Key Message
SARS-CoV-2 infection has taken a disproportionate toll on Ontario older adults, and on residents of disadvantaged and racialized urban neighbourhoods throughout the province.
Prioritizing and implementing vaccine distribution for Ontarians based on both age and neighbourhood of residence could ensure that those at the highest risk of SARS-CoV-2 infection, and hospitalization, ICU admission or death from COVID-19 will be among the first to receive vaccines.
This vaccine strategy will maximize the prevention of deaths and long-term morbidity, and best maintain health care system capacity by reducing hospitalizations and ICU admissions due to COVID-19 as compared with a strategy that prioritizes vaccination based on age alone (Figure 1).
The strategy would not interfere with the ongoing and future vaccination of any specific high-risk population, as it is intended to guide the mass distribution of vaccines to the general Ontario population.
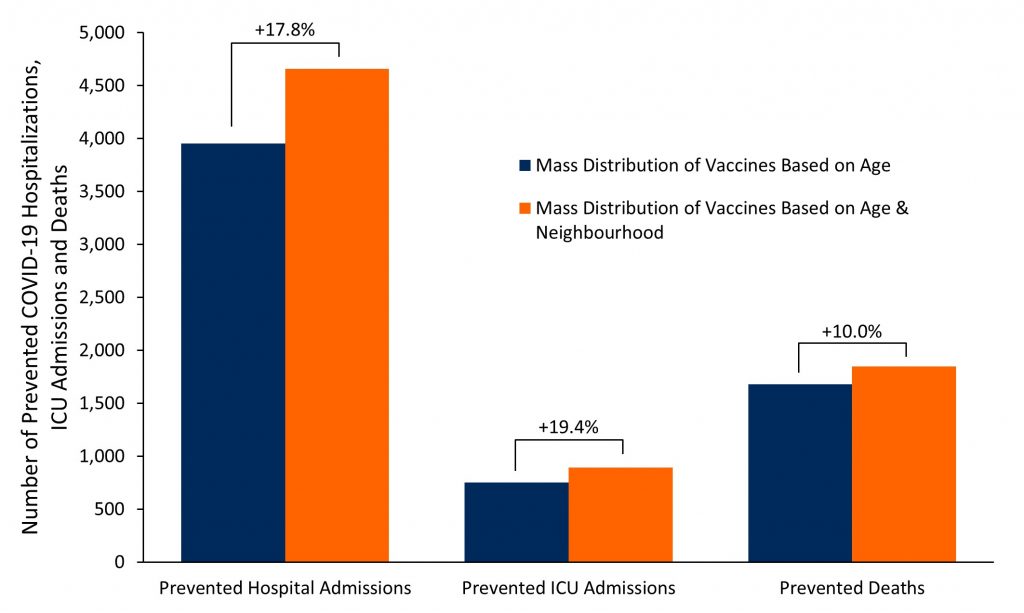
Bar graph presenting the projected number of prevented hospitalizations, ICU admissions and deaths due to COVID-19 in Ontario from March 1-May 31, 2021 under two strategies for mass distribution of vaccines: 1) prioritization based on age alone (blue bars) and 2) prioritization based on age and neighbourhood of residence (orange bars). The brackets above the bar graphs report the relative difference (%) in prevented outcomes between the two strategies for mass distribution of vaccines. See Table 1 below for the number of projected events associated with the different distribution strategies.
Summary
Background
Ontario is currently in the initial stages of its COVID-19 vaccine distribution plan, which involves the vaccination of 1.5-million high-risk individuals. Rapidly immunizing those at the greatest risk of acquiring SARS-CoV-2 infection and experiencing hospitalization, ICU admission and death from COVID-19 outside of specific high-risk groups will continue to be important in the Ontario’s subsequent mass distribution stages of vaccine, especially in the face of limited vaccine supply and with the emergence of variants of concern.
Questions
Which Ontario age groups and neighbourhoods have experienced the highest incidence of SARS-CoV-2 infection and hospitalizations, ICU admissions and deaths due to COVID-19?
What is the potential impact of an Ontario mass distribution strategy for COVID-19 vaccines that explicitly takes both age and neighbourhood of residence into account?
Findings
COVID-19 deaths and hospitalizations are strongly associated with individuals’ age and neighbourhood of residence. As of January 16, 2021, 50% of Ontario COVID-19 deaths, outside of LTC and retirement homes, have occurred in just 4% of the population aged 16 years or above. Similarly, 50% of hospitalizations were concentrated in just 11% of the population aged 16 years or above. The highest risk populations can be reliably identified using information on individuals’ age and neighbourhood of residence.
Projections indicate that a vaccine strategy prioritizing both age and neighbourhood would prevent an additional 3,767 cases of SARS-CoV-2 infection, and 702 hospital admissions, 145 ICU admissions, and 168 deaths from COVID-19 as compared to a strategy that prioritizes based on age alone.
Interpretation
A mass vaccine distribution strategy that prioritizes individuals based on both their age and neighbourhood of residence can reduce cases of SARS-CoV-2 infection, and hospitalizations, ICU admissions, and deaths due to COVID-19, and will also directly address the inequitable impact of COVID-19 on disadvantaged populations in Ontario.
The number of events prevented by this strategy will further increase in the context of vaccine scarcity, with increasing duration of the vaccine rollout, if the daily incidence of SARS-CoV-2 cases increases, if vaccination not only protects against symptomatic COVID-19, but also against asymptomatic infection and transmission, and if an age-based strategy is inequitable, resulting in higher vaccination rates in wealthier neighbourhoods, as currently observed in the United States.
Full Text
Background
COVID-19 has taken a disproportionate toll on older adults and residents of disadvantaged urban neighbourhoods in Ontario. More than 95% of Ontario’s COVID-19 deaths have occurred among individuals aged 60 years and older, and the COVID-19 case fatality rate is more than 100 times higher in individuals aged 80 years and older, as compared to individuals under 40 years of age.1 The incidence of SARS-CoV-2 infection is also disproportionately higher in urban neighbourhoods, especially in those with higher concentrations of essential workers, crowded housing, multigenerational family households, visible minorities and individuals with lower socioeconomic status.2 Recent evidence from the United States suggests that the mass distribution of the COVID-19 vaccine—which has largely used an age-based prioritization framework—has been inequitable, with higher vaccination rates in wealthier neighbourhoods, which also have lower incidences of SARS-CoV-2 infections and COVID-19 deaths.3,4 This has led to calls to consider prioritizing vaccine distribution based on both age and residence in neighbourhoods most severely affected by COVID-19.5,6
Ontario is currently in the initial stages of its COVID-19 vaccine distribution plan, which involves the vaccination of 1.5-million high-risk individuals, including residents, staff and caregivers of residents in congregate care settings; frontline healthcare workers; adults in First Nations, Métis, and Inuit populations; adult chronic home care recipients; and people aged 80 years or older. Rapidly immunizing those at the greatest risk of acquiring SARS-CoV-2 infection and experiencing hospitalization, ICU admission and death from COVID-19 outside of specific high-risk groups will continue to be important in the subsequent mass distribution stages, especially in the face of limited vaccine supply and the emergence of variants of concern.7 This approach will minimize deaths and long-term morbidity, and maintain health care system capacity.
Questions
Which Ontario age groups and neighbourhoods have experienced the highest incidence of SARS-CoV-2 infection and hospitalizations, ICU admissions and deaths due to COVID-19?
What is the potential impact of a mass distribution strategy for COVID-19 vaccines that explicitly takes both age and neighbourhood of residence into account?
Findings
Retrospective Analysis
To date, Ontario neighbourhoods with the highest cumulative incidence of SARS-CoV-2 infections are in Toronto, Peel, York, and Windsor-Essex regions (Figures 2 and 3).
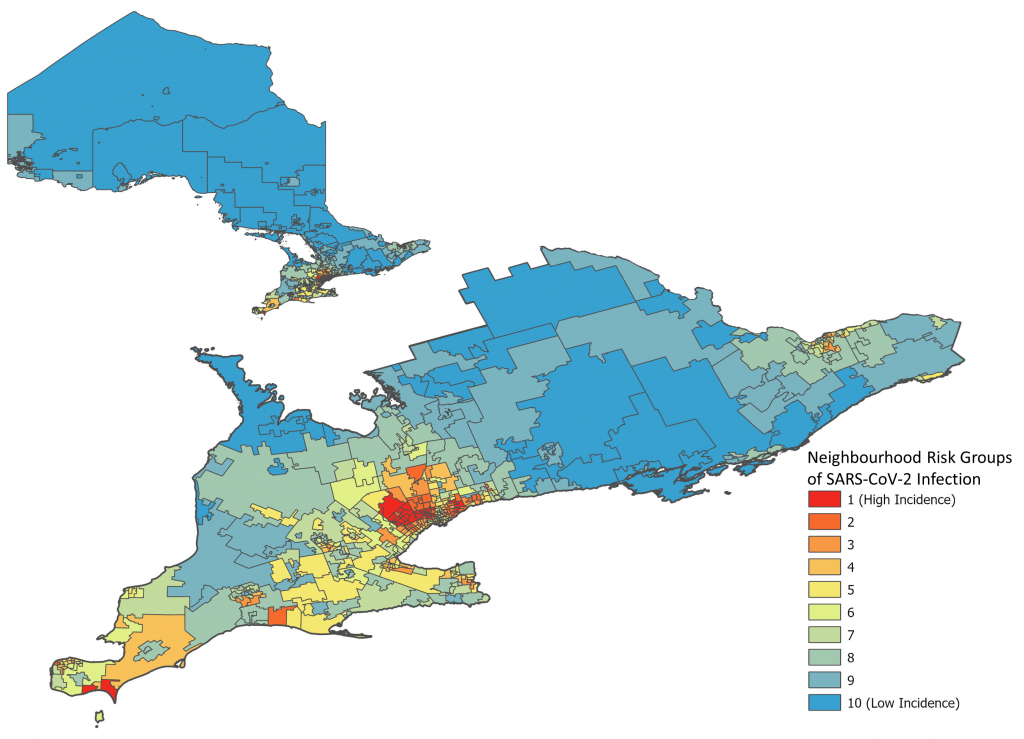
Neighbourhoods ranked in 10% increments by cumulative incidence of SARS-CoV-2 infection between Jan 23, 2020 and Jan 16, 2021. Each group represents 10% of the Ontario population (~1.5 million inhabitants). Neighbourhoods are defined by the first three digits of a resident’s postal code (also known as “forward sortation area”). A total of 509 neighbourhoods were analyzed. Group 1 includes neighbourhoods with the highest cumulative incidence of SARS-CoV-2 infection, whereas group 10 includes neighbourhoods with the lowest cumulative incidence of SARS-CoV-2 infection. Data sourced from the Public Health Case and Contact Management Solution and other case management systems (CCM plus), extracted on January 16, 2021.
As of January 16, 2021, 1,758 Ontarians have died of COVID-19 outside of long-term care (LTC) and retirement homes. Of these deaths, 21% occurred in Ontario neighbourhoods ranked in the top 10% of SARS-CoV-2 infection rates, while 49% of deaths occurred in individuals aged 80 years and older.
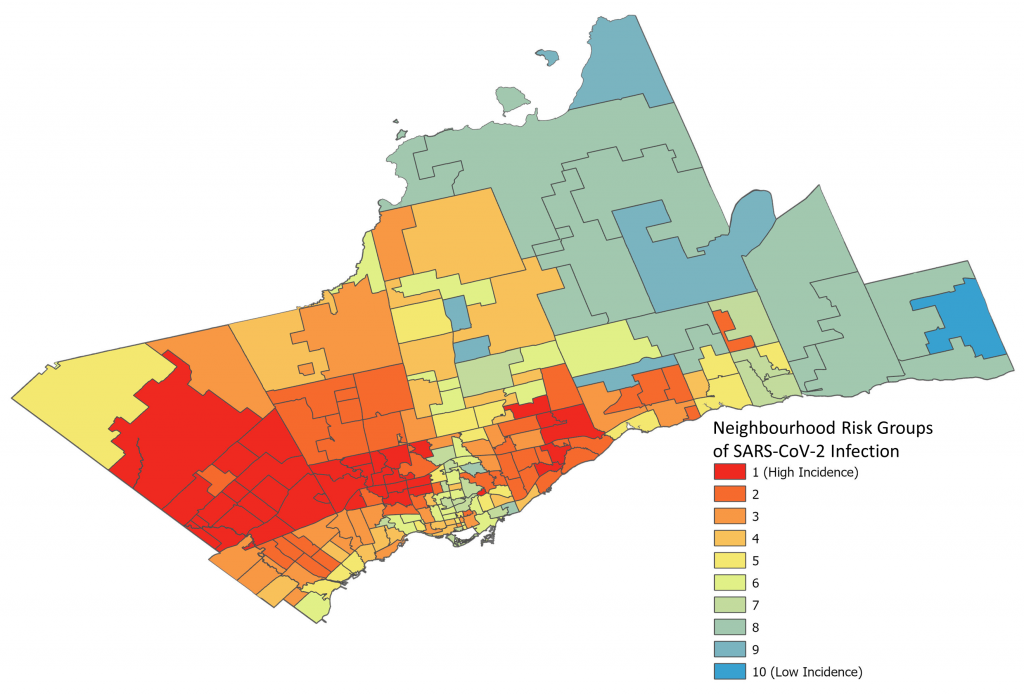
Neighbourhoods ranked in 10% increments by cumulative incidence of SARS-CoV-2 infection between Jan 23, 2020 and Jan 16, 2021. Neighbourhoods are defined by the first three digits of a resident’s postal code (also known as forward sortation area). A total of 180 neighbourhoods are presented. Group 1 includes neighbourhoods with the highest incidence of SARS-CoV-2 infections, whereas group 10 includes neighbourhoods with the lowest incidence of SARS-CoV-2 infections. Data sourced from the Public Health Case and Contact Management Solution and other case management systems (CCM plus), extracted on January 16, 2021.
COVID-19 deaths are strongly associated with an individual’s age and neighbourhood of residence. As of January 16, 2021, 50% of Ontario COVID-19 deaths, outside of LTC and retirement homes, have occurred in just 4% of the population aged 16 years or above. These are represented by the 10 lighter coloured cells in the upper left corner of Figure 4 with an incidence of more than 85 deaths per 100,000 residents.
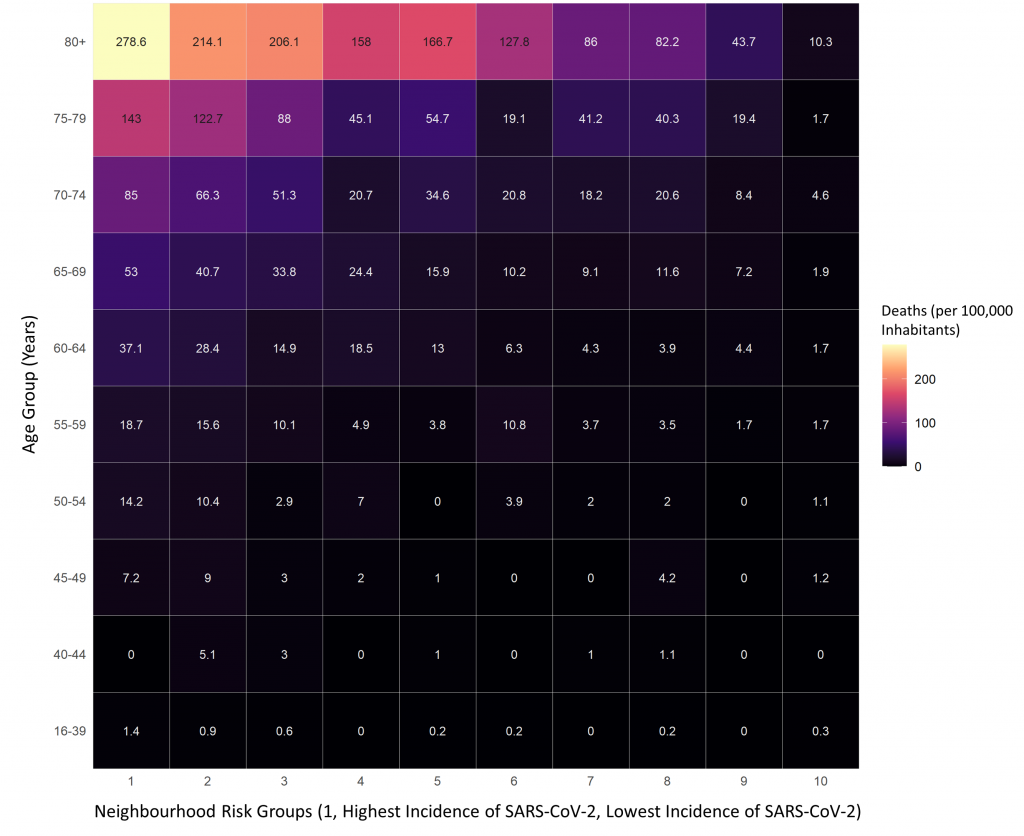
COVID-19 deaths by age and neighbourhood in Ontarians living outside of LTC and retirement homes from January 23, 2020 to January 16, 2021. COVID-19 deaths occurred predominantly in older adults residing in neighbourhoods with the highest cumulative incidence of SARS-CoV-2 infection. Over 50% of deaths occurred in 4% of the population, presented in the 10 cells in the upper left corner of the figure with incidence of more than 85 deaths per 100,000 inhabitants. Data sourced from the Public Health Case and Contact Management Solution and other case management systems (CCM plus), extracted on January 16, 2021; neighbourhood population from the Registered Persons Database (RPDB).
COVID-19 hospitalizations are also strongly associated with an individual’s age and neighbourhood of residence, with 50% of hospitalizations concentrated in 11% of the population aged 16 years or above. These are represented by the 22 lighter coloured cells with more than 160 hospitalizations per 100,000 inhabitants at the top left corner of Figure 5.
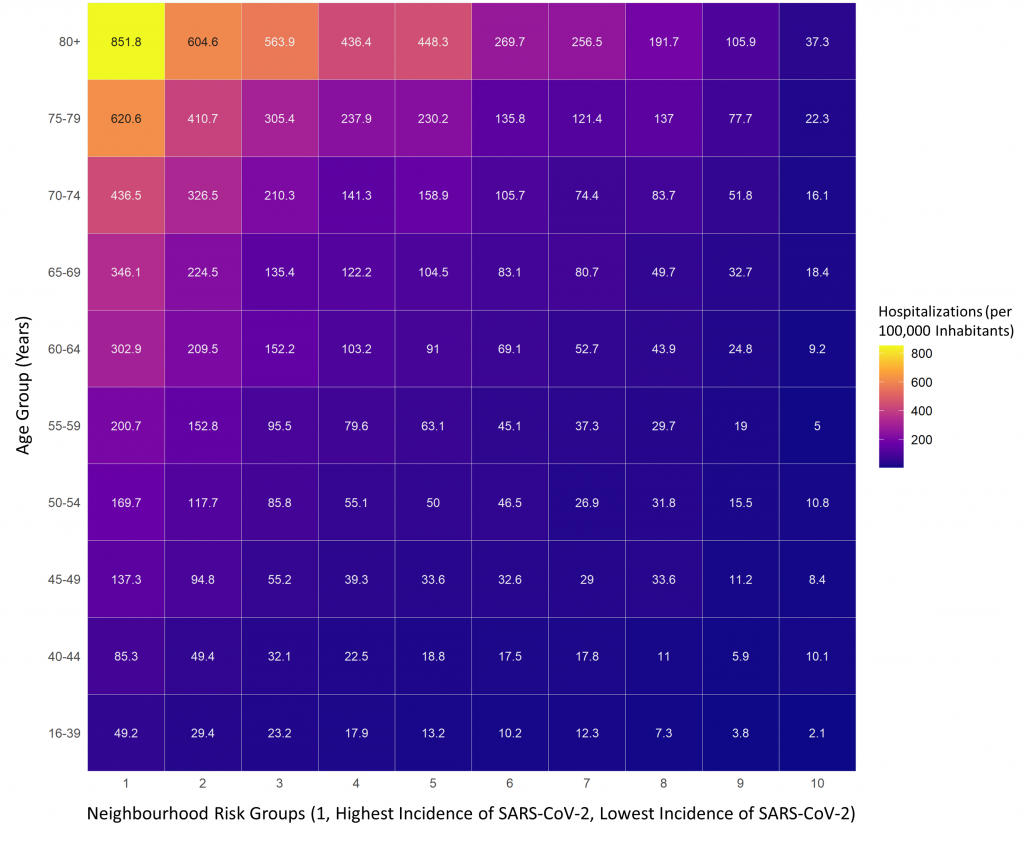
Incidence of COVID-19 hospitalizations by age and neighbourhood in Ontarians living outside of LTC and retirement homes from January 23, 2020 to January 16, 2021. COVID-19 hospitalizations occurred predominantly in older adults residing in neighbourhoods with the highest cumulative incidence of SARS-CoV-2 infection. Over 50% of hospitalizations occurred in approximately 11% of the population, represented by the 22 cells in the upper left corner of the figure with an incidence more than 160 hospitalizations per 100,000 inhabitants. Data sourced from the Public Health Case and Contact Management Solution and other case management systems (CCM plus), extracted on January 16, 2021; neighbourhood population from the Registered Persons Database (RPDB).
Vaccination Strategy Using Age and Neighbourhood-Based Prioritization
In view of the retrospective analysis above, an effective mass vaccine distribution strategy for Ontario should identify people with the highest priority for COVID-19 vaccination based on their age and the neighbourhood they reside in. This will prevent the largest number of deaths and hospitalizations due to COVID-19.
Figure 6 shows the number of deaths or hospitalizations due to COVID-19 that have occurred in Ontarians living outside of LTC and retirement homes between January 23, 2020 and January 16, 2021, which could be used as a blueprint to identify the highest priority individuals for vaccine distribution. There is a 380-fold difference in the frequency of COVID-19 deaths or hospitalizations between the oldest individuals living in neighbourhoods with the highest incidence of SARS-CoV-2 (top left cell of Figure 6), and the youngest individuals living in neighbourhoods with lowest incidence of SARS-CoV-2 (bottom right cell of Figure 6). Additional analyses indicates that the past occurrence of events shown in Figure 6 is highly predictive of the risk of future events in the same neighbourhoods (data available upon request).
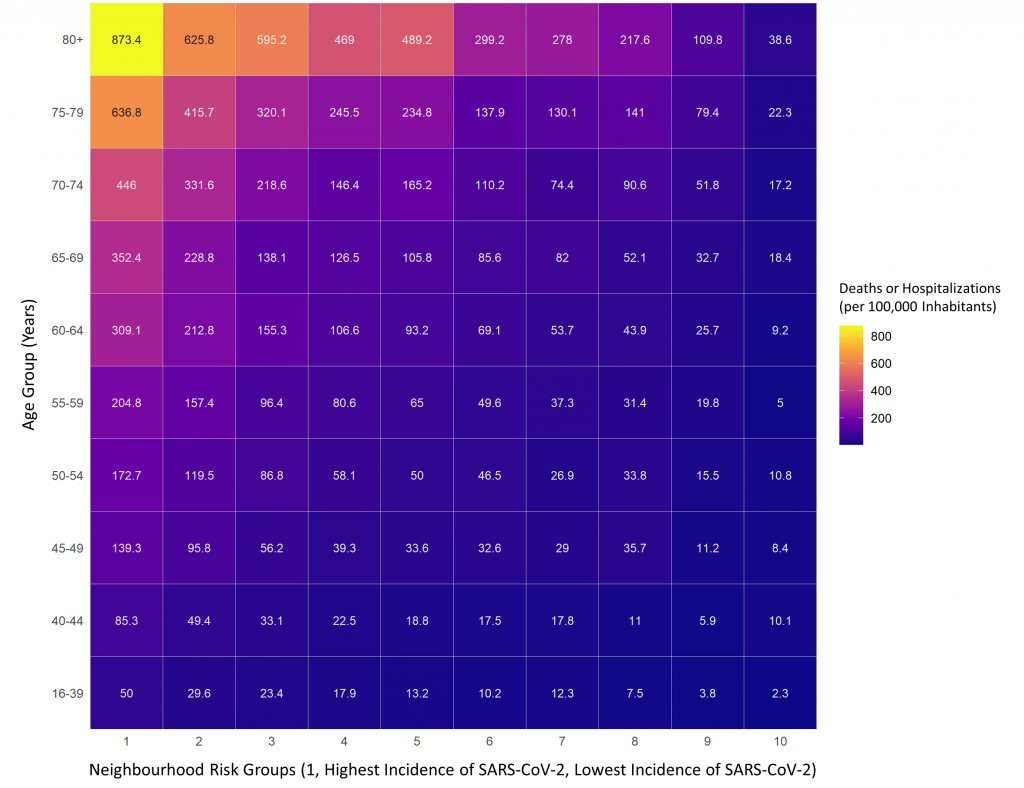
Incidence of COVID-19 deaths or hospitalizations by age and neighbourhood in Ontarians living outside of LTC and retirement homes. COVID-19 deaths or hospitalizations occurred predominantly in older adults residing in neighbourhoods with the highest cumulative incidence of SARS-CoV-2 infection. There is a 380-fold difference in the frequency of COVID-19 deaths or hospitalizations between the population 80 years of age and above living in the highest incidence neighbourhoods (top left cell) and the population between 16 and 39 years of age living in the lowest incidence neighbourhoods (bottom right cell). Data sourced from the Public Health Case and Contact Management Solution and other case management systems (CCM plus), extracted on January 16, 2021; neighbourhood population from the Registered Persons Database (RPDB).
Prioritizing mass vaccine distribution based on both age and neighbourhood of residence will ensure that Ontarians at the highest risk of SARS-CoV-2 infection, hospitalization, or death due to COVID-19 will be the first to receive vaccines. Within each neighbourhood risk group, the age cut-offs for priority of vaccination can be selected depending on the observed risk of death or hospitalization due to COVID-19. Cut-offs of 400, 300, 200 and 100 deaths or hospitalizations per 100,000 inhabitants can be used in descending order to sequentially identify age cut-offs for priority vaccination. Figure 7 is a 3-dimensional representation of the differences in the risk of COVID-19 deaths or hospitalizations observed across age bands and neighbourhood risk groups.
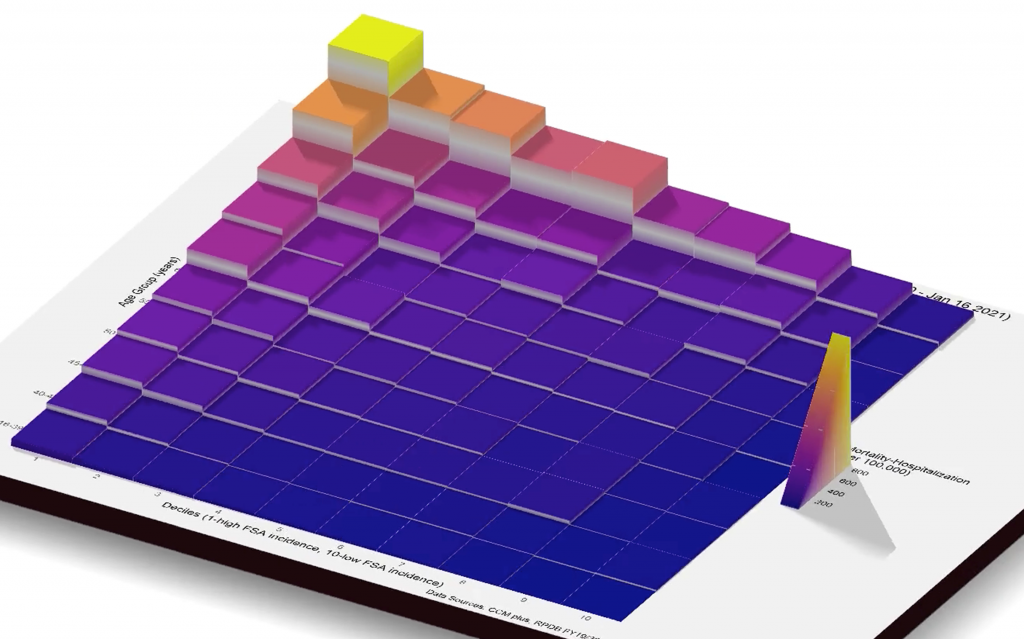
Risk of COVID-19 deaths or hospitalizations by age and neighbourhood in Ontarians living outside of LTC and retirement homes. COVID-19 deaths or hospitalizations occurred predominantly in older adults, especially those residing in neighbourhoods with the highest cumulative incidence of SARS-CoV-2 infection. Data sourced from the Public Health Case and Contact Management Solution and other case management systems (CCM plus), extracted on January 16, 2021; neighbourhood population from the Registered Persons Database (RPDB). See Figure 6 for explanations.
Figure 8 presents projections after most of Ontario moved back to the colour coded COVID-19 response framework for public health measures.8 The scenario takes into account that all Ontario regions had schools return to in-class learning, and all except for Toronto, Peel and North Bay-Parry Sound lifted some of their public health restrictions by February 22, 2021, in accordance with the framework.8 It assumes that the current effective reproduction number (Rt) for the traditional variants originally identified in Wuhan, China, is 1.00 (estimate on February 24, 2021), and that it will gradually increase over 3 weeks to 1.09 (the average Rt found for traditional variants during the first 3 weeks of December 2020). The scenario also assumes that Ontario will return to a province-wide lockdown with a stay-at-home order on March 10, 2021, due to early signs of surging SARS-CoV-2 infections as the more transmissible B.1.1.7 variant, which was first identified in the United Kingdom, becomes the dominant variant in the province.9
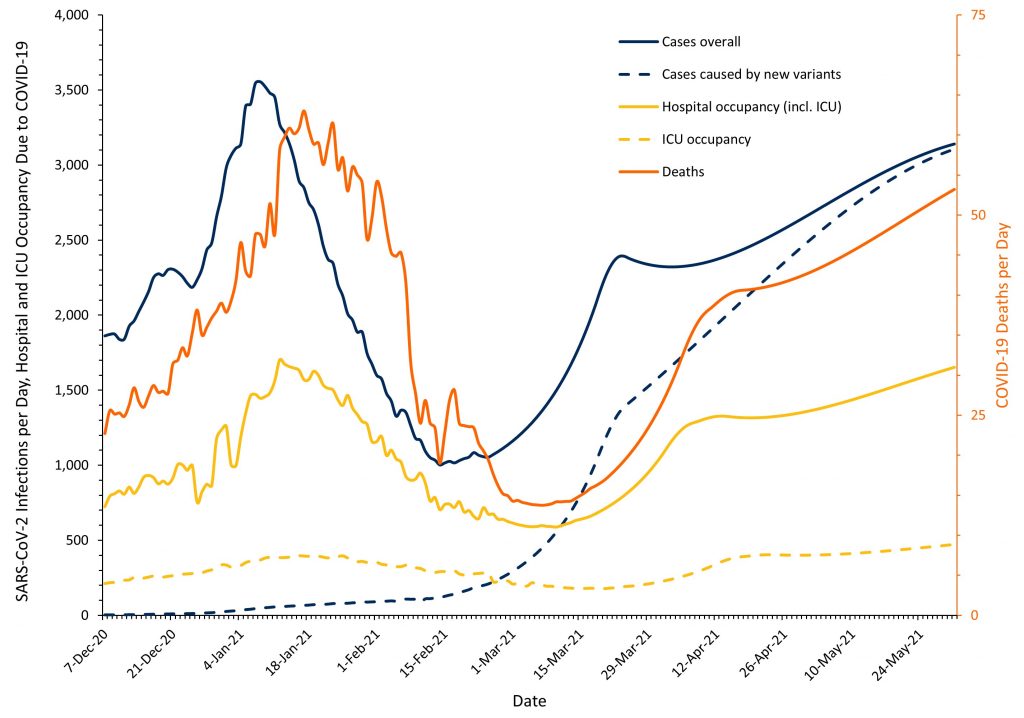
Line graphs presenting the actual and projected rolling 7-day average of SARS-CoV-2 infections overall and due to the B.1.1.7 variant, and COVID-19 hospital occupancy, ICU occupancy, and deaths in Ontario, from December 7, 2020, to May 31, 2021. Note that the scales for SARS-CoV-2 infections, and COVID-19 hospital and ICU occupancy (left) and for COVID-19 deaths per day (right) are different. Outcomes are projected for the period between February 25 and May 31, 2021 under the assumption that no additional vaccination will be administered to Ontarians, except for those administered by February 24, 2021 to residents, staff and caregivers of congregate care settings, frontline healthcare workers, adults in First Nations, Métis, and Inuit populations, and adult chronic home care recipients, and that there will be a province-wide lockdown with a stay-at-home order re-introduced on March 10, 2021. See results section above and methods section below for full assumptions used for the projections.
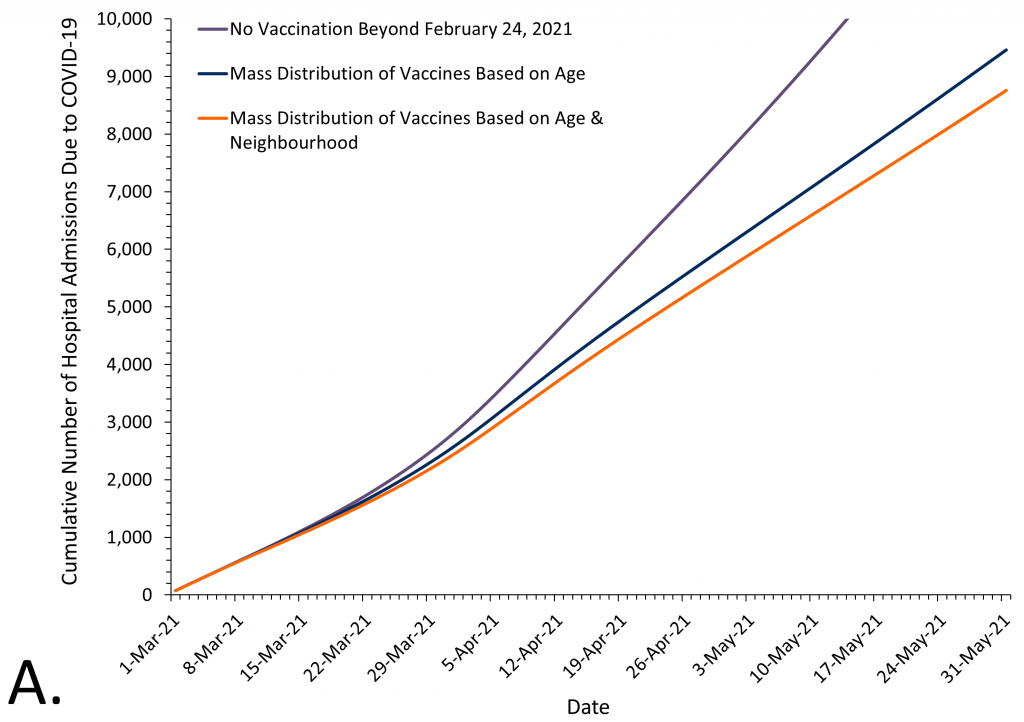
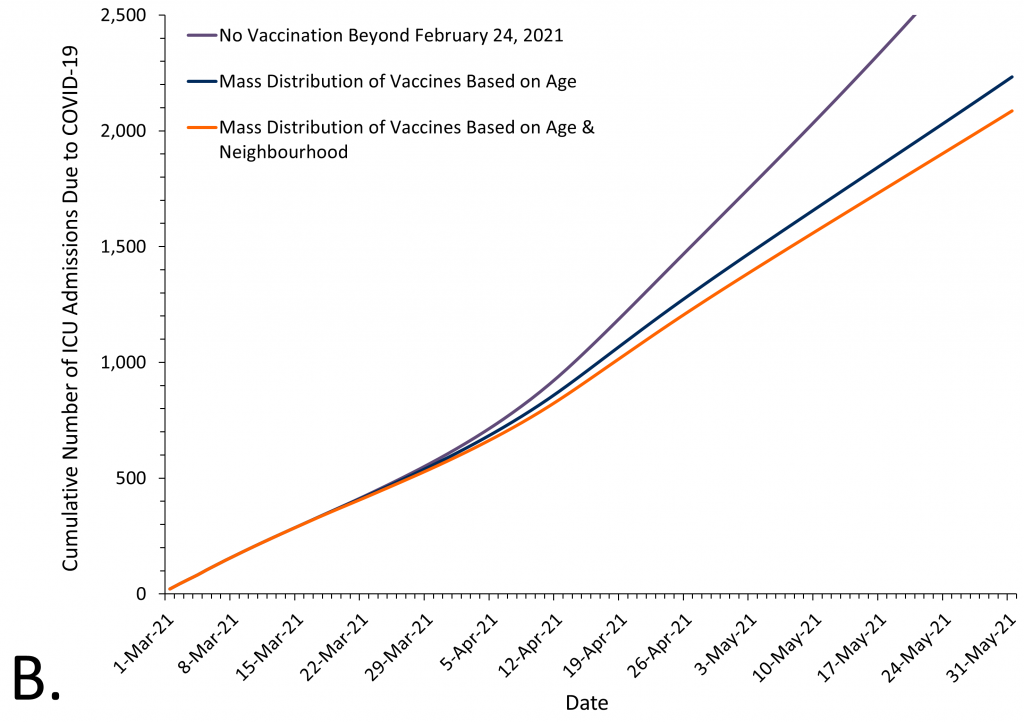
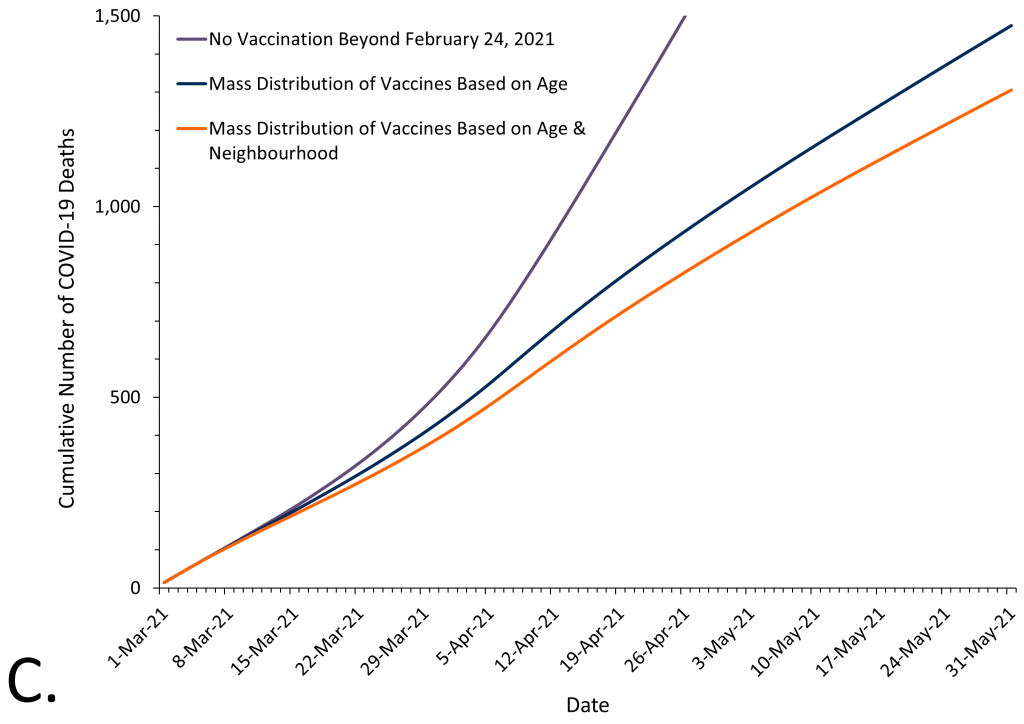
Projected cumulative number of hospitalizations (Panel A), ICU admissions (Panel B) and deaths (Panel C) occurring between March 1 and May 31, 2021, under 3 vaccine mass distribution scenarios. No vaccination refers to the control scenario of no additional vaccines being administered to Ontarians, except for those high-risk individuals vaccinated by February 24, 2021 (residents, staff and caregivers of congregate care settings for older adults, frontline healthcare workers, adults in First Nations, Métis, and Inuit populations, and adult chronic home care recipients). Mass distribution of vaccines based on age refers to a scenario of 1.3 million Ontarians being vaccinated between March 1 and May 20, 2021, using a prioritization framework for mass immunization based on age alone; this scenario assumes equal administration of vaccines across all Ontario neighbourhoods. Mass distribution of vaccines based on age & neighbourhood refers to a scenario of 1.3 million Ontarians being vaccinated between March 1 and May 20, 2021, using a prioritization framework based on both age and neighbourhood. See Figure 7 for base scenario.
Figure 9 shows the projected cumulative number of hospitalizations (Panel A), ICU admissions (Panel B) and deaths (Panel C) between March 1 and May 31, 2021 in Ontario under 3 scenarios. In Scenario 1, no additional vaccines are administered to Ontarians, except for those high-risk individuals vaccinated by February 24, 2021.8,10 In Scenario 2, 1.3 million Ontarians are vaccinated between March 1 and May 20, 2021, using a prioritization framework based on age alone; this scenario assumes equal administration of vaccines across all Ontario neighbourhoods. In Scenario 3, 1.3 million Ontarians being vaccinated between March 1 and May 20, 2021, using a prioritization framework based on both age and neighbourhood.
Table 1 presents estimates of the projected outcomes for all 3 scenarios. The cumulative projected number of events between March 1 and May 31, 2021 is consistently lower with a strategy for the mass distribution of vaccines that prioritizes based on both age and neighbourhood of residence as compared to either a scenario of no additional vaccination beyond February 24, 2021 or a vaccination strategy that prioritizes based on age alone. A vaccine strategy prioritizing both age and neighbourhood will prevent a projected additional 3,767 cases of SARS-CoV-2 infection, 702 hospitalizations, 145 ICU admissions, and 168 deaths from COVID-19 as compared to a strategy that prioritizes based on age alone (Table 1).
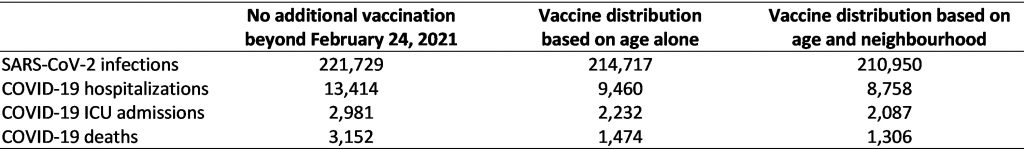
Under three scenarios: 1) no additional vaccination beyond February 24, 2021, 2) vaccine distribution prioritizing age alone, and 3) vaccine distribution prioritizing age and neighbourhood. Note that the estimates for the vaccine distribution strategy based on age alone assume equal administration of vaccines across all Ontario neighbourhoods. This assumption will likely underestimate the number of events, as experience in the United States suggests, that residents of socioeconomically deprived neighbourhoods at high risk of COVID-19 are less likely than residents of socioeconomically advantaged neighbourhoods at low risk of COVID-19 to receive the vaccine.3–6
Interpretation
As of January 16, 2021, 50% of Ontario COVID-19 deaths, outside of LTC and retirement homes, have occurred in just 4% of the population aged 16 years or above. These are represented by the 10 lighter coloured cells in the upper left corner of Figure 4 above. In addition, 50% of hospitalizations have occurred in 11% of the population aged 16 years or above. These are represented by the 22 lighter coloured cells in the top left corner of Figure 5 above. These high risk populations are defined by a combination of an individual’s age and neighbourhood of residence.
A strategy for the mass distribution of COVID-19 vaccines that prioritizes people based on both their age and neighbourhood of residence can reduce cases of SARS-CoV-2 infection, COVID-19 hospitalizations, ICU admissions, and deaths, and will also directly address the inequitable impact of COVID-19 on disadvantaged populations in Ontario.
The age and neighbourhood prioritization strategy is intended to guide the mass distribution of COVID-19 vaccines to the general population.7 The prioritization strategy needs to be combined with efforts to promote equitable administration of COVID-19 vaccines. This includes partnering with trusted community organizations and leaders to promote vaccine awareness and uptake. Simple registration procedures are essential, including options that do not require the internet or digital platforms, such as phone-based or in-person registration. Registration also needs to be accessible to those with limited English or French language proficiency, poor literacy, and those with cognitive or sensory impairments. Additional options that do not require pre-registration or government-issued identification are important. Vaccination centres should be located in local community centers, schools, houses of worship, or other highly frequented and trusted sites in the community. Centres should be accessible and located near public transportation. Hours of operation should extend beyond standard business hours. Mobile outreach options are required for individuals who cannot access vaccination centres due to mobility, transportation or other barriers.3–6
Importantly, the suggested mass distribution strategy would not interfere with the ongoing vaccination of any specific high-risk population prioritized for initial receipt of COVID-19 vaccines,11 including residents, staff and caregivers in congregate care settings; frontline healthcare workers; adults in First Nations, Métis, and Inuit populations; adult chronic home care recipients; and people aged 80 years or older irrespective of their neighbourhood of residence.
The strategy will also not interfere with Ontario’s planned vaccination of high-risk populations prioritized for subsequent receipt of COVID-19 vaccines, including people who live and work in high-risk congregate settings (e.g., shelters, community living), individuals with high-risk chronic conditions and their caregivers, other specific populations and communities beyond those identified in this strategy facing barriers related to the social determinants of health who are at greater risk of COVID-19, and frontline essential workers, including first responders, teachers and other education staff and the food processing industry.11–13 Age cut-offs could be used for the prioritization of high-risk essential workers who have similar risk of exposure to residents of high incidence neighbourhoods, regardless of their neighbourhood of residence, but based on their place of work (Figure 6).
Differences between a mass vaccine distribution strategy that prioritizes people based on both their age and neighbourhood of residence and a strategy based on age alone will become larger in the context of vaccine scarcity, with increasing duration of the vaccine rollout beyond May 31, 2021, if the daily incidence of SARS-CoV-2 cases increases, if vaccination also protects against asymptomatic infection and transmission,14 and if an age-based strategy is inequitable, resulting in higher vaccination rates in wealthier neighbourhoods, as currently observed in the United States.3,4
Methods Used for This Science Brief
We conducted a population-level retrospective cohort study and developed a data-driven predictive model of the potential impacts of different strategies for the mass distribution of COVID-19 vaccines in Ontario. All analyses were based on SARS-CoV-2 cases, COVID-19 hospitalizations, and COVID-19 death data retrieved from the Public Health Case and Contact Management Solution and other case management systems (CCM plus) reported between January 23, 2020 and January 16, 2021. Cases in LTC and retirement homes were excluded. Neighbourhood of residence was defined by 526 unique forward sortation areas (FSAs), the first 3 digits of a resident’s postal code. FSAs with less than 1,000 residents were merged with adjacent neighbourhoods to ensure accurate prediction of SARS-CoV-2 incidence, yielding 509 unique neighbourhoods. Age-specific population data by FSA were obtained from the Registered Persons Database (RPDB) Fiscal Year 2019/2020.
Age was classified into 10 age bands (16-39, 40-44, 45-49, 50-54, 55-59, 60-64, 65-69, 70-74, 75-79, and ≥80 years of age). Neighbourhood cumulative SARS-CoV-2 incidence was classified into 10 neighbourhood risk groups with equal populations based on the observed cumulative incidence of SARS-CoV-2 infection from the beginning of the COVID-19 pandemic (January 23, 2020) until January 16, 2021. The combination of the 10 age bands and 10 neighbourhood risk groups resulted in a matrix of 100 cells. For each cell, we calculated the rate of COVID-19 deaths, the rate of COVID-19 hospitalizations and the rate of the composite of COVID-19 hospitalizations or deaths due to COVID-19 per 100,000 inhabitants using the Public Health Case and Contact Management Solution and other case management systems (CCM plus). This data has demonstrated accuracy in identifying deaths and hospitalizations among COVID-19 cases in Ontario.15
We evaluated three scenarios: (1) an assumption that no additional vaccines would be administered to Ontarians, except for those administered by February 24, 2021 to residents, staff and caregivers in congregate care settings for older adults, frontline healthcare workers, adults in First Nations, Métis, and Inuit populations, and adult chronic home care recipients (control scenario); (2) an assumption that 2.2 million vaccine doses would be administered to 1.3 million Ontarians over a 13-week period between March 1 and May 31, 2021 with vaccination of 100,000 people per week, prioritizing by age based on the above 10 age bands; (3) an assumption that 2.2 million vaccine doses would be administered to 1.3 million Ontarians over a 13-week period between March 1 and May 31, with vaccination of 100,000 people per week, prioritizing by both age and neighbourhood of residence based on the 100 cells shown in Figure 6. For the third scenario, vaccination priority was based on the ranked incidence rate per 100,000 inhabitants of the composite outcome of hospitalization or death due to COVID-19.
We assumed that all Ontarians received mRNA-based vaccines, which as of February 25, 2021, are the only COVID-19 vaccines currently approved by Health Canada. Based on trial data, we defined COVID-19 vaccine efficacy to be 0% in the week after the first dose, 70% in week 2 post-vaccination, 85% in weeks 3-4 post vaccination, 90% in week 5 post-vaccination, and 95% thereafter.16 We assumed that all vaccinated individuals received the second vaccine dose within approved schedules,17 and that there were no indirect vaccine effects (i.e. we assumed no herd immunity effects).16,18
We modelled the effectiveness of prioritization strategies in scenarios 2 and 3 as compared with control scenario 1 using public health surveillance data limited to the second wave of the COVID-19 pandemic, from September 1, 2020 to January 16, 2021. These analyses yielded daily projections for the entire 13-week vaccination period, fromMarch 1toMay 31, 2021, and allowed us to estimate daily rate ratios comparing scenarios 2 and 3 with control scenario 1. The modelling process had five steps and was based on regression models that were fit using the gamm4 package in R.
First, a regression model of predicted baseline incidence of SARS-CoV-2 infections was developed. The prospective model estimated the predicted SARS-CoV-2 incidence in all Ontario neighbourhoods as a function of cumulative incidence from the onset of the pandemic (January 23, 2020) until January 9, 2021. The prediction model was based on a dataset of weekly neighbourhood SARS-CoV-2 incidence, using a logistic count regression model. The model had a random intercept to account for variation between neighbourhoods, and a penalized spline for time. Based on this model, we estimated SARS-CoV-2 incidence deciles. Second, we predicted the incidence of SARS-CoV-2 infections across the 100 cells defined by neighbourhood risk and age band, using a tensor spline for the interaction of neighbourhood risk and age.19 Third, we developed logistic count regression models for the risk of COVID-19 hospitalization and death, among SARS-CoV-2 cases, which yielded the probability of an event given case status. Fourth, we sorted cells defined by age bands and neighbourhood risk groups from most to least likely to experience the composite outcome of COVID-19 hospitalization or death. Based on this ranking we sequentially determined, from March 1, 2021 onwards, the Ontarians prioritized to receive the first dose of the COVID-19 vaccine each week, followed by the second dose within approved schedules. Fifth, we projected the incidence forward based on baseline SARS-CoV-2 incidence in risk group x age bands, and age band specific vaccination levels and estimated daily rate ratios for scenario 2 as compared with control scenario 1, and for scenario 3 as compared with control scenario 1.
Then, we used a deterministic, non-mechanistic model to project daily updated plausible estimates of the incidence of COVID-19 cases and deaths, and of hospital and ICU occupancy due to COVID-19 between February 25 and May 31, 2021, using the following assumptions: First, there would be a linear increase in the log of the effective reproduction number Rt for the traditional variant, originally identified in Wuhan, China, associated with school openings and opening of the province from log(1.00) as estimated on February 24, 2021, to log(1.09) three weeks later, with 1.09 reflecting the geometric mean Rt observed in Ontario for traditional variants during the 3 weeks between December 1 and December 21, 2020. Second, the province would go back into a lockdown with a province-wide stay-at-home order starting on March 10, 2021, which would result in a decrease of Rt for the traditional variants to 0.82 starting on March 20, 2021, 10 days after the lockdown. An Rt of 0.82 reflects the geometric mean found for the traditional variants during the 3 weeks between January 15 and February 4, 2021. Fourth, the B.1.1.7 variant would be 40% more transmissible than traditional variants and would continue to follow a logarithmic growth curve with a doubling time for the odds of 11.3 days, as observed between January 21 and February 24, 2021. We conservatively assumed that this doubling time would remain constant over time and would not be shortened by school openings and the opening of the province. Fifth, daily hospital occupancy (including ICU) from COVID-19 would be 5.7% of daily active cases, with 5.7% reflecting the mean percentage observed between December 24, 2020, and February 24, 2021, with an assumed time lag of 10 days between daily active cases and daily hospital occupancy, and a mean duration of 10 days for cases to be considered active. Sixth, daily ICU occupancy would be at 30.5% of hospital occupancy due to COVID-19, the mean percentage observed between December 8, 2020, and February 24, 2021, with a time lag of 10 days between daily hospital occupancy and daily ICU occupancy. Seventh, daily deaths caused by the traditional variants would be at 0.14% of daily active cases, which reflects the mean percentage observed during the three weeks between February 1 and February 21, 2021, after the vaccine distribution in LTC and retirement homes became partially effective, and the assumption that deaths would be further reduced by 10% once the vaccine distribution in LTC and retirement homes became fully effective. Seventh, there would be a relative increase in mortality of 30% associated with the B.1.1.7 variant as compared with the traditional variants. Eighth, Rt would be modified by seasonal changes in accordance with the inverse pattern observed in Ontario between August 1 and December 31, 2020, resulting in a progressive reduction of log(Rt) between March 1 and May 31, 2021.20
We multiplied the daily estimates of incidence of SARS-CoV-2 infections, hospital occupancy and deaths from COVID-19 with the daily rate ratios derived for scenarios 2 and 3 for vaccine distribution, and derived cumulative incidence curves of deaths, hospitalizations and ICU admissions, and the cumulative numbers of SARS-CoV-2 cases, and COVID-19 hospitalizations, ICU admissions, and deaths between March 1 and May 31, 2021.
References
1. Bonanad C, García-Blas S, Tarazona-Santabalbina F, et al. The Effect of Age on Mortality in Patients With COVID-19: A Meta-Analysis With 611,583 Subjects. J Am Med Dir Assoc. 2020;21(7):915-918. https://doi.org/10.1016/j.jamda.2020.05.045
2. van Ingen T, Brown KA, Buchan SA, Akingbola S, Daneman N, Smith BT. Neighbourhood-Level Risk Factors of COVID-19 Incidence and Mortality. Epidemiology; 2021. https://doi.org/10.1101/2021.01.27.21250618
3. Salmon D, Opel DJ, Dudley MZ, Brewer J, Breiman R. Reflections On Governance, Communication, And Equity: Challenges And Opportunities In COVID-19 Vaccination: Article examines the engagement and communication steps necessary to strengthen the COVID-19 vaccine roll out by federal, state, and local governments. Health Aff (Millwood). Published online February 4, 2021:10.1377/hlthaff. https://doi.org/10.1377/hlthaff.2020.02254
4. Bachireddy C, Dar M, Chen C. Medicaid and COVID-19 Vaccination—Translating Equitable Allocation Into Equitable Administration. JAMA Health Forum. 2021;2(2):e210114. https://doi.org/10.1001/jamahealthforum.2021.0114
5. Jean-Jacques M, Bauchner H. Vaccine Distribution—Equity Left Behind? JAMA. Published online January 29, 2021. https://doi.org/10.1001/jama.2021.1205
6. Bibbins-Domingo K, Petersen M, Havlir D. Taking Vaccine to Where the Virus Is—Equity and Effectiveness in Coronavirus Vaccinations. JAMA Health Forum. 2021;2(2):e210213. https://doi.org/10.1001/jamahealthforum.2021.0213
7. Government of Ontario. COVID-19 vaccination update. Technical Briefing presented at the: January 13, 2021; Ontario. Accessed January 19, 2020. https://files.ontario.ca/moh-covid-19-vaccine-technical-briefing-en-january-13-2021-2021-01-13.pdf
8. Government of Ontario. COVID-19 response framework: keeping Ontario safe and open. Ontario.ca. Published January 14, 2021. Accessed December 6, 2020. https://www.ontario.ca/page/covid-19-response-framework-keeping-ontario-safe-and-open
9. Brown KA, Gubbay J, Hopkins J, et al. Rapid Rise of S-Gene Target Failure and the UK variant B.1.1.7 among COVID-19 isolates in the Greater Toronto Area, Canada. medRxiv. Published online February 12, 2021:2021.02.09.21251225. https://doi.org/10.1101/2021.02.09.21251225
10. Stall NM, McGeer A, Maltsev A, et al. The impact of the speed of vaccine rollout on COVID-19 cases and deaths in Ontario long-term care homes. Sci Briefs Ont COVID-19 Sci Advis Table. 2021;2(8). https://doi.org/10.47326/ocsat.2021.02.08.1.0
11. Government of Ontario. Getting a COVID-19 vaccine in Ontario. COVID-19 (coronavirus) in Ontario. Published 2021. Accessed February 17, 2021. https://covid-19.ontario.ca/getting-covid-19-vaccine-ontario
12. Chen Y-H, Glymour M, Riley A, et al. Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: March through October 2020. medRxiv. Published online January 22, 2021:2021.01.21.21250266. https://doi.org/10.1101/2021.01.21.21250266
13. Murti M, Achonu C, Smith BT, et al. COVID-19 Workplace Outbreaks by Industry Sector and their Associated Household Transmission, Ontario, Canada, January – June, 2020. medRxiv. Published online November 30, 2020:2020.11.25.20239038. https://doi.org/10.1101/2020.11.25.20239038
14. Amit S, Regev-Yochay G, Afek A, Kreiss Y, Leshem E. Early rate reductions of SARS-CoV-2 infection and COVID-19 in BNT162b2 vaccine recipients. The Lancet. 2021;0(0). https://doi.org/10.1016/S0140-6736(21)00448-7
15. Chung H. Validation of COVID-19 Outcomes in Public Health Surveillance Data using Health Administrative Databases. Published online October 21, 2020.
16. Jüni P, Tuite AR, Bogoch II, et al. Rollout strategy for the Pfizer-BioNTech COVID-19 vaccine in Ontario. Sci Briefs Ont COVID-19 Sci Advis Table. 2021;2(6). https://doi.org/10.47326/ocsat.2021.02.06.1.0
17. Public Health Agency of Canada. Recommendations on the use of COVID-19 vaccines. Published December 14, 2020. Accessed February 11, 2021. https://www.canada.ca/en/public-health/services/immunization/national-advisory-committee-on-immunization-naci/recommendations-use-covid-19-vaccines.html
18. Polack FP, Thomas SJ, Kitchin N, et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med. 2020;383(27):2603-2615. https://doi.org/10.1056/NEJMoa2034577
19. Pedersen EJ, Miller DL, Simpson GL, Ross N. Hierarchical generalized additive models in ecology: an introduction with mgcv. PeerJ. 2019;7:e6876. https://doi.org/10.7717/peerj.6876
20. Brown KA, Soucy J-PR, Buchan SA, et al. The mobility gap: estimating mobility levels required to control Canada’s winter COVID-19 surge. medRxiv. Published online February 1, 2021:2021.01.28.21250622. https://doi.org/10.1101/2021.01.28.21250622
Document Information & Citation
Author Contributions: KAB and PJ conceived of the Science Brief. KAB, NMS, and PJ wrote the first draft. EJ, TVI, SB, PJ, and KAB conducted the analysis. All authors contributed to the interpretation of analyses, revised the Science Brief critically for important intellectual content and approved the final version.
The authors would like to thank Carmen Kong for creating the maps presented in this Science Brief.
Updated on March 1, 2021. Version 1.0 is available under Additional Resources.
Citation: Brown KA, Stall NM, Joh E, et al. A strategy for the mass distribution of COVID-19 vaccines in Ontario based on age and neighbourhood. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;2(10). https://doi.org/10.47326/ocsat.2021.02.10.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table can be found at www.covid19-sciencetable.ca.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, and its partners.
Additional Resources
How a shift in COVID-19 vaccine strategy could save more lives, Toronto Star
LILLEY: Good news on vaccine front changes Ontario’s plans once again, Toronto Sun
Vulnerable Toronto neighbourhoods push for priority access to COVID-19 vaccines, CBC
As Biden pushes for racial equity in vaccination, data is lagging, The New York Times
