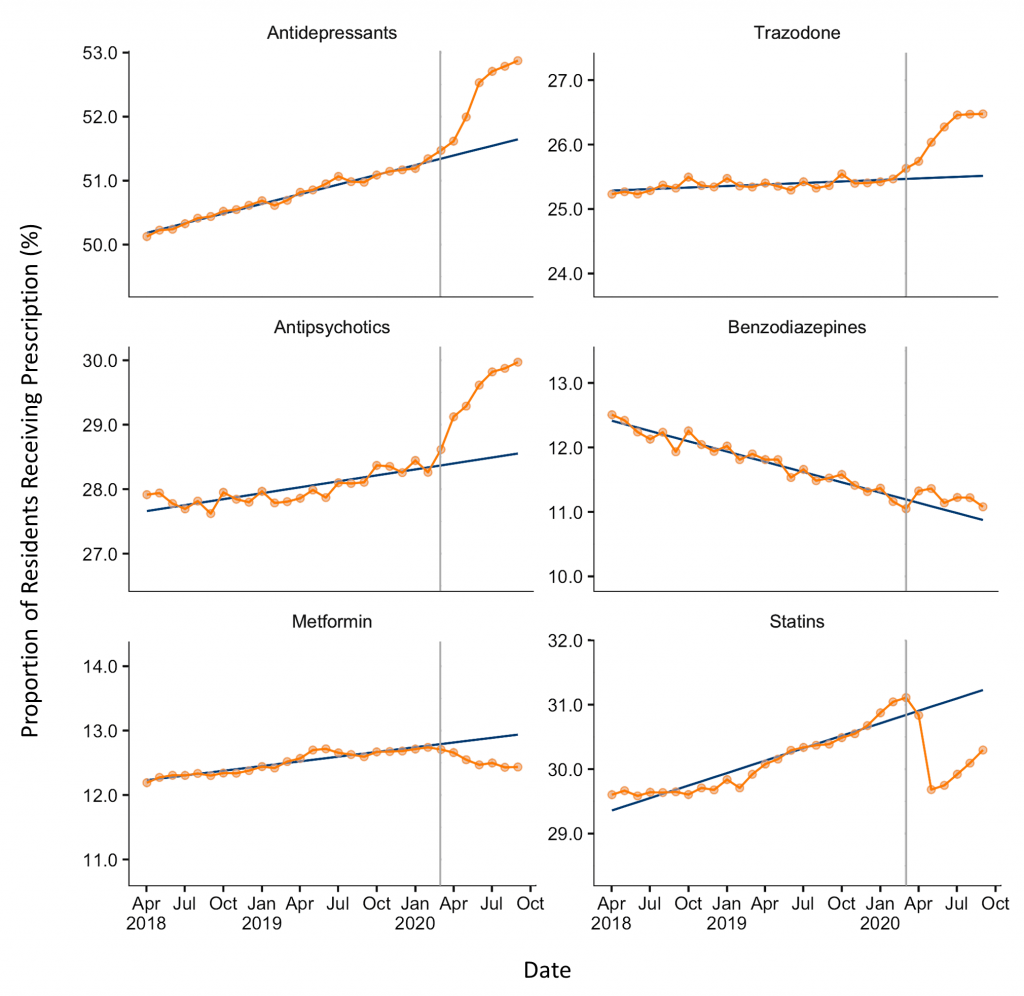
Graphs presenting the monthly proportion of Ontario LTC home residents who were dispensed a prescription by psychoactive drug class, from April 2019 through September 2020. The grey vertical lines represent the beginning of the COVID-19 lockdown in Ontario in March 2020. The blue line represents expected monthly proportion of psychoactive prescriptions in Ontario LTC homes by drug class, based on the trends over time of each drug class in Ontario prior to the March 2020 lockdown. Figure adapted from Stall et al. medRxiv. 2020.50
Ontario Evidence to Support Public Health Interventions and Policy in LTC Homes
The accumulating evidence on COVID-19 in Ontario’s LTC homes has been leveraged in several ways to support public health interventions and policy during the pandemic. The early recognition in Ontario that SARS-CoV-2 infections in LTC staff were associated with COVID-19 death among residents, and complementary evidence from other regions, motivated a public order implemented on April 22, 2020, restricting employees of LTC homes from working in more than one LTC home, congregate care, or healthcare setting within a 14-day period.17,35,51,52 This order came several weeks after similar ones in other jurisdictions like British Columbia, and did not apply to temporary agency staff or other contract staff who are not employees of LTC homes, to ensure LTC homes had available staff to work on an emergency basis.53,54
An Ontario study examined the impact of this public policy by using anonymized mobile device location data to study the number of connections between all LTC homes during the seven weeks before and the seven weeks after the single-site work order.55 In the period preceding the order, 42.7% (266) of LTC homes had a connection with at least one other home, compared to 12.7% (79) of homes during the period after restrictions, a drop of 70.3% (p<0.001) (Figure 20). The average number of connections per home in the period before the order was 3.90, compared to 0.77 connections in the period after the order, a drop of 80.3% (p<0.001). In both periods, mobility between LTC homes was higher in homes located in larger communities, those with higher bed counts, and those part of a large chain.
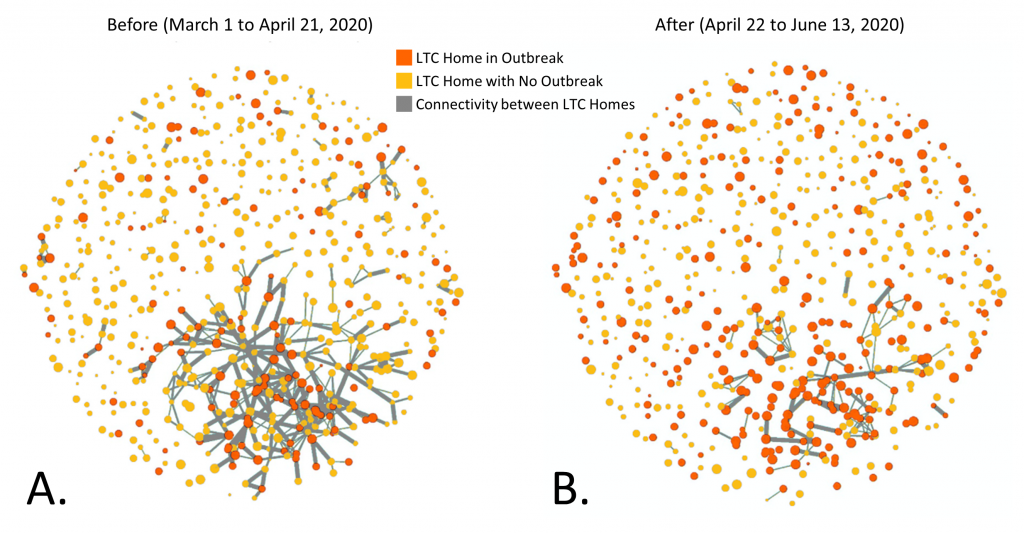
Network connectivity diagrams presenting connectivity and outbreaks in Ontario LTC homes, from March 1 to June 13, 2020. Diagram A presents the period of 7 weeks before the implementation of an order which limited LTC homes staff from working in other LTC of healthcare settings within a 14-day period, from March 1 to April 21, 2020. Diagram B presents the period of 7 weeks after the implementation of the order, from April 22 to June 13, 2020. The grey lines represent connections between LTC homes, which thicker lines representing more connections, and thinner lines representing fewer connections. In the 7 weeks after the implementation of the order in Ontario (diagram B) there is a significant reduction in connectivity between homes, as compared to the 7 weeks prior to the implementation of the order in Ontario (diagram A). Figure adapted from Jones et al. medRxiv. 2020.55
Documented risk factors for COVID-19 outbreaks, their size, and lethality, have been incorporated into provincial surveillance tools to identify and analyze higher risk LTC homes in the COVID-19 pandemic (Figure 21).
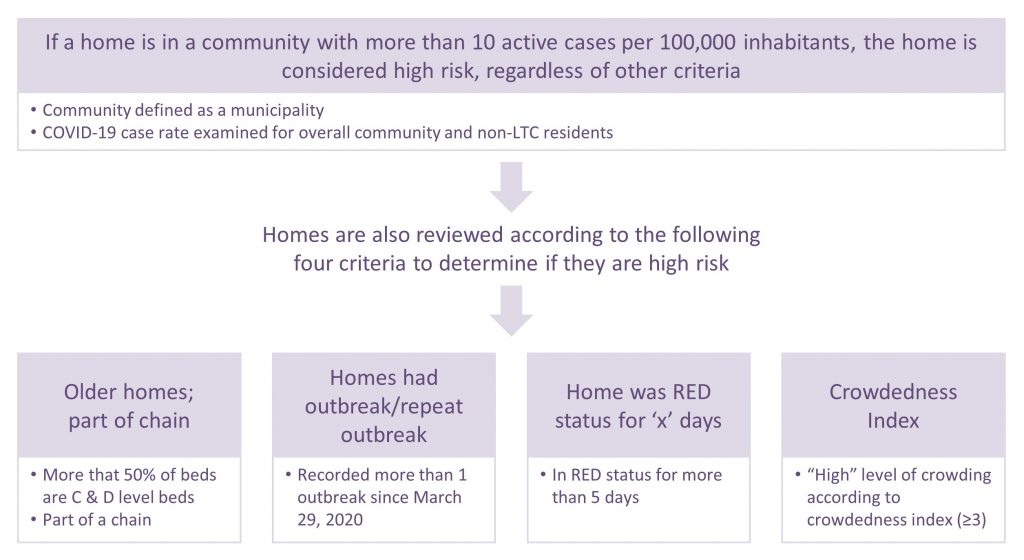
Figure adapted from the Capacity Planning and Analytics Division, Ontario Ministry of Health.56
The findings associating crowding with SARS-CoV-2 infections and COVID-19 deaths in LTC homes motivated revisions to provincial directives on resident admissions to LTC homes.37 A revision in June 2020 limited new resident admissions into rooms with more than two residents. In October 2020, it was further specified that “at any time, there should not be more than two (2) residents placed per room, including 3 or 4 bed ward rooms”.57
Recognizing the need to balance IPAC measures in LTC homes with resident wellbeing, and following guidance from several organizations, the Province of Ontario moved to update its LTC home visitor policy in early September 2020 to give greater access to family caregivers.58–64This allowed each resident and/or their substitute decision maker to designate a maximum of two caregivers who can visit a resident in LTC homes without time limits, including when a resident is infected with COVID-19 or when a LTC home is experiencing a COVID-19 outbreak.65 This policy aligns with emerging international evidence demonstrating the absence of evidence on the effectiveness of blanket visitor bans in reducing the introduction of SARS-CoV-2 infection in to LTC homes, and the relative safety of reintroducing family caregivers into LTC homes during the pandemic with appropriate IPAC procedures and access to PPE.66–69
Interpretation
The following are measures that could be effective in preventing COVID-19 outbreaks, hospitalizations, and deaths in Ontario’s LTC homes (Box 1).
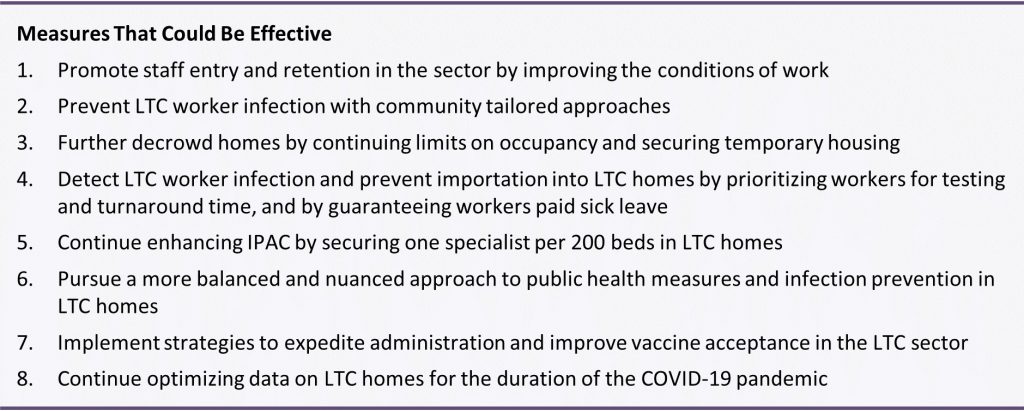
Promote Staff Entry and Retention in the Sector by Improving the Conditions of Work
The Ministry of Long-Term Care released a staffing study in July 2020 which emphasized that while the demand for LTC and resident acuity continues to increase in Ontario, staffing levels and access to appropriate training have not kept pace, resulting in a staffing crisis.3,5
The LTC sector has had difficulty retaining staff because of extremely demanding job responsibilities, stressful and poor work conditions, negative public image about working in the sector, and a lack of full-time job opportunities with fair pay and benefits. As of 2018, there were 50,000 PSWs employed in Ontario’s LTC sector sharing the equivalent of 32,700 full-time equivalent positions despite many staff wanting more full-time work.3 As a result, many PSWs need to work multiple part-time jobs to earn a living wage.3,70,71
The conditions of work within LTC homes and the difficulties in both promoting and retaining worker in the sector have been severely exacerbated by the COVID-19 pandemic.3 Many LTC home workers contracted SARS-CoV-2 infections themselves, with eight staff members dying of COVID-19 in the first wave and two staff members dying in the second wave to date. There is also a heightened fear among staff about onwards transmission of SARS-CoV-2 to family members, not having access to PPE given the shortages at the onset of the pandemic, and burnout given the stressful conditions many staff are exposed to in outbreak settings.3
Addressing the longstanding staffing shortages is one of the most urgent issues confronting Ontario’s LTC homes both during and in the wake of the COVID-19 pandemic.72 Research from the United States highlights how homes with lower levels of staffing experienced a greater incidence of SARS-CoV-2 infections and COVID-19 mortality.73,74
Recent commitments from the Government of Ontario, including temporary pay increases for LTC workers, return of service incentives, accelerated training programs, and increased hours of care per resident are promising for promoting staff entry and retention. However, many of these enhancements are temporary and are unlikely to end the current reliance on temporary staffing.75,76
Ontario’s LTC sector may benefit from extending these benefits beyond the COVID-19 pandemic, allowing the sector to minimize or eliminate staff mobility between homes and other workplaces during the COVID-19 pandemic. This could include creating more full-time jobs, more permanent pay increases, career ladders and more immediate increases in the hours of care being provided to each resident. Recent pre-budget commitments to increasing staffing levels to provide four hours of direct care per resident by 2024-25 are encouraging, but no definitive staffing strategy or accompanying financial commitment has been made to date.
Some LTC experts have suggested ensuring that a minimum of 70% of LTC staff work full-time in a single site, with the remaining 30% being permanent, part-time staff, thereby allowing homes to have flexibility in staff scheduling. Such a plan would still need to ensure all full-time and part-time staff have fair pay and benefits including paid sick leave.77
Prevent LTC Worker Infection with Community Tailored Approaches
As of 2018, approximately 90% of Ontario’s PSW workforce was female and 41% were visible minorities. Many of these LTC home workers reside in neighbourhoods with lower socioeconomic status, increased household density, and a greater number of frontline workers; these are all neighbourhood characteristics that increase the risk of SARS-CoV-2 infection.78 Research from the United States documents a clear relationship between staff neighbourhood characteristics and COVID-19 LTC home outbreaks, and the same phenomenon is likely to exist in Ontario.79
As our understanding of the COVID-19 pandemic has evolved, so too has our appreciation of the disproportionate impact the pandemic has incurred on under-served populations. There is now a greater recognition that a more robust community-based and tailored approach to public health measures is needed for individuals at higher risk of SARS-CoV-2 infection and burden of COVID-19, many of whom are frontline workers, racialized, living on low incomes and reside in crowded conditions.80 Indeed, “one-size-fits-all” public health interventions, such as stay-at-home orders, are disproportionately difficult for marginalized individuals to comply with, rendering them both ineffective and inequitable.80,81
A broad range of community tailored approaches have been proposed, including recommendations from Canada’s Chief Public Health Officer, such as: 1) enabling community health centres and local organizations to provide support and testing, 2) bottom-up approaches to gain and foster the trust of communities, including tailored communication and messaging, 3) individualized case management and support of households, and 4) top-down approaches at regional and provincial levels to support socioeconomically vulnerable households and communities (paid sick leaves and eviction moratoriums).
The province of Ontario recently announced $12.5 million in funding to support high priority communities, with community outreach, increased testing and wraparound support.82 Leveraging these community tailored interventions specifically for more vulnerable LTC home staff would not only reduce existing inequities that place these individuals and their households at greater risk of COVID-19 infection, but could also reduce LTC home outbreaks.
Further Decrowd Homes by Continuing Limits on Occupancy and Securing Temporary Housing
The evidence from Ontario’s first wave of COVID-19 clearly demonstrated that crowding in LTC homes was significantly associated with an increased incidence of resident SARS-CoV-2 infections and COVID-19 deaths.37 Directives limiting admissions and occupancy to no more than two residents per room are sensible, especially with financial commitments to fund homes as if they were at full capacity. However, these are hard to effectively and rapidly implement in case of existing high levels of occupancy. These directives are set to expire at the end of January 2021. Given the ongoing and extreme demand for LTC in Ontario, and the fact that many residents were already occupying these rooms, there are nearly 3,500 residents currently remaining in multi-occupancy rooms (Figure 22).
While additional funding may be required to financially protect homes when reducing occupancy in the sector, several measures to pre-emptively decrowd Ontario LTC homes may be effective. This includes creating temporary spaces such as field hospitals, using unoccupied hotels, and creating climate-controlled shelters in the parking lots or green spaces of LTC homes.83 These spaces could also be used as part of outbreak management to temporarily relocate residents living in LTC homes with large COVID-19 outbreaks, which could both provide homes with additional space to isolate and cohort residents and reduce some of the burden of caring for complex and high acuity residents in outbreak settings.20,80 The recently opened Specialized Care Centre in the Greater Toronto Area now has the capacity for 30 LTC residents to be temporarily relocated for ongoing care for homes experiencing large outbreaks and staffing challenges.84
Finally, while existing efforts to reduce crowding are necessary to prevent resident SARS-CoV-2 infections and COVID-19 deaths, these efforts resulted in a decreased number of available LTC beds and an increased LTC waiting list, which now stands at over 39,000 Ontarians. Longer-term commitments to build 30,000 new LTC beds in Ontario will not assist with this in the short-term. More home care supports for the increasing number of individuals waiting for LTC placement in the community is essential to avoid increasing the number of alternate level of care (ALC) patients, especially as many hospital are near, at, or above capacity during the second wave. The recent government commitments to make greater investments in the provision of more home and community care and expanded community paramedicine programs to support LTC waitlisted individuals is promising, and other options to consider are innovative proposals like a virtual LTC program.85
Detect LTC Worker Infection and Prevent Importation into LTC Homes by Prioritizing Workers for Testing, and by Guaranteeing Workers Paid Sick Leave
As community transmission of SARS-CoV-2 increases, there is a predictable increase in SARS-CoV-2 infections among LTC staff, necessitating strategies to both prevent and detect community and staff infections before they are imported in to LTC homes.
As previously discussed, many LTC home staff have part-time jobs without access to paid sick leave, meaning that staff may come to work sick and/or they may be forced to work other front-facing jobs that increase their risk of SARS-CoV-2 infection. More immediate and long-term commitments to increasing the number of full-time jobs with fair pay and benefits including paid sick leave will help remedy the staffing crisis and can also help reduce transmission of SARS-CoV-2 into LTC homes.86
It also remains important that LTC residents and staff continue to be prioritized for timely COVID-19 testing with a short turnaround time of results.87 Modeling suggests that frequent serial testing (e.g., 2-3 times weekly) of staff may be effective in reducing outbreaks if test turnaround time is rapid. However, the feasibility of such frequent testing is unclear with Ontario’s current testing system, and this strategy may be insufficiently effective with surging community SARS-CoV-2 transmission.88
Rapid antigen-based COVID-19 testing for staff is being employed in a select number of homes but there are concerns about suboptimal test performance in the high-risk LTC setting, including higher rates of false positives, which could further exacerbate existing staffing shortages. Further, the health human resources a home would require to implement twice or thrice weekly testing is substantial. Finally, staff “bubbling”, where staff confine themselves to a LTC home along with residents, has been implemented with documented success in reducing COVID-19 outbreaks in jurisdictions such as France. However, this approach seems impractical for most Ontario LTC homes.89
Continue Enhancing IPAC by Securing One Specialist per 200 Beds in LTC Homes
IPAC processes have improved in some of Ontario’s LTC homes since the onset of the pandemic, especially with implementation of the “hub and spoke” model where staff are being trained and managed by IPAC specialists of nearby acute care hospitals.90 There is still ongoing and urgent need for increased IPAC staffing, including commitments to hiring infection control staff at a ratio of one specialist per 200 beds in a LTC home, which has been recommended by the Provincial Infectious Diseases Advisory Committee (PIDAC) best practice guidance document since the 2003 SARS-CoV-1 outbreak in Toronto.91
It remains clear that an inadequate understanding of IPAC practice, and an inadequate implementation of IPAC measures in LTC homes relative to acute care hospitals means that outbreaks are controlled rapidly in acute care but are persistent and devastating in LTC settings. While practice improvements have reduced the risk of SARS-CoV-2 transmission in the second wave, as compared to the first wave in Ontario’s LTC sector, the risk of on-going transmission in LTC outbreaks is still substantial. Continued improvement in IPAC practice is key to protecting residents, staff, and essential caregivers from COVID-19.
Pursue a More Balanced and Nuanced Approach to Public Health Measures and Infection Prevention in LTC Homes
The greatest risk factor for whether a home will experience an outbreak is the incidence of SARS-CoV-2 and COVID-19 in the communities surrounding LTC homes. As such, the protection of LTC residents begins with maximal suppression of SARS-CoV-2 transmission in the community. While some have proposed targeted isolation of the vulnerable LTC population, it is practically impossible to restrict outbreaks and transmission in particular subpopulations while allowing widespread transmission of SARS-CoV-2 in the general population.92 Further, targeted isolation of a population is unethical and risks further exacerbating inequities and structural discrimination that are already present in LTC settings.93
Building on the province’s updated visitor guidelines that permitted caregivers back in to LTC homes in September 2020, there is an opportunity to balance and nuance infection prevention and public health measures in Ontario LTC homes. This will keep residents protected from COVID-19 and maintain their health and wellbeing throughout the remainder of the pandemic. Adequate practice and support for practice among essential family caregivers is critical in order to prevent the propagation of outbreaks in LTC homes.
One particularly challenging transition for LTC residents is new admission to a LTC home, since change in a familiar environment can be distressing for residents, especially when nearly 70% live with dementia and almost 90% have some form of cognitive impairment.94 New admissions to Ontario LTC homes currently require 14-days of self-isolation under Droplet and Contact Precautions with a negative SARS-CoV-2 test result at the end of self-isolation.57 This precautionary approach is sensible from an IPAC perspective but can precipitate substantial distress in newly admitted residents who have not yet acclimatized to their new environments. Additional resources and attention should be paid to preventing and mitigating the behavioural and psychological risks of this self-isolation period. This could include implementing strategies in LTC homes that better maintain the dignity and psychological wellbeing of the person requiring self-isolation.95,96
In communities surrounding LTC homes that have been identified as “high risk”, most short-term absences have been suspended, resulting in the inability of most residents to leave the property of a LTC home. While this intervention is likely intended to prevent LTC home residents from entering high-risk transmission settings in the community, it has also had the effect of preventing residents from going outside for fresh air or on short walks in the immediate vicinity of LTC homes; this highlights the need for a more nuanced absence policy, something that has already been implemented in Ontario’s retirement home sector.97
Other areas requiring immediate attention are the avoidance of universal cancellation of congregate dining and social activities in both homes situated in high-risk communities, and in homes where a contained outbreak may be occurring on a separate floor/unit of the home.
Finally, in many areas of the province, residents are no longer allowed to see general visitors, despite the fact that outdoor, distanced, and masked interactions, which were permitted over the summertime in the Province of Ontario, are very low risk interactions for SARS-CoV-2 transmission.
Implementing Strategies to Expedite Administration and Improve Vaccine Acceptance in the LTC Sector
It is reassuring that both the National Advisory Council on Immunization (NACI) and the Ontario’s Ministers’ COVID-19 Vaccine Distribution Task Force prioritized LTC and Retirement home residents, workers, and essential family caregivers for COVID-19 vaccination.98,99 Timely vaccination of Ontario’s LTC home population has the potential to substantially reduce COVID-19 cases and deaths as well as required health care resources.
To facilitate efficient administration of the vaccine, the LTC sector and its clinicians should be supported with educational materials and recommended behavioural change strategies to improve LTC resident, family, staff, and caregiver confidence in the COVID-19 vaccine. LTC homes that are not yet vaccinated should work to secure advanced consent from residents, and where necessary, their substitute decision makers for residents who cannot provide informed consent.
One particularly important initiative will be improving vaccine acceptance among Ontario LTC staff, whose influenza vaccination uptake was 76.4% in 2019-2020.100,101 Strategies to promote vaccine acceptance among LTC homes include: hearing, validating and addressing staff concerns about the COVID-19 vaccine development process, approval and safety; identifying peer champions to educate and encourage fellow staff vaccination; and by providing education and ongoing communication about COVID-19 vaccination programs.102,103 Finances and logistics may pose additional barriers to staff vaccination because of transportation and parking costs, and unpaid time away from work both while going to get vaccinated and in case of vaccine side effects causing missed work.104
Other organizations like the California Association of Long-Term Care Medicine have created a suite of tools to support vaccine implementation in LTC homes, including templated communications for LTC homes, information packages for residents and staff, COVID-19 vaccine consent forms, and information for homes describing strategies to promote vaccine acceptance.105 Similar materials were created and distributed across the Province of Ontario to ensure effective uptake of the COVID-19 vaccine in the LTC sector.
Continue Optimizing Data on LTC Homes for the Duration of the COVID-19 Pandemic
Rapid collection and access to data on the COVID-19 pandemic in Ontario’s LTC homes has generated substantial knowledge that has already been translated into public health policy. It is essential that Ontario continues to optimize sources of data on the LTC sector for the duration of the COVID-19 pandemic and beyond. This includes resuming expedited reviews of all COVID-19 and non-COVID-19 deaths occurring in LTC homes throughout the remainder of the pandemic, which stopped on June 29, 2020. This will facilitate ongoing calculations of excess mortality in the sector. Additionally, timely and complete data on vaccination rates among LTC residents, staff and essentially family caregivers is critical to understanding the success and effectiveness of Ontario’s COVID-19 vaccine rollout.
It is also essential that the LTC sector provide additional resources to LTC homes to promote timely and complete Resident Assessment Instrument – Minimum Data Set 2.0 (RAI-MDS 2.0) data collection on all residents.106,107 This data is essential in understanding how the functional and psychosocial status and care needs of Ontario’s LTC residents have been and continue to be impacted by the COVID-19 pandemic.108 The RAI-MDS 2.0 is normally completed on admission to a LTC home, quarterly, and after any substantial health change. Given the more limited feasibility of completing the RAI-MDS 2.0 during a pandemic, Ontario should prioritize the implementation of the next generation assessment, the interRAI LTCF, which is supported by CIHI and has been implemented in New Brunswick and internationally.109,110
Given the uncertainty some homes have in allowing essential family caregivers and visitors to regularly access homes, and to allow residents to leave on short absences, it is important to collect data on the frequency and nature of these occurrences to both understand the risks they may or may not carry with respect to SARS-CoV-2 transmission and the impact they have on resident quality of life and wellbeing.
Finally, enhancing data on staffing may be effective in increasing the understanding of levels and hours of care being provided to residents in LTC homes as well as the risk of staff being infected with COVID-19 and subsequently importing COVID-19 into LTC homes. This data could help support community tailored approaches specifically focused on LTC home workers.
The COVID-19 pandemic has had a devastating impact on Ontario’s LTC sector. A large body of evidence now documents the predictors of COVID-19 outbreaks, SARS-CoV-2 transmission, and deaths in Ontario’s LTC homes. While some of the existing evidence has been effectively leveraged to support public health interventions and policies, there are additional measures that may be effective in preventing COVID-19 outbreaks and deaths within LTC homes during both the pre- and post-COVID-19 vaccine era.
References
- Canadian Institute for Health Information. Long-term care homes in Canada: How many and who owns them? cihi.ca. Published September 24, 2020. Accessed December 8, 2020. https://www.cihi.ca/en/long-term-care-homes-in-canada-how-many-and-who-owns-them
- Ontario Long-Term Care Association. The role of long-term care. oltca.com. Published 2020. Accessed December 8, 2020. https://www.oltca.com/oltca/OLTCA/Public/LongTermCare/FactsFigures.aspx
- Long-Term Care Staffing Study Advisory Group. Long-Term Care Staffing Study. Ministry of Long-Term Care; 2020:51. https://files.ontario.ca/mltc-long-term-care-staffing-study-en-2020-07-31.pdf
- Block S, Dhunna S. What Does It Cost to Care? Canadian Centre for Policy Alternatives; 2020:12. Accessed December 8, 2020. https://www.policyalternatives.ca/sites/default/files/uploads/publications/Ontario%20Office/2020/06/Improving%20care%20in%20Ontario%20LTC%20facilities_final.pdf
- Ng R, Lane N, Tanuseputro P, et al. Increasing complexity of new nursing home residents in Ontario, Canada: a serial cross-sectional study. J Am Geriatr Soc. 2020;68(6):1293-1300. https://doi.org/10.1111/jgs.16394
- Tanuseputro P, Chalifoux M, Bennett C, et al. Hospitalization and mortality rates in long-term care facilities: does for-profit status matter? J Am Med Dir Assoc. 2015;16(10):874-883. https://doi.org/10.1016/j.jamda.2015.06.004
- Canadian Institute for Health Information. Pandemic Experience in the Long-Term Care Sector: How Does Canada Compare with Other Countries? Canadian Institute for Health Information; 2020. https://www.cihi.ca/sites/default/files/document/covid-19-rapid-response-long-term-care-snapshot-en.pdf
- Sepulveda ER, Stall NM, Sinha SK. A comparison of COVID-19 mortality rates among long-term care residents in 12 OECD countries. J Am Med Dir Assoc. 2020;21(11):1572-1574.e3. https://doi.org/10.1016/j.jamda.2020.08.039
- Comas-Herrera A, Zalakaín J, Litwin C, et al. Mortality Associated with COVID-19 Outbreaks in Care Homes: Early International Evidence. International Long-Term Care Policy Network; 2020:28. Accessed December 8, 2020. https://ltccovid.org/wp-content/uploads/2020/06/Mortality-associated-with-COVID-among-people-who-use-long-term-care-26-June-1.pdf
- Postill G, Murray R, Wilton AS, et al. An analysis of mortality in Ontario using cremation data: rise in cremations during the COVID-19 pandemic. MedRxiv. Published online July 24, 2020. https://doi.org/10.1101/2020.07.22.20159913
- Government of Ontario. Long-term care home COVID-19 data. Data Catalogue. Published January 18, 2021. Accessed January 19, 2021. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
- Public Health Ontario. Enhanced Epidemiological Summary: Trends of COVID-19 Incidence in Ontario. Ontario Agency for Health Protection and Promotion; 2020:18. https://www.publichealthontario.ca/-/media/documents/ncov/epi/covid-19-epi-trends-incidence-ontario.pdf?la=en
- Government of Canada. Population estimates on July 1st, by age and sex. Statistics Canada. Published September 29, 2020. Accessed January 17, 2021. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501
- Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382(22):2081-2090. https://doi.org/10.1056/NEJMoa2008457
- Goldberg SA, Lennerz J, Klompas M, et al. Presymptomatic transmission of Severe Acute Respiratory Syndrome Coronavirus 2 among residents and staff at a skilled nursing facility: results of real-time Polymerase Chain Reaction and serologic testing. Clinical Infectious Diseases. 2020;(ciaa991). https://doi.org/10.1093/cid/ciaa991
- Hoxha A, Wyndham-Thomas C, Klamer S, et al. Asymptomatic SARS-CoV-2 infection in Belgian long-term care facilities. The Lancet Infectious Diseases. Published online July 2020:S1473309920305600. https://doi.org/10.1016/S1473-3099(20)30560-0
- Dunning J, Dhuper M, Sinha S. The NIA’s ‘Iron Ring’ Guidance for Protecting Older Canadians in Long-Term Care and Congregate Living Settings. National Institute on Ageing https://static1.squarespace.com/static/5c2fa7b03917eed9b5a436d8/t/5f0f4610bcc2c332db002e67/1594836496177/NIA+Iron+Ring+Guidance+Document+July+15_2020.pdf
- Jüni P, Odutayo A, Allen U, et al. Dexamethasone in Patients Hospitalized for COVID-19. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2020;1(1). https://doi.org/10.47326/ocsat.2020.01.01.1.0
- Government of Canada. Interim guidance: Care of residents in long term care homes during the COVID-19 pandemic. Published July 17, 2020. Accessed December 20, 2020. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/residents-long-term-care-homes-covid-19.html
- Stall NM, Farquharson C, Fan‐Lun C, et al. A hospital partnership with a nursing home experiencing a COVID-19 outbreak: description of a multiphase emergency response in Toronto, Canada. JAGS. 2020;68(7):1376-1381. https://doi.org/10.1111/jgs.16625
- Marrocco FN, Coke A, Kitts J. Ontario’s long-term care COVID-19 commission. First interim recommendations. Published online October 23, 2020. Accessed December 5, 2020. http://www.ltccommission-commissionsld.ca/ir/pdf/20201023_First_Interim_Letter_English.pdf
- Ontario takes immediate steps to further protect long-term care residents and staff during COVID-19 outbreak. Ontario.ca. Published April 22, 2020. Accessed May 2, 2020. https://news.ontario.ca/en/release/56737/ontario-takes-immediate-steps-to-further-protect-long-term-care-residents-and-staff-during-covid-19
- Brown KA, Daneman N, Buchan SA, Chan AK, Stall NM. Temporal variations in the intensity of care provided to community and nursing home residents who died of COVID-19 in Ontario, Canada. medRxiv. Published online November 10, 2020:2020.11.06.20227140. https://doi.org/10.1101/2020.11.06.20227140
- Stall NM, Wu W, Lapointe‐Shaw L, et al. Sex- and age-specific differences in COVID-19 testing, cases, and outcomes: a population-wide study in Ontario, Canada. AGS. 2020;68(10):2188-2191. https://doi.org/10.1111/jgs.16761
- Rochon PA, Wu W, Giannakeas V, Stall NM. The missing pieces of the COVID‐19 puzzle. J Am Geriatr Soc. Published online June 23, 2020. https://doi.org/10.1111/jgs.16646
- Stall NM, Fischer HD, Fung K, et al. Sex-specific differences in end-of-life burdensome interventions and antibiotic therapy in nursing home residents with advanced dementia. JAMA Netw Open. 2019;2(8):e199557. https://doi.org/10.1001/jamanetworkopen.2019.9557
- White EM, Kosar CM, Feifer RA, et al. Variation in SARS-CoV-2 prevalence in U.S. skilled nursing facilities. J Am Geriatr Soc. 2020;68(10):2167-2173. https://doi.org/10.1111/jgs.16752
- Ouslander JG, Grabowski DC. COVID-19 in nursing homes: calming the perfect storm. AGS. 2020;68(10):2153-2162. https://doi.org/10.1111/jgs.16784
- Malikov K, Huang Q, Shi S, Stall NM, Tuite AR, Hillmer MP. Temporal associations between community incidence of COVID-19 and nursing home outbreaks in Ontario, Canada. medRxiv. Published online November 19, 2020:2020.11.17.20233312. https://doi.org/10.1101/2020.11.17.20233312
- COVID-19 response framework: keeping Ontario safe and open. Ontario.ca. Published December 4, 2020. Accessed December 6, 2020. https://www.ontario.ca/page/covid-19-response-framework-keeping-ontario-safe-and-open
- COVID-19: long-term care homes in areas with visitor restrictions. Ontario.ca. Published November 20, 2020. Accessed December 6, 2020. https://www.ontario.ca/page/covid-19-long-term-care-homes-in-areas-visitor-restrictions
- Ministry of Finance. Ontario Population Projections, 2019–2046. Government of Ontario; 2020. https://www.fin.gov.on.ca/en/economy/demographics/projections/
- Chow EJ, Schwartz NG, Tobolowsky FA, et al. Symptom screening at Illness onset of health care personnel with SARS-CoV-2 infection in King County, Washington. JAMA. 2020;323(20):2087. https://doi.org/10.1001/jama.2020.6637
- Vijh R, Ghafari C, Hayden A, et al. Serological survey following SARS-COV-2 outbreaks at long-term care facilities in metro Vancouver, British Columbia: Implications for outbreak management and infection control policies. AJIC. 2020;0(0). https://doi.org/10.1016/j.ajic.2020.10.009
- Fisman DN, Bogoch I, Lapointe-Shaw L, McCready J, Tuite AR. Risk factors associated with mortality among residents with coronavirus disease 2019 (COVID-19) in long-term care facilities in Ontario, Canada. JAMA Netw Open. 2020;3(7):e2015957. https://doi.org/10.1001/jamanetworkopen.2020.15957
- Stall NM, Jones A, Brown KA, Rochon PA, Costa AP. For-profit long-term care homes and the risk of COVID-19 outbreaks and resident deaths. CMAJ. 2020;192(33):E946-E955. https://doi.org/10.1503/cmaj.201197
- Brown KA, Jones A, Daneman N, et al. Association between nursing home crowding and COVID-19 infection and mortality in Ontario, Canada. JAMA Intern Med. Published online November 9, 2020. https://doi.org/10.1001/jamainternmed.2020.6466
- Hado E, Feinberg LF. Amid the COVID-19 pandemic, meaningful communication between family caregivers and residents of long-term care facilities is imperative. Journal of Aging & Social Policy. 2020;32(4-5):410-415. https://doi.org/10.1080/08959420.2020.1765684
- Committee on Family Caregiving for Older Adults, Board on Health Care Services, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine. Families Caring for an Aging America. (Schulz R, Eden J, eds.). National Academies Press (US); 2016. http://www.ncbi.nlm.nih.gov/books/NBK396401/
- Schlaudecker JD. Essential family caregivers in long-term care during the COVID-19 pandemic. J Am Med Dir Assoc. 2020;21(7):983. https://doi.org/10.1016/j.jamda.2020.05.027
- Suarez-Gonzalez A. Detrimental Effects of Confinement and Isolation on the Cognitive and Psychological Health of People Living with Dementia during COVID-19: Emerging Evidence. International Long Term Care Policy Network; 2020.
- Low L-F. Easing lockdowns in care homes during COVID-19: risks and risk reduction. ltccovid.org. Published May 13, 2020. Accessed July 7, 2020. https://ltccovid.org/2020/05/13/easing-lockdowns-in-care-homes-during-covid-19-risks-and-risk-reduction/
- Abbasi J. Social isolation—the other COVID-19 threat in nursing homes. JAMA. 2020;324(7):619. https://doi.org/10.1001/jama.2020.13484
- Cagnin A, Di Lorenzo R, Marra C, et al. Behavioral and psychological effects of coronavirus disease-19 quarantine in patients with dementia. Front Psychiatry. 2020;11. https://doi.org/10.3389/fpsyt.2020.578015
- Van der Roest HG, Prins M, van der Velden C, et al. The Impact of COVID-19 Measures on Well-Being of Older Long-Term Care Facility Residents in the Netherlands. J Am Med Dir Assoc. 2020;21(11):1569-1570. https://doi.org/10.1016/j.jamda.2020.09.007
- Diamantis S, Noel C, Tarteret P, Vignier N, Gallien S. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)-related deaths in french long-term care facilities: the “Confinement Disease” is probably more deleterious than the coronavirus disease-2019 (COVID-19) itself. Journal of the American Medical Directors Association. 2020;21(7):989-990. https://doi.org/10.1016/j.jamda.2020.04.023
- Confinement Syndrome. North Simcoe Muskoka Specialized Geriatric Services; 2020. Accessed December 7, 2020. https://www.nsmsgs.ca/Uploads/ContentDocuments/Confinement%20Syndrome%20Aug17-20.pdf
- Rochon PA. Variation in nursing home antipsychotic prescribing rates. Arch Intern Med. 2007;167(7):676. https://doi.org/10.1001/archinte.167.7.676
- Howard R, Burns A, Schneider L. Antipsychotic prescribing to people with dementia during COVID-19. The Lancet Neurology. 2020;19(11):892. https://doi.org/10.1016/S1474-4422(20)30370-7
- Stall NM, Zipursky JS, Rangrej J, et al. Increased prescribing of psychotropic medications to ontario nursing home residents during the COVID-19 pandemic. medRxiv. Published online November 30, 2020:2020.11.26.20239525. https://doi.org/10.1101/2020.11.26.20239525
- McMichael TM, Currie DW, Clark S, et al. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382(21):2005-2011. https://doi.org/10.1056/NEJMoa2005412
- Chen MK, Chevalier JA, Long EF. Nursing home staff networks and COVID-19. NBER. Published online October 2020:28. https://doi.org/10.3386/w27608
- Liu M, Maxwell CJ, Armstrong P, et al. COVID-19 in long-term care homes in Ontario and British Columbia. CMAJ. 2020;192(47):E1540-E1546. https://doi.org/10.1503/cmaj.201860
- Government of Ontario. O. reg. 146/20: limiting work to a single long-term care home. Ontario.ca. Published July 24, 2014. Accessed December 7, 2020. https://www.ontario.ca/laws/view
- Jones A, Watts AG, Khan SU, et al. Impact of a public policy restricting staff mobility between long-term care homes in Ontario, Canada during the COVID-19 pandemic. medRxiv. Published online November 18, 2020:2020.11.17.20231498. https://doi.org/10.1101/2020.11.17.20231498
- Ministry of Health and Long-Term Care. Capacity planning and analytics division. Presented at the: September 2020; Ontario. Accessed December 24, 2020. http://www.ltccommission-commissionsld.ca/presentations/pdf/LTCC_Capacity_Planning_and_Analytics_Overview.pdf
- Directive #3 update: long-term care visitors and admissions. Published online 2020. Accessed December 7, 2020. http://health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/directives/LTCH_HPPA.pdf
- Chu CH, Donato‐Woodger S, Dainton CJ. Competing crises: COVID-19 countermeasures and social isolation among older adults in long-term care. Journal of Advanced Nursing. 2020;76(10):2456-2459. https://doi.org/10.1111/jan.14467
- Stall NM, Johnstone J, McGeer AJ, Dhuper M, Dunning J, Sinha SK. Finding the right balance: an evidence-informed guidance document to support the re-opening of canadian nursing homes to family caregivers and visitors during the coronavirus disease 2019 pandemic. JAMDA. 2020;21(10):1365-1370.e7. https://doi.org/10.1016/j.jamda.2020.07.038
- Long-Term Care Interest Group. Family presence in older adult care a statement regarding family caregivers and the provision of essential care. Published online June 29, 2020. https://rgps.on.ca/wp-content/uploads/2020/06/2020-June-29-Family-Presence-in-Older-Adult-Care-Family-Caregivers-FINAL.pdf
- Reuniting family with their loved ones in long-term care homes during COVID-19. Published online July 15, 2020. Accessed December 7, 2020. https://rnao.ca/sites/rnao-ca/files/FINAL_RNAO_Statement_on_Reuniting_Families_in_LTC_1.pdf
- Canadian Foundation for Healthcare Improvement. Better together: e-integration of family caregivers as essential partners in care in a time of COVID-19. Published online July 2020. Accessed July 8, 2020. https://www.cfhi-fcass.ca/docs/default-source/itr/tools-and-resources/bt-re-integration-of-family-caregivers-as-essential-partners-covid-19-e.pdf?sfvrsn=5b3d8f3d_2
- Government of Ontario. Welcoming caregivers to Ontario’s long-term care homes. Ontario Newsroom. Published September 2, 2020. Accessed January 18, 2021. https://news.ontario.ca/en/release/58220/welcoming-caregivers-to-ontarios-long-term-care-homes
- Tupper SM, Ward H, Parmar J. Family Presence in Long-Term Care During the COVID-19 Pandemic: Call to Action for Policy, Practice, and Research. Can Geriatr J. 2020;23(4):335-339. https://doi.org/10.5770/cgj.23.476
- Ministry of Long Term Care. Resuming Visits in Long-Term Care Homes. Government of Ontario; 2020:12. Accessed December 7, 2020. http://health.gov.on.ca/en/pro/programs/ltc/docs/covid-19/mltc_visitor_policy_20200909_en.pdf
- Comas-Herrera A, Salcher-Konrad M, Baumbusch J, Farina N, Goodman C, Lorenz-Dant K. Rapid Review of the Evidence on Impacts of Visiting Policies in Care Homes during the COVID-19 Pandemic. McMaster University; 2020:6. Accessed December 8, 2020. https://www.nccmt.ca/uploads/media/media/0001/02/3021cb8ca67e86dfa1d29ea5ef2ea14dc486bfe1.pdf
- Kruse F, Vrinzen C, Jeurissen P, van der Woerd O, van Tol L. The impact of COVID-19 on long-term care in the Netherlands: the second wave. Published online November 25, 2020:24. https://ltccovid.org/2020/11/25/updated-country-report-the-impact-of-covid-19-on-long-term-care-in-the-netherlands-the-second-wave/
- The National Collaborating Centre for Methods and Tools. Rapid Review: What Risk Factors Are Associated with COVID-19 Outbreaks and Mortality in Long-Term Care Facilities and What Strategies Mitigate Risk? McMaster University; 2020. Accessed January 18, 2021. https://www.nccmt.ca/uploads/media/media/0001/02/3021cb8ca67e86dfa1d29ea5ef2ea14dc486bfe1.pdf
- Verbeek H, Gerritsen DL, Backhaus R, de Boer BS, Koopmans RTCM, Hamers JPH. Allowing visitors back in the nursing home during the COVID-19 crisis: a dutch national study into first experiences and impact on well-being. J Am Med Dir Assoc. 2020;21(7):900-904. https://doi.org/10.1016/j.jamda.2020.06.020
- Duan Y, Iaconi A, Song Y, et al. Care Aides Working Multiple Jobs: Considerations for Staffing Policies in Long-Term Care Homes During and After the COVID-19 Pandemic. J Am Med Dir Assoc. 2020;21(10):1390-1391. https://doi.org/10.1016/j.jamda.2020.07.036
- Houtven CHV, DePasquale N, Coe NB. Essential long-term care workers commonly hold second jobs and double- or triple-duty caregiving roles. J Am Geriatr Soc. 2020;68(8):1657-1660. https://doi.org/10.1111/jgs.16509
- Boscart VM, Sidani S, Poss J, et al. The associations between staffing hours and quality of care indicators in long-term care. BMC Health Serv Res. 2018;18(1):750. https://doi.org/10.1186/s12913-018-3552-5
- Harrington C, Ross L, Chapman S, Halifax E, Spurlock B, Bakerjian D. Nurse staffing and coronavirus infections in California nursing homes. Policy, Politics, & Nursing Practice. 2020;21(3):174-186. https://doi.org/10.1177/1527154420938707
- Gorges RJ, Konetzka RT. Staffing levels and COVID-19 cases and outbreaks in U.S. nursing homes. J Am Geriatr Soc. 2020;68(11):2462-2466. https://doi.org/10.1111/jgs.16787
- Royal Society of Canada. Restoring Trust: COVID-19 and the Future of Long-Term Care.; 2020. Accessed December 6, 2020. https://rsc-src.ca/sites/default/files/LTC%20PB%20%2B%20ES_EN_0.pdf
- Government of Ontario. A better place to live, a better place to work: Ontario’s long-term care staffing plan. Ontario.ca. Published December 16, 2020. Accessed December 20, 2020. https://www.ontario.ca/page/better-place-live-better-place-work-ontarios-long-term-care-staffing-plan
- Armstrong P, Cohen M. A Higher Standard: Setting Federal Standards in Long-Term Care and Continuing Care. Canadian Cantre for Policy Alternatives; 2020. Accessed January 18, 2021. https://www.policyalternatives.ca/sites/default/files/uploads/publications/National%20Office/2020/11/A%20higher%20standard.pdf
- Sundaram ME, Calzavara A, Mishra S, et al. The individual and social determinants of COVID-19 in Ontario, Canada: a population-wide study. medRxiv. Published online November 12, 2020:2020.11.09.20223792. https://doi.org/10.1101/2020.11.09.20223792
- Shen K. Relationship between nursing home COVID-19 outbreaks and staff neighborhood characteristics. medRxiv. Published online September 11, 2020:2020.09.10.20192203. https://doi.org/10.1101/2020.09.10.20192203
- Alliance for Healthier Communities. To effectively support marginalized people most impacted by COVID-19, Ontario needs a community response strategy. Published November 17, 2020. Accessed January 18, 2021. https://www.allianceon.org/blog/effectively-support-marginalized-people-most-impacted-COVID-19-Ontario-needs-community-response
- Public Health Agency of Canada. From Risk to Resilience: An Equity Approach to COVID-19.; 2020. Accessed January 18, 2021. https://www.canada.ca/content/dam/phac-aspc/documents/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19/cpho-covid-report-eng.pdf
- Government of Ontario. Ontario supporting high priority communities. Ontario Newsroom. Published December 21, 2020. Accessed January 17, 2021. https://news.ontario.ca/en/backgrounder/59793/ontario-supporting-high-priority-communities
- Baughman AW, Hirschberg RE, Lucas LJ, et al. Pandemic care through collaboration: lessons from a COVID-19 field hospital. JAMDA. 2020;21(11):1563-1567. https://doi.org/10.1016/j.jamda.2020.09.003
- Government of Ontario. Ontario opening specialized care centre in Greater Toronto Area. Ontario Newsroom. Published December 28, 2020. Accessed January 17, 2021. https://news.ontario.ca/en/release/59829/ontario-opening-specialized-care-centre-in-greater-toronto-area
- National Institute for Ageing. Bringing Long-Term Care Home.; 2020. Accessed December 7, 2020. https://static1.squarespace.com/static/5c2fa7b03917eed9b5a436d8/t/5fb57afdbb4dec698ea3b7d2/1605729021992/BringLTCHome_V2.11.17%284%29pdf.pdf
- Rios P, Radhakrishnan A, Williams C, et al. Preventing the transmission of COVID-19 and other coronaviruses in older adults aged 60 years and above living in long-term care: a rapid review. Systematic Reviews. 2020;9(1):218. https://doi.org/10.1186/s13643-020-01486-4
- McGarry BE, SteelFisher GK, Grabowski DC, Barnett ML. COVID-19 test result turnaround time for residents and staff in US nursing homes. JAMA Intern Med. Published online October 30, 2020. https://doi.org/10.1001/jamainternmed.2020.7330
- Chin ET, Huynh BQ, Chapman LA, Murrill M, Basu S, Lo NC. Frequency of routine testing for COVID-19 in high-risk environments to reduce workplace outbreaks. medRxiv. Published online September 9, 2020:2020.04.30.20087015. https://doi.org/10.1101/2020.04.30.20087015
- Belmin J, Um-Din N, Donadio C, et al. Coronavirus disease 2019 outcomes in french nursing homes that implemented staff confinement with residents. JAMA Netw Open. 2020;3(8):e2017533. https://doi.org/10.1001/jamanetworkopen.2020.17533
- Elrod JK, Fortenberry JL. The hub-and-spoke organization design: an avenue for serving patients well. BMC Health Serv Res. 2017;17(1):457. https://doi.org/10.1186/s12913-017-2341-x
- Ontario Agency for Health Protection and Promotion, Provincial Infectious Diseases Advisory Committee, Ontario, Public Health Ontario. Best Practices for Infection Prevention and Control Programs in Ontario: In All Health Care Settings. Public Health Ontario; 2012. Accessed January 18, 2021. https://www.deslibris.ca/ID/236594
- Alwan NA, Burgess RA, Ashworth S, et al. Scientific consensus on the COVID-19 pandemic: we need to act now. The Lancet. 2020;396(10260):e71-e72. https://doi.org/10.1016/S0140-6736(20)32153-X
- Ganguli-Mitra A, Young I, Engelmann L, et al. Segmenting communities as public health strategy: a view from the social sciences and humanities. Wellcome Open Res. 2020;5:104. https://doi.org/10.12688/wellcomeopenres.15975.1
- Canadian Institute for Health Information. Dementia in long-term care. Journal of Nursing Management. Published 2020. Accessed December 26, 2020. https://www.cihi.ca/en/dementia-in-canada/dementia-care-across-the-health-system/dementia-in-long-term-carehttps://www.cihi.ca/en/dementia-in-canada/dementia-care-across-the-health-system/dementia-in-long-term-care
- Iaboni A, Grigorovich A, Barned C, et al. Dementia Isolation Toolkit.; 2020:38. Accessed December 8, 2020. https://dementiaisolationtoolkit.com/wp-content/uploads/2020/09/Dementia-Isolation-Toolkit-Full-1.pdf
- Iaboni A, Cockburn A, Marcil M, et al. Achieving safe, effective, and compassionate quarantine or isolation of older adults with dementia in nursing homes. Am J Geriatr Psychiatry. 2020;28(8):835-838. https://doi.org/10.1016/j.jagp.2020.04.025
- Government of Ontario. Retirement Home COVID-19 Visiting Policy.; 2020:17.
- Ismail SJ, Zhao L, Tunis MC, Deeks SL, Quach C. Key populations for early COVID-19 immunization: preliminary guidance for policy. CMAJ. 2020;192(48):E1620-E1632. https://doi.org/10.1503/cmaj.202353
- Government of Ontario. Ontario identifies key groups for distribution of initial COVID-19 vaccines. Ontario Newsroom. Published December 7, 2020. Accessed December 7, 2020. https://news.ontario.ca/en/release/59508/ontario-identifies-key-groups-for-distribution-of-initial-covid-19-vaccines
- Public Health Ontario. Median Influenza Immunization Coverage Rates: Ontario Hospital and Long-Term Care Staff, 2019-20 Influenza Season. Ontario Agency for Health Protection and Promotion; 2020:2. Accessed December 8, 2020. https://www.publichealthontario.ca/-/media/documents/f/2020/factsheet-influenza-immunization-rates-hcw-2019-20.pdf?la=en
- Jaklevic MC. Nursing homes’ next test—vaccinating workers against COVID-19. JAMA. 2020;324(19):1928. https://doi.org/10.1001/jama.2020.21354
- Finney Rutten LJ, Zhu X, Leppin A, et al. Evidence-based strategies for clinical organizations to address COVID-19 vaccine hesitancy. Mayo Clin Proc. Published online December 28, 2020:S0025619620314877. https://doi.org/10.1016/j.mayocp.2020.12.024
- French J, Deshpande S, Evans W, Obregon R. Key guidelines in developing a pre-emptive COVID-19 vaccination uptake promotion strategy. Int J Environ Res Public Health. 2020;17(16). https://doi.org/10.3390/ijerph17165893
- Volpp KG, Loewenstein G, Buttenheim AM. Behaviorally informed strategies for a national COVID-19 vaccine promotion program. JAMA. 2021;325(2):125-126. https://doi.org/10.1001/jama.2020.24036
- California Association of Long Term Care Medicine. COVID-19 guidance and resources. caltcm.org. Published 2020. Accessed December 6, 2020. https://www.caltcm.org/covid-19
- Kim H, Jung Y-I, Sung M, Lee J-Y, Yoon J-Y, Yoon J-L. Reliability of the interRAI Long Term Care Facilities (LTCF) and interRAI Home Care (HC). Geriatr Gerontol Int. 2015;15(2):220-228. https://doi.org/10.1111/ggi.12330
- Mor V. A comprehensive clinical assessment tool to inform policy and practice: applications of the minimum data set. Med Care. 2004;42(4):III. https://doi.org/10.1097/01.mlr.0000120104.01232.5e
- McArthur C, Saari M, Heckman GA, et al. Evaluating the effect of COVID-19 pandemic lockdown on long-term care residents’ mental health: a data-driven approach in New Brunswick. J Am Med Dir Assoc. 2021;22(1):187-192. https://doi.org/10.1016/j.jamda.2020.10.028
- Hirdes JP, Ljunggren G, Morris JN, et al. Reliability of the interRAI suite of assessment instruments: a 12-country study of an integrated health information system. BMC Health Serv Res. 2008;8(1):277. https://doi.org/10.1186/1472-6963-8-277
- interRAI. Long-term care facilities (LTCF). interrai.org. Published 2020. Accessed December 20, 2020. https://www.interrai.org/long-term-care-facilities.html
Slide Deck & Video Presentation
Document Information & Citation
Author Contributions: NS wrote the first draft of the science brief. All authors contributed to the conception of the science brief, revised it critically for important intellectual content, and approved the final version.
Citation: Stall NM, Brown KA, Maltsev A, et al. COVID-19 and Ontario’s long-term care homes. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;2(7). https://doi.org/10.47326/ocsat.2021.02.07.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Copyright: 2020 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table and its partners.
This Science Brief was updated with minor changes on January 26, 2021.
