Key Message
Overall confidence in COVID-19 vaccines amongst Ontarians has remained within the range of 72% to 76%. It is important to understand which individuals and groups have lower vaccine confidence, and why, as this knowledge can support a tailored and informed response.
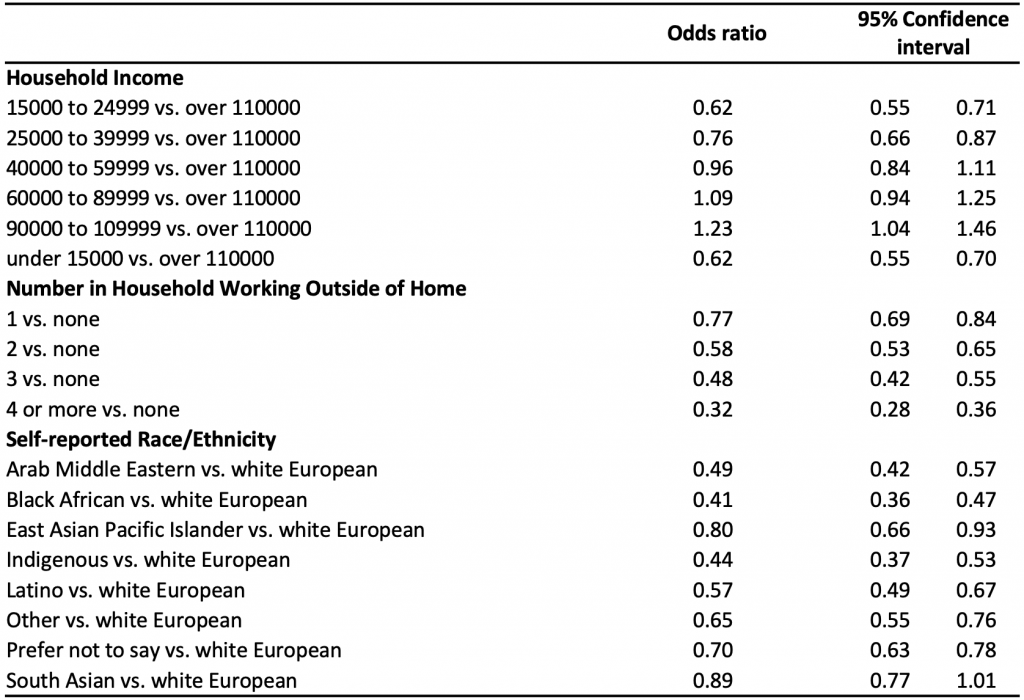
Survey data from 28,660 Ontarians reveal that individuals with lower confidence in COVID-19 vaccines tend to have a lower household income, are more likely to be unable to work from home, and self-identify as racialized (a race other than white European). Lower vaccine confidence is associated with a complex set of factors including health inequities, systemic barriers to accessing health care, and mistrust in government and health care institutions.
Community-level strategies, outreach, and interventions can address the drivers of lower vaccine confidence. These strategies include engagement with local leaders, and partnerships with trusted individuals and organizations to build confidence and drive increased vaccine uptake.
Summary
Background
All Ontarians over the age of 12 years have been eligible for COVID-19 vaccines as of May 23, 2021. As of October 5, 2021, 11,299,600 (86.7%) eligible individuals in Ontario have received their first dose, and 10,649,353 (81.7%) have received two doses of a COVID-19 vaccine.1
While mandatory vaccination or reporting of vaccination status is required in a growing number of settings, vaccination ultimately remains an individual choice. The decision to get vaccinated is multifactorial, and influenced by a combination of capability, opportunity, and motivation (key determinants of behaviour).2,3 Vaccine uptake in Ontario has been lower among racialized communities, especially in areas with the highest proportions of refugees, recent immigrants, and recent OHIP registrants — communities that have also been the most impacted by SARS-CoV-2 infections.4–6 Effective and efficient tailored community outreach programs that aim to increase population-level vaccine coverage can be informed by an understanding of the populations with the highest rate of vaccine hesitancy.
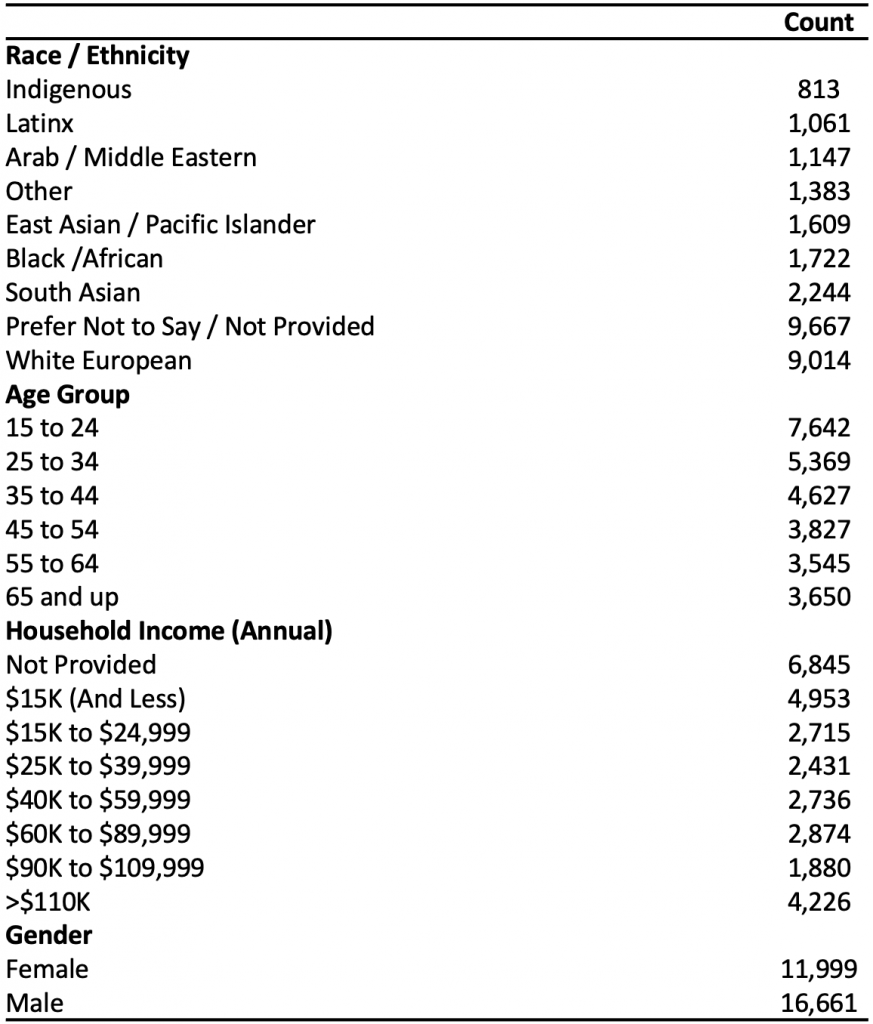
The Fields Institute for Research in Mathematical Sciences developed and administered an internet-based survey to better understand Ontarians’ views, knowledge, and engagement with COVID-19 public health measures, as well as their plans to get a COVID-19 vaccine. Household income, ethnic background, and the number of individuals in the household working outside of the home were self-reported by respondents. The survey was launched on December 9, 2020 and concluded at days end June 30, 2021. During this period, 28,660 Ontarians between the ages of 15 to 98 completed the survey of English-language, multiple-choice questions. The survey was administered by RIWI, an Ontario-based third-party provider that surveys online consumers about sentiment, knowledge, and attitudes. This Brief presents some of the findings from the survey data applicable to vaccination. This Brief also includes some key strategies to enhance messaging to those communities among whom the survey has identified lower rates of vaccine confidence.
Questions
What does the survey data reveal about the proportion of Ontarians choosing to get a COVID-19 vaccine, and has this proportion changed over time?
Are there specific groups among whom vaccine hesitancy is higher?
Using the information gathered from the survey data, what specific strategies can community leaders use to help increase COVID-19 vaccine uptake in these groups?
Findings
COVID-19 Vaccine Confidence in Ontario
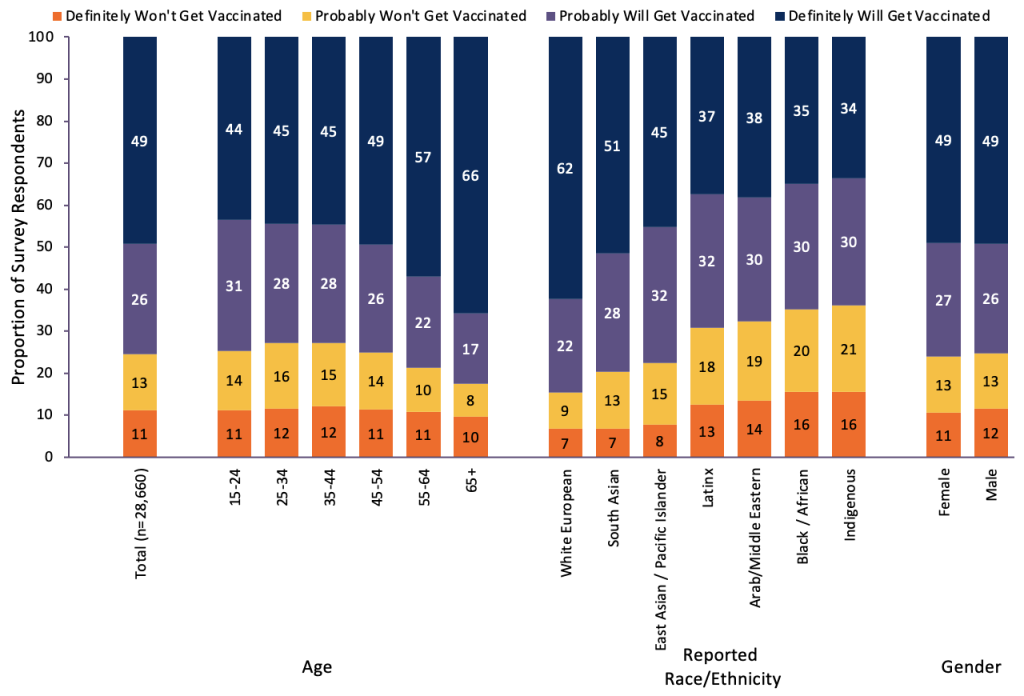
Between December 2020 and June 2021, 28,660 Ontarians completed a survey. Demographics of the respondents are presented in Table 1. Over 75% of respondents were vaccine confident, with 26% reporting they would “probably get vaccinated,” and 49% reporting they would “definitely get vaccinated.” Among those reporting they were unlikely to get a vaccine against COVID-19, 11% reported they would “definitely not get vaccinated,” and 13% reported they would “probably not get vaccinated.”
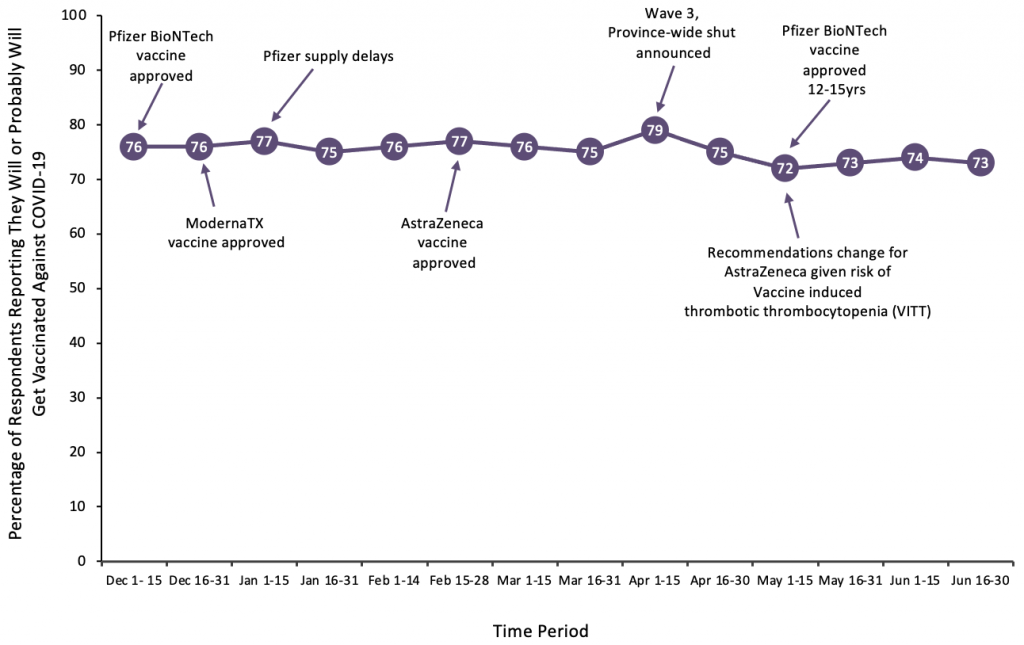
Overall, vaccine confidence in Ontario has remained relatively stable in the period since COVID-19 vaccines were approved for use in Canada. Vaccine confidence has ranged from 72% and 79% between December 2020 and June 2021. Vaccine confidence was highest in early April 2021, corresponding to the peak of Wave 3, when the province was reporting between 3,000 – 4,000 daily new cases of COVID-19 and there were over 700 individuals with COVID-19 related critical illness in Ontario critical care units.1 Conversely, vaccine confidence was lowest during periods of uncertainty related to COVID-19 vaccines, either due to supply issues (January 2021) or concerns over safety (May 2021). Overall, 76% of respondents surveyed were vaccine confident, and despite ongoing public messaging about the importance of vaccination, there appears to be a vaccine confidence ceiling.
Demographic and Regional Associations with COVID-19 Vaccine Confidence
Aggregated survey results demonstrate that those who self-identify as a visible minority, who have a lower self-reported household income, and who live in a household with a greater number of people working outside of the home, reported higher, lower levels of vaccine confidence.
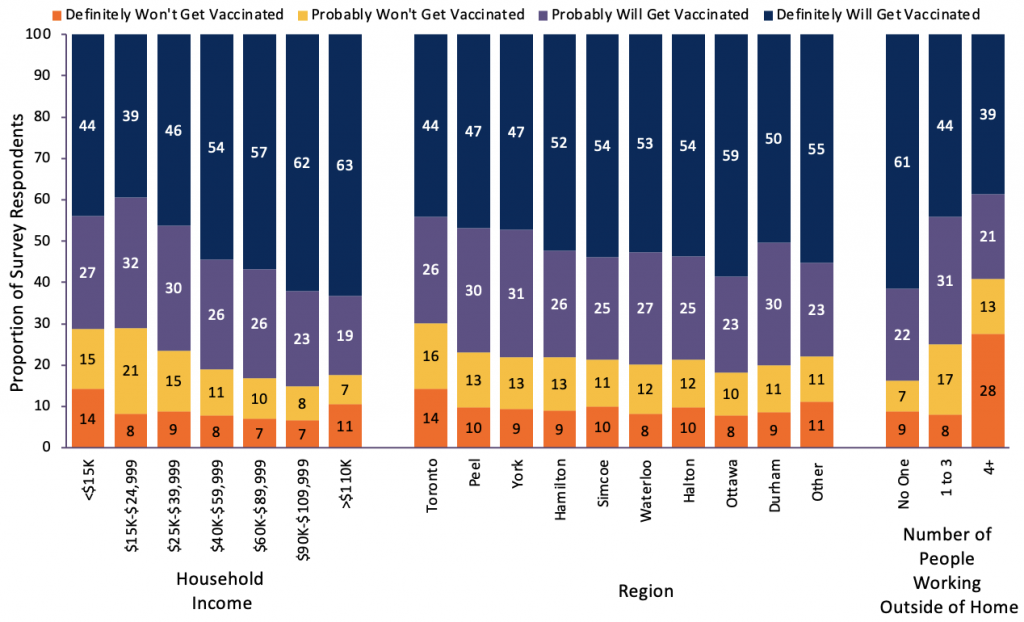
Table 2 presents the results of multivariable logistic regression analyses conducted to determine the independent association between survey respondents’ self-reported demographics (race/ethnicity, household income, and number of people in the household working outside the home) and the odds of being vaccine confident (definitely or probably going to get vaccinated). A statistically significant decrease in the odds of being vaccine confident was found among those with lower household income, with increasing numbers of people in the household unable to work from home, and self-identifying as a race other than white European.
Interpretation
The results of a survey of 28,660 individuals in Ontario demonstrate fairly consistent levels of confidence in COVID-19 vaccines over time (72%-76%). However, there is a statistically significant difference in vaccine confidence between specific groups. Individuals identifying as non-white European, from lower income households, and with a higher number of individuals working outside the home had a statistically significant lower odds of being vaccine confident.
Ontario data show a higher risk for SARS-CoV-2 exposure and infection among racialized and low-income communities.7York, Peel and Toronto have seen the highest rates of cases per capita.7 Workplace outbreaks have contributed to a significant number of cases.8 Concerningly, the results of this survey demonstrate that vaccine hesitancy is highest among these same groups for whom there has been a disproportionate burden of COVID-19 outcomes, and in whom vaccination will prevent more infections and severe outcomes.9
While other Canadian surveys have shown higher rates of overall confidence in COVID-19 vaccines,10 we believe that the larger sample size and the granularity of choice (allowing respondents to indicate how confident they were in their choice to either get vaccinated or not get vaccinated), provides an accurate picture of the attitudes of Ontario’s residents over the period of data collected. Furthermore, the results have been relatively consistent over time, with a ceiling of 79% confidence, representing the maximum percentage of people willing and able to be vaccinated. These results therefore underscore a need for additional, tailored strategies that better support those that remain uncertain.
Ontario launched the “Last Mile Strategy” in August 2021 to increase COVID-19 vaccination uptake for individuals who have not yet received their first or second dose, and in communities and groups with lower vaccination rates.11 This strategy partners with public health units to offer community-based and easy-to-access settings for vaccination such as mobile clinics and smaller, accessible clinics tailored to specific community needs.
Community and public health leaders working to increase vaccine uptake in identified communities are encouraged to employ strategies that aim to increase the capability, opportunity, and motivation to get vaccinated. A case study from the Black Scientists’ Taskforce demonstrates that community-specific interventions can be highly effective.
Specific Strategies Community Leaders Can Use to Help Increase Vaccine Uptake in These Groups: Case Study of the Black Scientists’ Taskforce on Vaccine Equity
Community-tailored engagement, outreach, and interventions are important to address the drivers of hesitancy and increase vaccine uptake in certain groups. A previous science Brief outlined key strategies that could be employed to enhance capability, opportunity, and motivation to get vaccinated in the general population.12 In this section, using the Black Scientists Taskforce on Vaccine Equity as a case study, we show how tailored and community-specific interventions can be developed to help improve vaccine confidence.
The research and engagement conducted by the Black Scientists’ Taskforce on Vaccine Equity offers an illustrative example of such strategies vis-a-vis Black communities in Toronto, Ontario. The Black Scientists’ Taskforce on Vaccine Equity conducted a series of weekly COVID-19 townhalls from February 1 to June 9,13 2021 to better understand low levels of vaccine confidence in the Black community. On average, 339 people were in attendance in each session, with a total attendance of 6785 people. During the events, people asked questions regarding COVID-19 vaccines, shared their opinions, and made suggestions to advance racial and vaccine equity.13
Importantly, this approach shifted away from the concept of hesitancy and instead was focused on understanding and working to address the complex historical, environmental, and societal factors that drive mistrust. Table 3 summarizes behavioral science strategies to support vaccine intention. Community engagement, outreach, and culturally responsive listening determined that vaccine hesitancy in the Black community grew out of historical mistrust with health care institutions and government, concerns for the safety of vaccines, contemporary experiences with anti-Black racism, and mixed messaging from mainstream media.
| Vaccination Intention Barriers/Enablers | Principle12 | Behavioural Science Suggestions12 | Cases Study Example of Black Scientists’ Taskforce |
| Capability | |||
| Concerns about speed of vaccine development, approval, and racial diversity in clinical trials. Perceptions about natural immunity. | Principle 1: Explain how vaccines were able to be developed and approved both quickly and safely. | Describe vaccine development and safety processes, and monitoring systems. Address misinformation and conspiracy theories with empathy and respect. | Task Force members were available to answer questions, showing the assurance of commitment. Focus on sharing scientific facts in lay terminology to maximize understanding. Task Force members sharing their own personal stories created a unique narrative of culturally and scientifically grounded wisdom. |
| Opportunity | |||
| Participation of trusted community organizations and leaders (e.g. faith leaders, community elders, service providers). | Principle 2: Leverage trusted sources in the community. | Community engagement delivered by trusted neighbourhood ambassadors, aimed at educating residents about vaccines and addressing sources of mistrust and confidence issues. Culturally responsive principles shared and accepted by participants should ground discussions: commitment to these principles contribute to trust-building and allow for difficult conversations about perceived problems with vaccines. Respectful conversations can highlight discrepancies of disease versus vaccine risks. Virtual town halls to have community conversations. However, this method will only work if the conversations aim to build participants’ efficacy for informed vaccine decision-making. | At the onset, the Task Force met with faith leaders, community elders, and Black service providers to get a sense of community concerns and understanding regarding the risks of COVID-19 and related vaccines. These meetings allowed for open discussions about COVID-19 impacts and insights from Black service providers about public health. Following the advice of community and health care leaders, the Task Force conducted some grassroots community engagement by sponsoring a range of Kwanzaa holiday activities put together by different community organizations to share COVID-19 information, hear from people about whether they would welcome vaccine conversations, and assess approaches for engagement. The town halls were organized in partnership with community organizations, with local leaders serving as moderators and facilitators. |
| Historical mistrust of healthcare institutions and governments. Experience with systemic racism. | Principle 3: Recognize the role that historical medical mistrust plays and allow time to address it. | Community-tailored engagement is important to determine the best approach for addressing vaccine mistrust. | The Task Force began by reframing the term ‘hesitancy’ and removing blame on individuals who have legitimate trust concerns. The Task Force also identified and prioritized vulnerable community members. These groups included seniors, farmworkers, childcare staff, congregate care facility workers, educators, LGBTQ+ etc. |
| Motivation | |||
| Vaccine safety concerns (e.g. side effects, safety for pregnant or breastfeeding people, fertility, interaction with other medicine). Mixed messaging from the media. | Principle 4:12 Use effective risk communication tools to clarify risk and severity of COVID-19 and vaccine side effects. | Among Canadians who have some hesitancy, safety concerns are among the main reasons, regardless of race. Leverage trusted individuals from diverse communities who can clearly communicate risk information. Outreach is an essential first step for understanding community members’ needs, issues, and perspectives on COVID-19 vaccination safety concerns. | Concerns about fertility are prevalent in the Black community. The iterative approach taken by the Task Force allows for the flexibility required as a result of the fluid nature of the vaccine rollout and a slowdown in vaccine uptake due to mixed messaging from decision-makers. |
| Leveraging extrinsic motivations may help when paired with other strategies. | Principle 5: Consider incentives14and contingent rewards15 that link vaccination to personal values and priorities. | Providing music, food, and vaccination souvenirs can attract both vaccine confident and the more hesitant members of the community. | At all three Black-focused clinics in the Greater Toronto Area, organizers welcomed both those who were vaccine confident and vaccine hesitant. The organizers competently reinforced vaccine confidence with culturally responsive messaging in clinics. |
Based on these insights, community-level strategies were developed and deployed to address health inequities and trust concerns that drive vaccine hesitancy. These strategies focused on providing culturally responsive and community-relevant information about vaccines. Additionally, they built relationships and trust in the community by offering vaccine clinics in safe community spaces during off-work hours that were accessible and staffed by trained community members. These strategies also offered other supports that were community-specific. Table 4 describes behavioral science strategies to support vaccination uptake. Trust was built and vaccine uptake was increased via engagement with and participation of trusted community organizations and leaders including grassroots organizations, local hospitals, health units, community health care centres, as well as community faith leaders, members of the Black media, and members of the Black Physicians of Ontario (BPAO). This work was not easy, and their report notes “earning community trust and building vaccine confidence are marathon efforts.”
| Vaccination Uptake Barriers/Enablers | Principle | Behavioural Science Suggestions | Cases Study Example of Black Scientists’ Taskforce |
| Opportunity | |||
| Difficult to get time off for vaccination. Precarious essential work. Clinic location and hours. Booking systems difficult to navigate and complete correctly. | Principle 1: Make booking and attendance easier by maximizing the use of accessible and convenient locations, times, and days of the week. Support flexible work hours and paid time off to encourage uptake. | Building relationships and trust in the community by creating vaccination sites in safe community spaces during off-work hours that are accessible,16 staffed by trained individuals, and offer community-specific supports. Essential workers who are unable to work from home should also be targeted for workplace vaccination. Accommodate with scheduling that meets their needs. Municipalities should support walk-in vaccinations with simplified registration requirements. | Ensure vaccines are set aside specifically for members of high-risk Black and racialized communities, given past history of Black-serving clinics running out of vaccines and having to close ahead of schedule. |
| Technological, transportation, and mobility barriers. | Principle 2: One size most certainly does not fit all. Enable multiple operational strategies to reach individuals who are homebound or uncomfortable with technology. | Outreach is crucial for increasing vaccine uptake in certain groups. Offer transportation services to clinics for people facing barriers.17 Mobile vaccination clinics.18 Race-based data gathering is critical for understanding and addressing racialized pandemic disparities in meaningful ways. | The Task Force recommended door-to-door vaccine distribution to individuals in communities with significant technological, transportation, and mobility barriers.18 |
The Task Force organized online engagement sessions and collected pre- and post-survey data. Prior to the sessions, between 40% – 50% of participants self-identified as “vaccine hesitant.” Following the session, those who self-identified as “vaccine hesitant” decreased by approximately 25%.
This approach offers insights for other community-based efforts to increase vaccine uptake, and build confidence and trust. Engagement with local community leaders, partnerships with trusted individuals and organizations, and community-tailored strategies are important to support communities and groups with lower vaccine confidence to increase uptake. Each community will have unique barriers to vaccine confidence. Overcoming these barriers will require community-specific enablers and interventions.
Methods Used for This Science Brief
The data utilized in compiling this brief was collected by RIWI Corp., a third-party service provider. RIWI’s surveys deploy a random domain-intercept technology. For example, when a potential participant clicks on an inactive link or types in the address for a dormant website, instead of encountering a “page does not exist” notification or getting spammed by an advertisement, a RIWI survey is rendered full site on the page. Individuals decide whether they would like to participate in the research. No incentives for responding are offered. The survey can be accessed by all web-enabled devices, and due to the nature of the technology, the survey cannot be reached by someone who is not online.
RIWI groups respondents automatically by region, city, and sub-city area, and provides participants with a language- and context-appropriate survey. RIWI automatically collects and reports the time of access and geo-location data from all respondents; age, income, household, ethnicity, and other demographic data are all self-reported. Participants are assigned a unique identifier and no personally identifiable information is stored or reported. Continuous bot-filtering and anomaly detection are deployed to authentic human responses. IP addresses are translated into unique identifiers that RIWI utilizes to ensure that respondents have not previously completed the survey. Points of entry to the survey (i.e., lapsed Web domains) are rotated. RIWI methodology has been designed to reduce self-selection bias, social desirability bias, acquiescence bias, and online coverage bias.
Results are re-weighted (where stated) using 2016 Canadian census data to adjust for age and gender bias. Respondent weight values are generated post-stratification using a ranking algorithm. Survey participants comprised a randomized sample of internet users, and the sample was re-weighted to adjust for Statistics Canada age and gender population data. Respondents were from all regions in Ontario, with the majority from the province’s largest and most populous regions including Durham, Halton, Hamilton, Peel, Ottawa, Toronto, York, and Waterloo.
To identify strategies to enable and support vaccine uptake, we drew upon existing literature on strategies recommended and shown to be effective in increasing vaccination intention and uptake. This has included evidence syntheses produced by the Evidence Synthesis Network and Public Health Ontario, the WHO, and individual syntheses.19,20 The Behaviour Change Wheel was used to map the identified barriers/enablers to nine specific categories of intervention functions (i.e., change strategies) and seven policy categories (i.e., policy levers). This analysis has allowed us to suggest fit-for-purpose behavioural solutions supported by policy to address specific particular barriers and enablers to vaccination uptake in Ontarians.2
References
1. Government of Ontario. COVID-19 vaccinations data. COVID-19 (coronavirus) in Ontario. Published 2021.https://covid-19.ontario.ca/data
2. Michie S, van Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci IS. 2011;6:42. https://doi.org/10.1186/1748-5908-6-42
3. Crawshaw J, Konnyu K, Castillo G, et al. Factors affecting COVID-19 vaccination acceptance and uptake among the general public: A living behavioural science evidence synthesis (v5, Aug 31st, 2021).; 2021:75.https://www.mcmasterforum.org/docs/default-source/product-documents/living-evidence-syntheses/covid-19-living-evidence-synthesis-4.5—factors-affecting-covid-19-vaccination-acceptance-and-uptake-among-the-general-public.pdf?sfvrsn=33dc4261_5
4. IC/ES. COVID-19 Dashboard. Published April 6, 2021. Accessed April 7, 2021. https://www.ices.on.ca/DAS/AHRQ/COVID-19-Dashboard
5. Sundaram ME, Calzavara A, Mishra S, et al. Individual and social determinants of SARS-CoV-2 testing and positivity in Ontario, Canada: A population-wide study. CMAJ. Published online January 1, 2021. https://doi.org/10.1503/cmaj.202608
6. Crawshaw J, Konnyu K, Castillo G, van Allen Z, Grimshaw JM, Presseau J. Factors affecting COVID-19 vaccination acceptance and uptake among the general public: A living behavioural science evidence synthesis (v3, June 30th, 2021).; 2021:62. https://www.mcmasterforum.org/docs/default-source/product-documents/living-evidence-syntheses/covid-19-living-evidence-synthesis-4.3—factors-affecting-covid-19-vaccination-acceptance-and-uptake-among-the-general-public.pdf?sfvrsn=2954597f_5
7. Mishra S, Ma H, Moloney G, et al. Increasing concentration of COVID-19 by socioeconomic determinants and geography in Toronto, Canada: An observational study. medRxiv. Published online April 6, 2021:2021.04.01.21254585. https://doi.org/10.1101/2021.04.01.21254585
8. Chagla Z, Ma H, Sander B, Baral SD, Mishra S. Characterizing the disproportionate burden of SARS-CoV-2 variants of concern among essential workers in the Greater Toronto Area, Canada. Published online May 8, 2021:2021.03.22.21254127. https://doi.org/10.1101/2021.03.22.21254127
9. Iveniuk J, McKenzie K. Monitoring Progress: Race and Vaccine Equity.; 2021. https://www.wellesleyinstitute.com/publications/monitoring-progress-race-and-vaccine-equity/
10. Despite months of mixed messages, most Canadians who received an AstraZeneca vaccine have no regrets. Angus Reid Institute. Published May 17, 2021. https://angusreid.org/canada-astrazeneca-herd-immunity/
11. Government of Ontario. Ontario deploying last mile strategy to further increase vaccination rates. news.ontario.ca. Published August 24, 2021. https://news.ontario.ca/en/release/1000762/ontario-deploying-last-mile-strategy-to-further-increase-vaccination-rates
12. Presseau J, Arnason T, Buchan JL, et al. Strategies to support Ontarians’ capability, opportunity, and motivation for COVID-19 vaccination. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;2(36). https://doi.org/10.47326/ocsat.2021.02.36.1.0
13. The Black Scientists’ Taskforce on Vaccine. Toronto’s Black Community Town Halls Unpacked.; 2021. https://www.toronto.ca/legdocs/mmis/2021/hl/comm/communicationfile-132894.pdf
14. Mantzari E, Vogt F, Marteau TM. Financial incentives for increasing uptake of HPV vaccinations: A randomized controlled trial. Health Psychol. 2015;34(2):160-171. https://doi.org/10.1037/hea0000088
15. Wigham S, Ternent L, Bryant A, Robalino S, Sniehotta FF, Adams J. Parental financial incentives for increasing preschool vaccination uptake: Systematic review. Pediatrics. 2014;134(4):e1117-1128. https://doi.org/10.1542/peds.2014-1279
16. Research, Analysis, and Evaluation Branch. Evidence Synthesis Briefing Note: Strategies to encourage vaccine acceptance and address vaccine hesitancy. https://esnetwork.ca/briefings/strategies-to-encourage-vaccine-acceptance-and-address-vaccine-hesitancy/
17. Rotenberg S, Downer MB, Brown H, et al. COVID-19 vaccination for people with disabilities. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;2(35). https://doi.org/10.47326/ocsat.2021.02.35.1.0
18. Stall NM, Nakamachi Y, Chang M, et al. Mobile in-home COVID-19 vaccination of Ontario homebound older adults by neighbourhood risk. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;1(19). https://doi.org/10.47326/ocsat.2021.02.19.1.0
19. Brewer NT, Chapman GB, Rothman AJ, Leask J, Kempe A. Increasing vaccination: Putting psychological science into action. Psychol Sci Public Interest. 2018;18(3):149-207. https://doi.org/10.1177/1529100618760521
20. Lawes-Wickwar S, Ghio D, Tang MY, et al. A rapid systematic review of public responses to health messages encouraging vaccination against infectious diseases in a pandemic or epidemic. Vaccines. 2021;9(2). https://doi.org/10.3390/vaccines9020072
Document Information & Citation
Author Contributions: All authors contributed to the conception of the brief. KAB wrote the first draft of the brief. JT, KAB, SY, GL performed the analyses. All authors revised the Science Brief critically for important intellectual content and approved the final version.
Citation: Barrett KA, Feldman J, Trent J, et al. COVID-19 vaccine confidence in Ontario and strategies to support capability, opportunity, and motivation among at risk populations. Science Briefs of the Ontario COVID-19 Science Advisory Table.2021;2(47). https://doi.org/10.47326/ocsat.2021.02.47.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners can be found at https://covid19-sciencetable.ca/. The declarations of interest of external authors can be found under Additional Resources.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners.
