Key Message
Screen time has substantially increased for children and youth in Ontario and globally during the COVID-19 pandemic. Emergency measures introduced during the pandemic such as closures of schools and recreation contributed to increased screen time. There is a growing body of evidence associating increased screen time with harms to physical (e.g., decreased physical activity, eye strain and headaches), cognitive (e.g., attentiveness) and mental (e.g., reported symptoms of depression and anxiety) health in children and youth. There are evidence-based strategies to promote healthy screen habits for children and their families which offer an approach to encourage healthier screen use in the home setting and mitigate potential harms. However, the burden to reduce screen time cannot fall to parents and families alone. Policies are needed to avoid closures of schools and recreation, and ensure alternatives to screen time for children and youth of all ages that promote socialization and physical activity. In addition, there are key equity considerations when it comes to accessibility of alternatives to screen time such as child care and community recreation.
Summary
Background
Evidence from Ontario and globally has associated pandemic-related stay-at-home orders, closures of schools and recreation with increased screen time for children and youth. Screen time is considered any time spent with an electronic device, and can be active (e.g., video chatting, online learning) or passive (e.g., watching television). Recommendations from pediatric societies and other associations typically recommend limits to screen time to promote healthy development. This brief explores evidence associating screen time with physical, cognitive and mental health outcomes in children and youth, as well as evidence-informed strategies to encourage screen use within guidelines as well as healthy screen habits. Increased screen time in children and youth during the COVID-19 pandemic necessitates considerations of ways in which policies can promote screen use within guidelines and mitigate impacts to children and youth of public health emergency responses.
Questions
What factors mitigate or exacerbate the potential for negative effects of screen time on children and youth during the COVID-19 pandemic?
What evidence-informed strategies are useful for parents/caregivers to encourage screen use that falls within recommended guidelines for children and youth?
What policies can address screen time in children and youth?
Findings
Measures such as stay-at-home orders, closures of schools, and recreation facilities have likely driven increased screen time for children and youth. The reduction of in-person activities has necessitated the use of screens for education, socialization, cultural activities, and family gatherings. The impact of screen use on health outcomes in children and youth varies by age, gender and other factors.
Interpretation
There is growing evidence that associates pandemic-related closures and stay-at-home orders with increased screen time in children and youth. Evidence from research related to screen time interventions has emphasized strategies for individuals to decrease and limit screen use. The rise in screen time during the pandemic is concerning, and public health may have a role in promoting messages to parents and caregivers with concrete, practical ways to curb or limit children’s screen use. Individual-level interventions vary based upon the age of children or youth, and can include education and resources to support good screen hygiene for youth, parents and caregivers. Policy-level interventions are necessary to support parents, caregivers and children to reduce screen time. Equitable access to safe recreational opportunities for all children with a focus on children, families and communities that may lack access to resources such as high-quality child care or accessible recreation settings. These could include, for example, ensuring open access to in-person school and related extracurricular activities for children of all ages, developmental stages and abilities.
Full Text
Background
There is a growing body of evidence documenting that screen time has substantially increased for children and adolescents since the beginning of the COVID-19 pandemic.1 ‘Screen time’ refers to time spent with any screen, including smartphones, tablets, television, video games, computers or wearable technology.2 Depending on the intention of activity, depriving adolescents of active use (e.g., using social media to connect with peers) has been proposed to decrease wellbeing.3 Of note, there is evidence which suggests that cognitive and language abilities can be promoted through increased screen use, although such evidence is generally weak or requires further contextualization of these effects related to overall duration of use, specific activity engagement, and household characteristics.4 This level of engagement has been classified as active and passive screen use. Active screen use can include virtual reality fitness games, activities that encourage skill development and learning, and video chatting with friends and family. Passive screen time typically refers to activities that involve watching television, or other activities that prioritize receiving screen-based information without high levels of cognitive engagement (e.g., scrolling through social media apps). Both passive and active time spent using screens outside of online school-based requirements has increased for children and youth during the COVID-19 pandemic from 0.75 hours to as high as 6.5 hours per day in parent-report studies from the United States and elsewhere globally.1,5–9 A survey of children in Ontario found that non-online school-based screen time increased by over 3 hours per day in the pandemic compared to the pre-pandemic period.6
These data suggest that Ontario children are spending well above national public health recommendations on screens. The Canadian 24-hour Movement Guidelines, has recommended no more than 1 hour of screen time for children aged 4 years and under, and 2 hours of screen time for children and youth aged 5 to 17 years.10 A position statement from the Canadian Paediatric Society on screen time and young children does not recommend screen time for children under 2 years old, and recommends a limit of less than 1 hour per day for children 2 to 5 years old. For children and youth, recommendations relate to healthy screen behaviour, highlighting the pervasiveness of screens for education, recreation and socialization for children and youth.2,11
The first wave of the COVID-19 pandemic globally in spring 2020 was associated with sharp increases in screen time for children of all ages, including very young children to adolescents.12 This has been supported with data from Ontario, where a survey of parents gathered in June – August 2020 found that children’s screen time (e.g., watching television and playing video games) increased significantly, from 2.6 to 5.9 hours a day (p = 0.001) with the onset of the pandemic.6
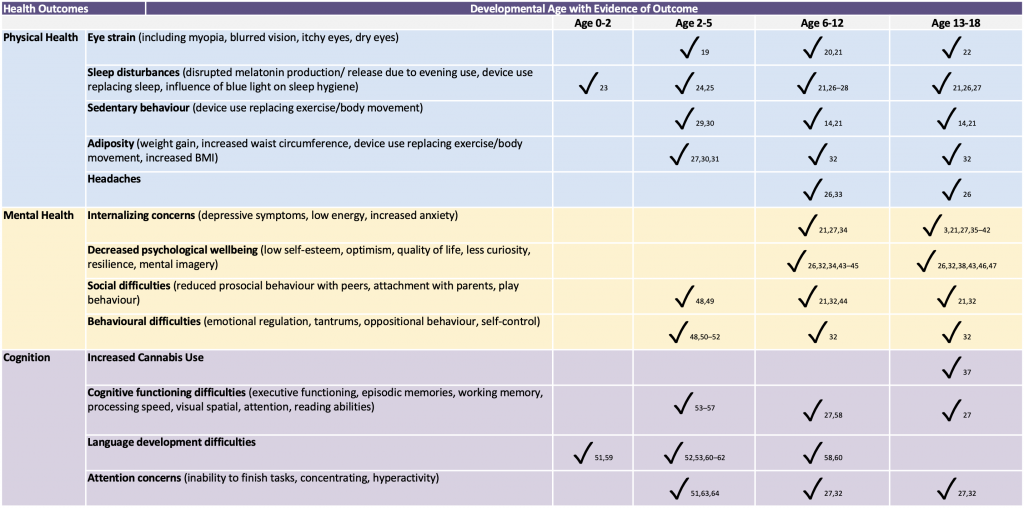
There have been changing family and community contexts throughout the COVID-19 pandemic. Some studies have associated an increase in screen time has been proportionate to family distress, related to childcare pressures, particularly among under-resourced families.1,6 Public health measures during the COVID-19 pandemic including school closures or reductions in hours of child care contributed to increased screen time for children and youth across all ages, irrespective of whether or not they were school-aged and learning online.12 The detrimental effects on physical, cognitive and mental health outcomes associated with increased screen time are well documented across a range of age categories and developmental stages (Table 1). Studies have indicated a dose-response relationship describing that for every additional hour of screen time above a 2-hour threshold of device use, there are increased likelihood of developing subsequent health concerns, including depression in adolescents,13,14 unhealthy weight gain,15 sleep disruption in preschool children16 and increased sedentary behaviours for children and youth,17 among other outcomes (Table 1). Although one limitation to the current review is that most literature has reported cross-sectional data, a recent review of 17 longitudinal studies with youth aged 10 to 24 years has found that many symptom measures are derived from parent or self-report data, however, the sheer number of moderating variables, distinctive differences among modes of technology, utility of screen time, and differences across age categories makes it difficult to compare results across populations.18 As such, further research is required to contextualize these differences. Future health policy and longitudinal randomized-controlled trials (RCTs) should assess screen use interventions with respect to developmental needs, context, and culture, particularly dose-response relationships among groups disproportionally affected by COVID-19 consequences.
Questions
What factors mitigate or exacerbate the potential for negative effects of screen time on children and youth during the COVID-19 pandemic?
What evidence-informed strategies are useful for parents/caregivers to encourage screen use that falls within recommended guidelines for children and youth?
What policies can address screen time in children and youth?
Findings
Pandemic-related public health measures have led to challenges that likely exacerbated screen use for children and adolescents.12 Specifically, these include mandated quarantine or physical isolation protocols, disruptions to childcare, and a switch to distance-based, online education. Stay-at-home orders have reduced or eliminated recreational activities for families, including sporting events, summer camps, play dates, birthday parties, and other non-screen related activities. At times, social distancing orders have generated additional screen time when events or activities were moved to a virtual environment. Further, the nature of these orders created a cascading series of events that have resulted in unintentional increased screen time for families. By reducing in-person activities, naturally occurring family routines related to activity preparation and travel time to event locations have been eliminated, providing more time at home, and thus, increased access to screens.
A cohort study of Ontario children found that adherence to public health measures in spring 2020 was associated with shorter outdoor time and longer total screen time.35 Outdoor time is recommended for children and youth as part of national movement guidelines.65 The association with outdoor time was stronger in younger children (ages <5 years), and the associations with total screen time were stronger in females and in older children (≥5 years).35 These findings have been related to lack in access to public facilities and in-person social activities, increased boredom, social isolation, and lack of routine while families are isolating. A study of family behaviours during mandatory COVID-19 stay-at-home orders in Portugal found that boys were more likely to engage in active screen time (Pombo et al., 2021),84 and overall, screen time had increased since the pandemic onset.
Disruptions in Child Care
Hartshorne and colleagues (2021)1 demonstrated that screen time significantly increased for children and youth within families who experienced disruptions in childcare due to COVID-19. Prior to COVID-19, research shows children predominately under parental supervision, rather than in formal child care services, engaging in greater amount of screen time and studies suggest that most parents report screens for babies and toddlers were useful distraction tools when needing to engage in other household tasks or self-care.17 For example, parents of children aged 0 to 4 who exceeded recommended screen guidelines, about two-thirds did not believe the screen time was excessive, and felt that such use had educational benefits, was an enjoyable activity, and enabled parents to complete other household tasks.66 Increased household demands concerns have been further exacerbated within particular socio-economic groups during the pandemic, as many families struggled to cope with loss of affordable childcare options within changing employment demands. To date, no studies have examined the potential effects of emergency childcare services on reducing screen time.
Screen Time and Mental Health Outcomes for Children and Youth
A longitudinal study of Ontario children from May 2020 to April 2021 examined different types of screen time (television, computer, video games, electronic learning) and mental health outcomes in over 2,000 children with multiple observations (6,648 observations). Electronic learning was associated with higher levels of depression and anxiety in a cohort of older children, mean age 11.3 years.67 In younger children (mean age 5.9 years [standard deviation (SD) 2.5]; 275 male participants (51.7%)), higher television or digital media time was associated with higher levels of conduct problems (age 2-4 years: β, 0.22 [95% confidence interval (CI), 0.10-0.35], p < .001; age 4 years: β, 0.07 [95% CI, 0.02-0.11], p = .007) and hyperactivity/inattention (β, 0.07 [95% CI, 0.006-0.14], p = .04). In older children and youth (mean age 11.3 years [SD 3.3]; 844 male participants (56.5%)), higher levels of television or digital media time were associated with higher levels of depression, anxiety, and inattention; higher levels of video game time were associated with higher levels of depression, irritability, inattention, and hyperactivity. These findings suggest that association between screen time and mental health outcomes during the pandemic were pervasive across type of screen use and type of mental health outcome. Policy interventions, as well as evidence-informed social supports, may be required to reduce mental health burden by addressing screen time in children and youth during the pandemic and beyond.
Demographic and Household Factors
Demographical differences among children and adolescents with higher screen time have been reported (Table 2), however, systematic reviews have reported inconsistent results across categories.68,69 Most studies that have examined these traits are cross-sectional in nature and therefore, robust relationships have been challenging to define. Available studies suggest that demographic differences can alter the relationships between screen use by children and language development, suggesting that a more nuanced understanding of the patterns of screen use among various populations is required.70 The interaction effects of age, gender, and reason for screen use also warrant further understanding. For example, a longitudinal study following youth from Grades 5 to 9 indicated that girls in Grade 9 had the highest screen use, however, this decreased in the next two years, whereas boys screen use, although lower, remained relatively stable across time. This study also found that reasons of use, including social networking, web use, passive use were all higher for girls, while video gaming screen time was higher for boys.71 Further, it appears that the detrimental effects of increased screen time are more likely to affect older children and adolescents than younger children, particularly after considering what the technology was used for.
There are a number of contextual and family-level factors associated with increased screen time including having more electronic devices in a child’s bedroom,72 decreased extracurricular activities,73 lack of an enforced and consistent bedtime,28 household disorganization,74 and a prior history of adverse childhood experiences.75,76 Parents with a higher self-reported ability to limit screen time were associated with an overall reduction in screen time.77 Similarly, lower parental stressors, less parents’ own use of screen time, and greater parental social support were also associated with decreased use and a greater parental restriction on child screen use.78 Of note, most studies of parental and child screen were conducted prior to the COVID-19 pandemic.
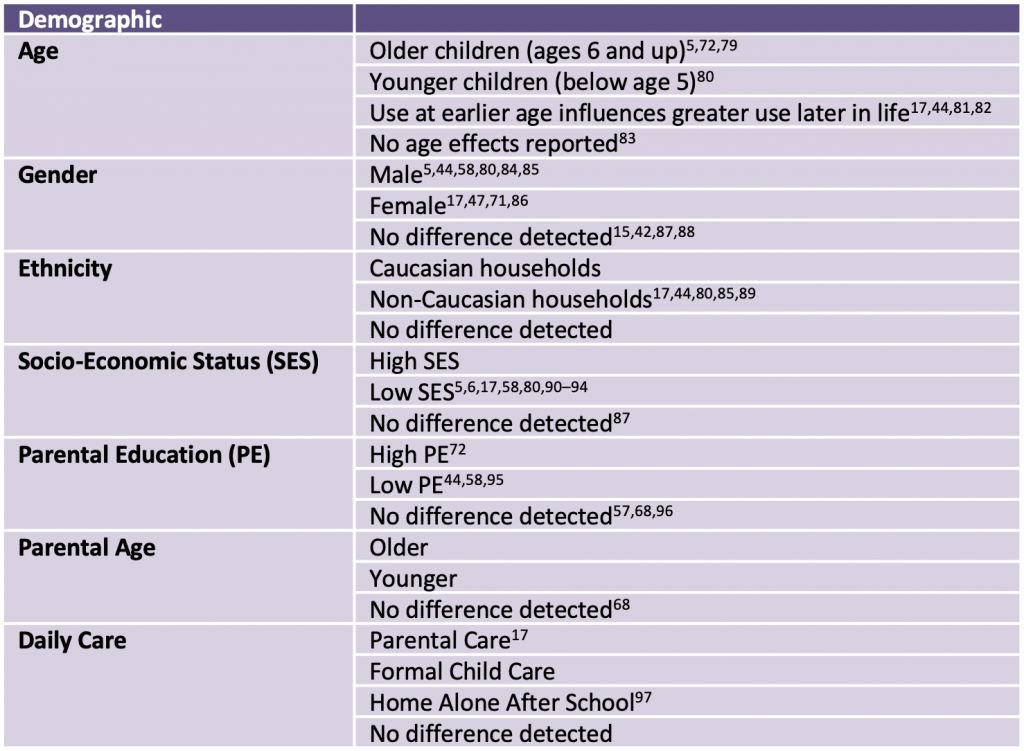
As this table provides a review of cross-sectional studies and systematic reviews that show differences among variables of interest, these data do not necessarily depict causal relationships.
Intent, Engagement, and Timing of Use
Research shows that the level of cognitive and physical engagement while using screens can modify level of risks associated with prolonged use.98 Depending on the circumstance, some electronic devices can be passive in some instances (e.g., playing a video game that is well known to the individual and therefore, not particularly stimulating) or active in others (e.g., learning particular skills to beat a difficult level in a video game), making it difficult to distinguish negative effects among types of electronic devices. In the context of the COVID-19 pandemic-related changes to recreational screen time habits, there has been a reported shift to more passive screen time, rather than active use.8
The distinction between intent of screen use can provide more information regarding potential consequences of these activities. For example, passive screen use, such as watching television, has been shown to be associated with a reduced ability for children to process verbal information. However, for children who spent a similar duration of time engaging in interactive use of electronic devices, this negative association was reduced.99 Passive use is also associated with increased anxiety and depressive disorders in adolescence.36These relationships require further understanding, as there are some very limited data which report that active screen use has been associated with positive educational outcomes,32 but also come with health consequences such as headaches in adolescents.100
To date, most literature dedicated to online teaching and learning activities in response to COVID-19 stay-at-home orders has focused on increased learning difficulties for children and youth. These studies all included concerns with increased screen time either expressed by the study authors or the parent-participants. More research is required to further understand these relationships between types of screen time and outcomes, included distinctions related to opportunities for peer socialization, active learning strategies, synchronous vs. asynchronous teaching, opportunities for individual teaching support, and influence of parental monitoring while providing school online.
Type of Technology Use
The nature of the screen use, whether it is active or passive, can influence the health outcomes of children and youth when they use technology more and in an unmonitored fashion. For example, playing video games is a relatively low-risk or benign activity for children and youth, particularly when the content of these games is developmentally appropriate and regularly supervised by parents. However, prolonged video game playing can be harmful for children when it interferes with academics, interpersonal relationships, physical/health behaviours, or occupational functioning. A study showed that 20% of Grade 7 and 8 students sampled reported engaging in excessive gaming during pandemic-related school closures, with 5% met researcher criteria for a behavioural gaming addiction. This was more commonly observed among male students, students who reported increased loneliness, and those with limited social or family support.100 Increased engagement in video games can reduce the likelihood of a young person engaging in more effective prosocial behaviours to reduce feelings of loneliness, depression, or social isolation affiliated with pandemic-related school shutdowns, such as engaging in physical activity or connecting with friends.101
There is also an increased likelihood that higher engagement on specific platforms can increase the secondary risk of additional mental health harms, such as increased risk of experiencing cyberbullying, online harassment or exploitation, unintentional collection of children’s personal data or breaches of privacy, or exposure to age inappropriate and unregulated content.102 The type of secondary risk outcomes can vary among type of technology used, age, and gender.103 For example, increased time spent on viewing social media was more strongly associated with depressive symptoms compared to television use.3
Evidence-Informed Strategies for Parents/Caregivers
“Screen hygiene”, considered to be the use of individual behavioural strategies to mitigate the detrimental effects of increased screen use, hadn’t been recommended in response to observed changes in screen time during the COVID-19 pandemic.104 To date, the evidence used to both conceptualize, measure, and inform screen-based recommendations within existing literature varies in quality, rigor, and clinical utility.105,106Systematic review and meta-analysis of interventions designed to reduce screen time in children and adolescents found that the majority of studies reported significant, although small, effect sizes.49,107,108Studies with the greatest effect sizes were those which set explicit goals for reduced use, monitored outcomes using objective measures, had methods to provide timely feedback to parents of ongoing efficacy and use, involved counselling services, and promoted high levels of parental monitoring.109 Another review found that interventions that were short-term (less than seven months in duration) and were supported with counselling or health promotion curricula had larger effect sizes.107 While, parents and families alone cannot be expected to address sharp increases in screen time, there are some strategies at the individual level which have been found to be effective at promoting healthy screen hygiene. Experts endorse a ‘harm reduction’ approach to screen time, which is an evidence-based, person-centred approach that seeks to reduce the health and social harms associated with a particular behaviour, without an expectation that individuals will fully abstain or stop the behaviour.110 Total elimination or rapid curbing of screen use is not realistic, given how pervasive screens are and in the context of the COVID-19 pandemic public health measures. Parents and caregivers may experience guilt and shame regarding screen use and their inability to curb children’s screen time to meet guidelines. Approaches from harm reduction can promote honest and realistic conversations with clinicians and educators about strategies to reduce screen time, as well as positive parent-child interactions and parenting approaches to encourage healthy screen habits and use.
Some commonly proposed strategies related to promoting healthy screen hygiene at an individual level include:
- Set and monitor consistent time limits on device use, by setting a schedule of use and sticking to it, a time that devices are turned off, or developing a family media plan. Time can be allotted individually for either educational or recreational device use. Developing daily device use routines can encourage children and adolescents to know what to expect regarding their devices.11,110–112
- Talk about the effects of screen use, particularly with older children and adolescents. Review age-appropriate information, such as articles or books, about the effects of screen time. For older adolescents, encourage them to reflect on their individual screen use, and work in collaboration to mutually develop a plan to set and monitor limits.
- Designate specific times during the day that are always screen-free, such as meal time, bedtimes, and during intentional family recreational or play time.110,111 Setting screen-free locations such as a child’s bedroom and meal table is also recommended.112 An RCT in preschool children that assessed an intervention with these strategies in preschool children had moderate effects on overall wellbeing.113
- Take frequent breaks from screen use. The 20-20-20 rule states that for every 20 minutes of screen use, one should remove focus from the screen, and for 20 seconds, visually focus on an object approximately 20 feet in the distance. This strategy has been recommended to reduce eyestrain by briefly relaxing the eyes.104,114 Post-test results of students who implemented this rule in conjunction with use of artificial tears showed increased ocular health.115
- Promote “active” screen use activities that emphasize learning, socialization with friends and family, creativity, or practicing skills, rather than screen use with no clear intent or purpose. Discourage multi-tasking or task switching between screen use and other tasks.11,110,112
- Incorporate movement throughout the day during extended periods of screen use. Encourage children and youth to stretch or move their bodies while engaging in screen time, and adjust their posture while engaging in electronic device use.110,111
- Encourage parents to model healthy screen hygiene by limiting their own personal use of devices and screen time at home.11,95,110,111
- Consider tapering screen use, particularly as children and adolescents adjust to post-COVID-19 expectations and experiences. Although replacing screen time with other activities will occur naturally for some children and families, for those carrying a heavier load for any number of reasons, this may require explicit support. Implementing the aforementioned strategies may be difficult for some families. If families are concerned about increased screen use impairing their children or adolescents’ abilities, they are advised to contact their local children’s mental health agency.
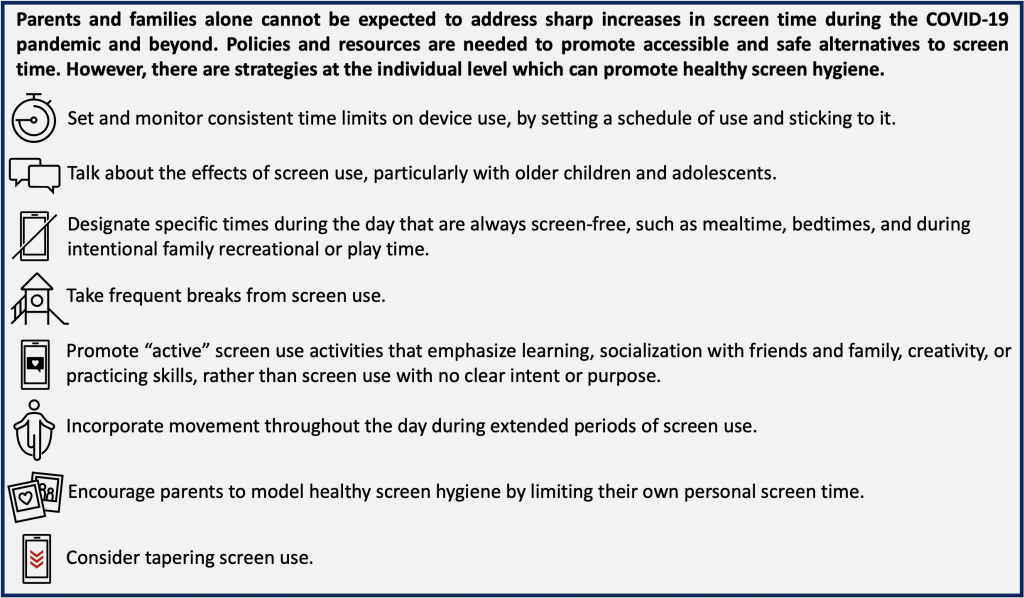
Figure presenting a summary of individual-level interventions targeted towards parents, caregivers, families, children and youth to promote healthy screen hygiene for children and youth.
Policies and Planning Considerations
From a public policy approach, there are approaches that can address some of the drivers of increased screen time for children of various ages, as well as support healthy behaviours and activities for children. For example, accessible and high-quality child care can mitigate screen time for younger children, both within the pandemic period and beyond. For example, the free, publicly-available, province-wide EarlyOn drop-in childcare center has been a model resource for childcare support. Alongside pandemic school closures centers shifted online. However, in other jurisdictions children were able to attend with pre-registration and this was eventually introduced in Ontario. Policies to prioritize and maintain continuity of programs which are safe spaces for children and families during the pandemic and beyond are needed. Child care options including affordable, short-term or emergency day care services may reduce child care concerns as well as increased use of screens. Increased screen time by children and youth and decreased physical activity were associated with pandemic-related closures of schools and other recreational activities and spaces. The harms and outcomes of these closures and unintended consequences of public health measures necessitate the development of robust emergency planning to avoid future closures and harms to children and youth.
Further, for school-aged children and youth, policies which advocate for in-person schooling and recreation are important. In-person schooling and recreational activities before, after or during school are healthy physical activity, and offer active and social alternatives to screens that promote healthy child and youth development. The use of screens for learning, socializing and play is increasingly inevitable for children, youth and adolescents. Investments in resources and training to be delivered in clinical and education settings whereby youth can be encouraged to reflect on screen use, as well as gain tools and strategies to safely and effectively navigate the online environment are needed.110
Interpretation
There is growing evidence suggesting that restrictions during the COVID-19 pandemic are associated with increased screen use in children and youth. Screen time increases are concerning given that prolonged use can affect physical, cognitive and mental health outcomes across multiple developmental stages. Evidence supporting screen use interventions in the context of COVID-19 public health measures such as school and child care closures are not available, however, evidence extrapolated from previous screen use interventions at the individual level has suggested that increased parental monitoring, implementing screen-free routines, and frequent breaks away from screens can mitigate overall effects on mental health. These, however, may not be feasible and practical for many. Equity considerations are key.
The harms of increased screen time in children and youth necessitate a broader policy response. Investments in child care, retaining in-person school, and extracurricular programs for children and youth can support families and caregivers of children of all ages and promote healthy development. Further, the association between increased screen time and closures of child care and schools demonstrates the importance of efforts to facilitate continuity and accessibility of child care and school during emergencies to avoid unintended harms to children and youth. Further, investments are needed to inform education and outreach to help youth and adolescents build screen hygiene and social media safety skills. Screen hygiene is adopted at the individual level, but supported by investments in public health, education and recreation services and programs that serve children, caregivers and families.
As parents and caregivers who perceive they have the capacity to regulate screens tend to do this more, further guidance of how to encourage parents, caregivers, clinicians, educators and decision-makers to do so is needed. There are many strategies at the individual level to limit device use, including password protecting apps, automating when devices turn off, or installing monitoring devices. Sharing these strategies through public health promotion campaigns can provide parents and caregivers with concrete, practical ways to implement the above recommendations and increase awareness overall around the need to limit screen use for children and youth, and promote activities that encourage physical activity and healthy development. Careful attention to equity considerations is important so that resources are appropriately accessible to those parents and caregivers in communities disparately affected by the pandemic. Finally, ensuring that systems are appropriately resourced (e.g., school and community) to mitigate and correct any disruptions in attaining developmental milestones (particularly for the preschool to primary-aged children) and mental health supports for adolescents in an equitable manner that is attentive to culture and context.
Methods Used for This Science Brief
A rapid review of PubMed, Google Scholar, the COVID-19 Rapid Evidence Reviews, the Joanna Briggs Institute’s COVID-19 Special Collection, LitCovid in PubMed, the Oxford COVID-19 Evidence Service, the World Health Organization’s Global Literature on Coronavirus Disease began on May 7, 2021 and was completed on May 27, 2021. Reports citing relevant articles and reference lists of identified articles were also reviewed during this time. Keywords used in this review were: “screen time and COVID-19”, however were tailored for each database. Specific literature describing screen time, COVID-19 in children and youth was identified manually by brief authors following these preliminary database searches.
References
1. Hartshorne JK, Huang YT, Lucio Paredes PM, Oppenheimer K, Robbins PT, Velasco MD. Screen time as an index of family distress. Curr Res Behav Sci. 2021;2. https://doi.org/10.1016/j.crbeha.2021.100023
2. Canadian Paediatric Society. Screen time and young children: Promoting health and development in a digital world. https://cps.ca/en/documents//position//screen-time-and-young-children/
3. Boers E, Afzali MH, Newton N, Conrod P. Association of screen time and depression in adolescence. JAMA Pediatr. 2019;173(9). https://doi.org/10.1001/jamapediatrics.2019.1759
4. Linebarger DL, Vaala SE. Screen media and language development in infants and toddlers: An ecological perspective. Dev Rev. 2010;30(2):176-202. https://doi.org/10.1016/j.dr.2010.03.006
5. Eyimaya AO, Irmak AY. Relationship between parenting practices and children’s screen time during the COVID-19 pandemic in Turkey. J Pediatr Nurs Nurs Care Child Fam. 2021;56. https://doi.org/10.1016/j.pedn.2020.10.002
6. Seguin D, Kuenzel E, Morton JB, Duerden EG. School’s out: Parenting stress and screen time use in school-age children during the COVID-19 pandemic. J Affect Disord Rep. 2021;6:100217. https://doi.org/10.1016/j.jadr.2021.100217
7. Tebar WR, Christofaro DGD, Diniz TA, et al. Increased screen time is associated with alcohol desire and sweetened foods consumption during the COVID-19 pandemic. Front Nutr. 2021;8. Accessed March 29, 2022. https://www.frontiersin.org/article/10.3389/fnut.2021.630586
8. Moore SA, Faulkner G, Rhodes RE, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: A national survey. Int J Behav Nutr Phys Act. 2020;17(1):85. https://doi.org/10.1186/s12966-020-00987-8
9. Xiang M, Zhang Z, Kuwahara K. Impact of COVID-19 pandemic on children and adolescents’ lifestyle behavior larger than expected. Prog Cardiovasc Dis. 2020;63(4):531-532. https://doi.org/10.1016/j.pcad.2020.04.013
10. Tremblay MS, Carson V, Chaput JP, et al. Canadian 24-hour movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016;41(6 (Suppl. 3)):S311-S327. https://doi.org/10.1139/apnm-2016-0151
11. Canadian Paediatric Society, Digital Health Task Force, Ottawa, Ontario. Digital media: Promoting healthy screen use in school-aged children and adolescents. Paediatr Child Health. 2019;24(6):402-408. https://doi.org/10.1093/pch/pxz095
12. Bergmann C, Dimitrova N, Alaslani K, et al. Young children’s screen time during the first COVID-19 lockdown in 12 countries. Sci Rep. 2022;12(1):2015. https://doi.org/10.1038/s41598-022-05840-5
13. Grøntved A, Singhammer J, Froberg K, et al. A prospective study of screen time in adolescence and depression symptoms in young adulthood. Prev Med. 2015;81:108-113. https://doi.org/10.1016/j.ypmed.2015.08.009
14. Liu M, Wu L, Yao S. Dose–response association of screen time-based sedentary behaviour in children and adolescents and depression: A meta-analysis of observational studies. Br J Sports Med. 2016;50(20):1252-1258. https://doi.org/10.1136/bjsports-2015-095084
15. Hume C, Timperio A, Veitch J, Salmon J, Crawford D, Ball K. Physical activity, sedentary behavior, and depressive symptoms among adolescents. J Phys Act Health. 2011;8(2):152-156. https://doi.org/10.1123/jpah.8.2.152
16. Zhu R, Fang H, Chen M, et al. Screen time and sleep disorder in preschool children: Identifying the safe threshold in a digital world. Public Health. 2020;186:204-210. https://doi.org/10.1016/j.puhe.2020.07.028
17. Carson V, Hunter S, Kuzik N, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: An update. Appl Physiol Nutr Metab. 2016;41(6 (Suppl. 3)):S240-S265. https://doi.org/10.1139/apnm-2015-0630
18. Tang S, Werner-Seidler A, Torok M, Mackinnon AJ, Christensen H. The relationship between screen time and mental health in young people: A systematic review of longitudinal studies. Clin Psychol Rev. 2021;86:102021. https://doi.org/10.1016/j.cpr.2021.102021
19. Yang GY, Huang LH, Schmid KL, et al. Associations between screen exposure in early life and myopia amongst Chinese preschoolers. Int J Environ Res Public Health. 2020;17(3):1056. https://doi.org/10.3390/ijerph17031056
20. Bao J, Drobe B, Wang Y, Chen K, Seow EJ, Lu F. Influence of near tasks on posture in myopic Chinese schoolchildren. Optom Vis Sci. 2015;92(8):908-915. https://doi.org/10.1097/OPX.0000000000000658
21. Lissak G. Adverse physiological and psychological effects of screen time on children and adolescents: Literature review and case study. Environ Res. 2018;164:149-157. https://doi.org/10.1016/j.envres.2018.01.015
22. Mylona I, Deres ES, Dere GDS, Tsinopoulos I, Glynatsis M. The impact of internet and videogaming addiction on adolescent vision: A review of the literature. Front Public Health. 2020;8. https://www.frontiersin.org/article/10.3389/fpubh.2020.00063
23. Chen B, van Dam RM, Tan CS, et al. Screen viewing behavior and sleep duration among children aged 2 and below. BMC Public Health. 2019;19(1):59. https://doi.org/10.1186/s12889-018-6385-6
24. Staples AD, Hoyniak C, McQuillan ME, Molfese V, Bates JE. Screen use before bedtime: Consequences for nighttime sleep in young children. Infant Behav Dev. 2021;62:101522. https://doi.org/10.1016/j.infbeh.2020.101522
25. Beyens I, Nathanson AI. Electronic media use and sleep among preschoolers: Evidence for time-shifted and less consolidated sleep. Health Commun. 2019;34(5):537-544. https://doi.org/10.1080/10410236.2017.1422102
26. Chetty-Mhlanga S, Fuhrimann S, Eeftens M, et al. Different aspects of electronic media use, symptoms and neurocognitive outcomes of children and adolescents in the rural Western Cape region of South Africa. Environ Res. 2020;184:109315. https://doi.org/10.1016/j.envres.2020.109315
27. Stiglic N, Viner RM. Effects of screentime on the health and well-being of children and adolescents: A systematic review of reviews. BMJ Open. 2019;9(1). https://doi.org/10.1136/bmjopen-2018-023191
28. Kato T, Yorifuji T, Yamakawa M, Inoue S. National data showed that delayed sleep in six-year-old children was associated with excessive use of electronic devices at 12 years. Acta Paediatr. 2018;107(8):1439-1448. https://doi.org/10.1111/apa.14255
29. Downing KL, Hinkley T, Salmon J, Hnatiuk JA, Hesketh KD. Do the correlates of screen time and sedentary time differ in preschool children? BMC Public Health. 2017;17(1):285. https://doi.org/10.1186/s12889-017-4195-x
30. LeBlanc AG, Spence JC, Carson V, et al. Systematic review of sedentary behaviour and health indicators in the early years (aged 0–4 years). Appl Physiol Nutr Metab. 2012;37(4):753-772. https://doi.org/10.1139/h2012-063
31. Biddle SJH, García Bengoechea E, Wiesner G. Sedentary behaviour and adiposity in youth: A systematic review of reviews and analysis of causality. Int J Behav Nutr Phys Act. 2017;14(1):43. https://doi.org/10.1186/s12966-017-0497-8
32. Sanders T, Parker PD, del Pozo-Cruz B, Noetel M, Lonsdale C. Type of screen time moderates effects on outcomes in 4013 children: Evidence from the longitudinal study of Australian children. Int J Behav Nutr Phys Act. 2019;16(1):117. https://doi.org/10.1186/s12966-019-0881-7
33. Çaksen H. Electronic screen exposure and headache in children. Ann Indian Acad Neurol. 2021;24(1):8. https://doi.org/10.4103/aian.AIAN_972_20
34. Zhang J, Liu MW, Yu HJ, et al. Associations of health-risk behaviors with mental health among Chinese children. Psychol Health Med. 2022;27(3):528-536. https://doi.org/10.1080/13548506.2020.1859559
35. Li X, Vanderloo LM, Maguire JL, et al. Public health preventive measures and child health behaviours during COVID-19: A cohort study. Can J Public Health Rev Can Santé Publique. 2021;112(5):831-842. https://doi.org/10.17269/s41997-021-00549-w
36. Kim S, Favotto L, Halladay J, Wang L, Boyle MH, Georgiades K. Differential associations between passive and active forms of screen time and adolescent mood and anxiety disorders. Soc Psychiatry Psychiatr Epidemiol. 2020;55(11):1469-1478. https://doi.org/10.1007/s00127-020-01833-9
37. Doggett A, Gohari MR, Godin KM, Ferro MA, Patte KA, Leatherdale ST. Cannabis use, screen time, and internalizing symptoms among Canadian youth: Testing mediation pathways. Subst Use Misuse. 2021;56(8):1232-1240. https://doi.org/10.1080/10826084.2021.1922455
38. Cooray MS. Screen time, sleep and social relationships: A population-level study examining emotional wellbeing during early adolescence. Univ Br Columbia. Published online 2020. https://doi.org/10.14288/1.0392376
39. Zink J, Belcher BR, Kechter A, Stone MD, Leventhal AM. Reciprocal associations between screen time and emotional disorder symptoms during adolescence. Prev Med Rep. 2019;13:281-288.https://doi.org/10.1016/j.pmedr.2019.01.014
40. Bickham DS, Hswen Y, Rich M. Media use and depression: Exposure, household rules, and symptoms among young adolescents in the USA. Int J Public Health. 2015;60(2):147-155. https://doi.org/10.1007/s00038-014-0647-6
41. Gunnell KE, Flament MF, Buchholz A, et al. Examining the bidirectional relationship between physical activity, screen time, and symptoms of anxiety and depression over time during adolescence. Prev Med. 2016;88:147-152. https://doi.org/10.1016/j.ypmed.2016.04.002
42. Riehm KE, Feder KA, Tormohlen KN, et al. Associations between time spent using social media and internalizing and externalizing problems among US youth. JAMA Psychiatry. 2019;76(12):1266-1273. https://doi.org/10.1001/jamapsychiatry.2019.2325
43. Twenge JM, Campbell WK. Associations between screen time and lower psychological well-being among children and adolescents: Evidence from a population-based study. Prev Med Rep. 2018;12:271-283. https://doi.org/10.1016/j.pmedr.2018.10.003
44. Przybylski AK, Weinstein N. Digital screen time limits and young children’s psychological well-being: Evidence from a population-based study. Child Dev. 2019;90(1):e56-e65. https://doi.org/10.1111/cdev.13007
45. Suggate SP, Martzog P. Screen-time influences children’s mental imagery performance. Dev Sci. 2020;23(6):e12978. https://doi.org/10.1111/desc.12978
46. Poulain T, Vogel M, Ludwig J, Grafe N, Körner A, Kiess W. Reciprocal longitudinal associations between adolescents’ media consumption and psychological health. Acad Pediatr. 2019;19(1):109-117. https://doi.org/10.1016/j.acap.2018.08.009
47. Viner RM, Gireesh A, Stiglic N, et al. Roles of cyberbullying, sleep, and physical activity in mediating the effects of social media use on mental health and wellbeing among young people in England: A secondary analysis of longitudinal data. Lancet Child Adolesc Health. 2019;3(10):685-696. https://doi.org/10.1016/S2352-4642(19)30186-5
48. Mistry KB, Minkovitz CS, Strobino DM, Borzekowski DLG. Children’s television exposure and behavioral and social outcomes at 5.5 years: Does timing of exposure matter? Pediatrics. 2007;120(4):762-769. https://doi.org/10.1542/peds.2006-3573
49. Schmidt ME, Pempek TA, Kirkorian HL, Lund AF, Anderson DR. The effects of background television on the toy play behavior of very young children. Child Dev. 2008;79(4):1137-1151. https://doi.org/10.1111/j.1467-8624.2008.01180.x
50. Lin HP, Chen KL, Chou W, et al. Prolonged touch screen device usage is associated with emotional and behavioral problems, but not language delay, in toddlers. Infant Behav Dev. 2020;58:101424. https://doi.org/10.1016/j.infbeh.2020.101424
51. Zimmerman FJ, Christakis DA, Meltzoff AN. Associations between media viewing and language development in children under age 2 years. J Pediatr. 2007;151(4):364-368. https://doi.org/10.1016/j.jpeds.2007.04.071
52. Tomopoulos S, Dreyer BP, Berkule S, Fierman AH, Brockmeyer C, Mendelsohn AL. Infant media exposure and toddler development. Arch Pediatr Adolesc Med. 2010;164(12):1105-1111. https://doi.org/10.1001/archpediatrics.2010.235
53. Hutton JS, Dudley J, Horowitz-Kraus T, DeWitt T, Holland SK. Associations between screen-based media use and brain white matter integrity in preschool-aged children. JAMA Pediatr. 2020;174(1):e193869. https://doi.org/10.1001/jamapediatrics.2019.3869
54. Pagani LS, Fitzpatrick C, Barnett TA, Dubow E. Prospective associations between early childhood television exposure and academic, psychosocial, and physical well-being by middle childhood. Arch Pediatr Adolesc Med. 2010;164(5):425-431. https://doi.org/10.1001/archpediatrics.2010.50
55. McArthur BA, Browne D, McDonald S, Tough S, Madigan S. Longitudinal associations between screen use and reading in preschool-aged children. Pediatrics. 2021;147(6):e2020011429. https://doi.org/10.1542/peds.2020-011429
56. McHarg G, Ribner AD, Devine RT, Hughes C. Screen time and executive function in toddlerhood: A longitudinal study. Front Psychol. 2020;11. https://www.frontiersin.org/article/10.3389/fpsyg.2020.570392
57. Zimmerman FJ, Christakis DA. Children’s television viewing and cognitive outcomes: A longitudinal analysis of national data. Arch Pediatr Adolesc Med. 2005;159(7):619-625. https://doi.org/10.1001/archpedi.159.7.619
58. Walsh JJ, Barnes JD, Tremblay MS, Chaput JP. Associations between duration and type of electronic screen use and cognition in US children. Comput Hum Behav. 2020;108:106312. https://doi.org/10.1016/j.chb.2020.106312
59. van den Heuvel M, Ma J, Borkhoff CM, et al. Mobile media device use is associated with expressive language delay in 18-month-old children. J Dev Behav Pediatr. 2019;40(2):99-104. https://doi.org/10.1097/DBP.0000000000000630
60. Madigan S, McArthur BA, Anhorn C, Eirich R, Christakis DA. Associations between screen use and child language skills: A systematic review and meta-analysis. JAMA Pediatr. 2020;174(7):665-675. https://doi.org/10.1001/jamapediatrics.2020.0327
61. Chonchaiya W, Pruksananonda C. Television viewing associates with delayed language development. Acta Paediatr. 2008;97(7):977-982. https://doi.org/10.1111/j.1651-2227.2008.00831.x
62. Christakis DA, Gilkerson J, Richards JA, et al. Audible television and decreased adult words, infant vocalizations, and conversational turns: A population-based study. Arch Pediatr Adolesc Med. 2009;163(6):554-558. https://doi.org/10.1001/archpediatrics.2009.61
63. Hill MM, Gangi D, Miller M, Rafi SM, Ozonoff S. Screen time in 36-month-olds at increased likelihood for ASD and ADHD. Infant Behav Dev. 2020;61:101484. https://doi.org/10.1016/j.infbeh.2020.101484
64. Foster EM, Watkins S. The value of reanalysis: TV viewing and attention problems. Child Dev. 2010;81(1):368-375. https://doi.org/10.1111/j.1467-8624.2009.01400.x
65. 24-Hour Movement Guidelines. Canadian 24-hour movement guidelines for the children and youth (5-17 years): An integration of physical activity, sedentary behaviour, and sleep. https://csepguidelines.ca/guidelines/children-youth/
66. Carson V, Tremblay MS, Spence JC, Timmons BW, Janssen I. The Canadian sedentary behaviour guidelines for the early years (zero to four years of age) and screen time among children from Kingston, Ontario. Paediatr Child Health. 2013;18(1):25-28. https://doi.org/10.1093/pch/18.1.25
67. Li X, Vanderloo LM, Keown-Stoneman CDG, et al. Screen use and mental health symptoms in canadian children and youth during the COVID-19 pandemic. JAMA Netw Open. 2021;4(12). https://doi.org/10.1001/jamanetworkopen.2021.40875
68. Paudel S, Jancey J, Subedi N, Leavy J. Correlates of mobile screen media use among children aged 0–8: A systematic review. BMJ Open. 2017;7(10):e014585. https://doi.org/10.1136/bmjopen-2016-014585
69. Duch H, Fisher EM, Ensari I, Harrington A. Screen time use in children under 3 years old: A systematic review of correlates. Int J Behav Nutr Phys Act. 2013;10(1):102. https://doi.org/10.1186/1479-5868-10-102
70. Blankson AN, O’Brien M, Leerkes EM, Calkins SD, Marcovitch S. Do hours spent viewing television at ages 3 and 4 predict vocabulary and executive functioning at age 5? Merrill-Palmer Q. 2015;61(2):264-289. https://doi.org/10.13110/merrpalmquar1982.61.2.0264
71. Rosenberg M, Houghton S, Hunter SC, et al. A latent growth curve model to estimate electronic screen use patterns amongst adolescents aged 10 to 17 years. BMC Public Health. 2018;18(1):332. https://doi.org/10.1186/s12889-018-5240-0
72. Aguilar-Farias N, Toledo-Vargas M, Miranda-Marquez S, et al. Sociodemographic predictors of changes in physical activity, screen time, and sleep among toddlers and preschoolers in chile during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(1):176. https://doi.org/10.3390/ijerph18010176
73. Campos L, Veríssimo L, Nobre B, Morais C, Dias P. Protective factors in the use of electronic media according to youth and their parents: An exploratory study. Int J Environ Res Public Health. 2021;18(7):3573. https://doi.org/10.3390/ijerph18073573
74. Emond JA, Tantum LK, Gilbert-Diamond D, Kim SJ, Lansigan RK, Neelon SB. Household chaos and screen media use among preschool-aged children: A cross-sectional study. BMC Public Health. 2018;18(1):1210. https://doi.org/10.1186/s12889-018-6113-2
75. Jackson DB, Testa A, Fox B. Adverse childhood experiences and digital media use among U.S. children. Am J Prev Med. 2021;60(4):462-470. https://doi.org/10.1016/j.amepre.2020.09.018
76. Cammack AL, Gazmararian JA, Suglia SF. History of child maltreatment and excessive dietary and screen time behaviors in young adults: Results from a nationally representative study. Prev Med. 2020;139:106176. https://doi.org/10.1016/j.ypmed.2020.106176
77. Guerrero MD, Vanderloo LM, Rhodes RE, Faulkner G, Moore SA, Tremblay MS. Canadian children’s and youth’s adherence to the 24-h movement guidelines during the COVID-19 pandemic: A decision tree analysis. J Sport Health Sci. 2020;9(4):313-321. https://doi.org/10.1016/j.jshs.2020.06.005
78. Lampard AM, Jurkowski JM, Davison KK. The family context of low-income parents who restrict child screen time. Child Obes. 2013;9(5):386-392. https://doi.org/10.1089/chi.2013.0043
79. Allen MS, Vella SA. Screen-based sedentary behaviour and psychosocial well-being in childhood: Cross-sectional and longitudinal associations. Ment Health Phys Act. 2015;9:41-47. https://doi.org/10.1016/j.mhpa.2015.10.002
80. Abdel Magid HS, Milliren CE, Pettee Gabriel K, Nagata JM. Disentangling individual, school, and neighborhood effects on screen time among adolescents and young adults in the United States. Prev Med. 2021;142:106357. https://doi.org/10.1016/j.ypmed.2020.106357
81. Hish AJ, Wood CT, Howard J, et al. Infants who watch television become toddlers who watch more television: Screen time patterns in the Greenlight Study. Pediatrics. 2020;146(1_MeetingAbstract):32-33. https://doi.org/10.1542/peds.146.1MA1.32b
82. Kvamsdal CA. Prevalence and Trends in Screen Time from 2014-2019, among Norwegian Adolescents. University of Agder; 2019. https://uia.brage.unit.no/uia-xmlui/bitstream/handle/11250/2681725/Christian%20Asbj%C3%B8rn%20Kvamsdal.pdf?sequence=1
83. Schaan CW, Cureau FV, Sbaraini M, Sparrenberger K, Kohl III HW, Schaan BD. Prevalence of excessive screen time and TV viewing among Brazilian adolescents: A systematic review and meta-analysis. J Pediatr (Rio J). 2019;95(2):155-165. https://doi.org/10.1016/j.jped.2018.04.011
84. Pombo A, Luz C, Rodrigues LP, Cordovil R. COVID-19 confinement in Portugal: Effects on the household routines of children under 13. Res Sq. Published online April 11, 2022. https://doi.org/10.21203/rs.3.rs-45764/v1
85. Fletcher EN, Whitaker RC, Marino AJ, Anderson SE. Screen time at home and school among low-income children attending head start. Child Indic Res. 2014;7(2):421-436. https://doi.org/10.1007/s12187-013-9212-8
86. Perrino T, Brincks A, Lee TK, Quintana K, Prado G. Screen-based sedentary behaviors and internalizing symptoms across time among U.S. Hispanic adolescents. J Adolesc. 2019;72(1):91-100. https://doi.org/10.1016/j.adolescence.2019.02.014
87. Boers E, Afzali MH, Conrod P. Temporal associations of screen time and anxiety symptoms among adolescents. Can J Psychiatry. 2020;65(3):206-208. https://doi.org/10.1177/0706743719885486
88. Costa BGG da, Salmon J, Santos PC dos, Minatto G, Silva KS. Clustering of screen time behaviours in adolescents and its association with waist circumference and cardiorespiratory fitness. J Sci Med Sport. 2020;23(5):487-492. https://doi.org/10.1016/j.jsams.2019.11.007
89. Foulds HJA, Rodgers CD, Duncan V, Ferguson LJ. A systematic review and meta-analysis of screen time behaviour among North American indigenous populations. Obes Rev. 2016;17(5):455-466. https://doi.org/10.1111/obr.12389
90. Arnup J, Black N, Johnston D. Children’s time use changes during periods of financial hardship. Published online April 23, 2020. https://doi.org/10.31234/osf.io/9fpmn
91. Fu K wa, Ho FKW, Rao N, et al. Parental restriction reduces the harmful effects of in-bedroom electronic devices. Arch Dis Child. 2017;102(12):1125-1131. https://doi.org/10.1136/archdischild-2017-312639
92. Tandon PS, Zhou C, Sallis JF, Cain KL, Frank LD, Saelens BE. Home environment relationships with children’s physical activity, sedentary time, and screen time by socioeconomic status. Int J Behav Nutr Phys Act. 2012;9(1):88. https://doi.org/10.1186/1479-5868-9-88
93. Krist L, Bürger C, Ströbele-Benschop N, et al. Association of individual and neighbourhood socioeconomic status with physical activity and screen time in seventh-grade boys and girls in Berlin, Germany: A cross-sectional study. BMJ Open. 2017;7(12):e017974. https://doi.org/10.1136/bmjopen-2017-017974
94. Leppänen MH, Sääksjärvi K, Vepsäläinen H, et al. Association of screen time with long-term stress and temperament in preschoolers: Results from the DAGIS study. Eur J Pediatr. 2020;179(11):1805-1812. https://doi.org/10.1007/s00431-020-03686-5
95. Gebremariam MK, Henjum S, Terragni L, Torheim LE. Correlates of screen time and mediators of differences by parental education among adolescents. BMC Pediatr. 2020;20(1):279. https://doi.org/10.1186/s12887-020-02181-y
96. Certain LK, Kahn RS. Prevalence, correlates, and trajectory of television viewing among infants and toddlers. Pediatrics. 2002;109(4):634-642. https://doi.org/10.1542/peds.109.4.634
97. Haycraft E, Sherar LB, Griffiths P, Biddle SJH, Pearson N. Screen-time during the after-school period: A contextual perspective. Prev Med Rep. 2020;19:101116. https://doi.org/10.1016/j.pmedr.2020.101116
98. Sweetser P, Johnson D, Ozdowska A, Wyeth P. Active versus passive screen time for young children. Australas J Early Child. 2012;37(4):94-98. https://doi.org/10.1177/183693911203700413
99. Veraksa N, Veraksa A, Gavrilova M, Bukhalenkova D, Oshchepkova E, Chursina A. Short- and long-term effects of passive and active screen time on young children’s phonological memory. Front Educ. 2021;6. https://www.frontiersin.org/article/10.3389/feduc.2021.600687
100. Alyoubi RA, Kobeisy SA, Souror HN, et al. Active screen time habits and headache features among adolescents and young adults in Saudi Arabia. Published 2020. https://ijpras.com/article/active-screen-time-habits-and-headache-features-among-adolescents-and-young-adults-in-saudi-arabia?html
101. Marciano L, Ostroumova M, Schulz PJ, Camerini AL. Digital media use and adolescents’ mental health during the COVID-19 pandemic: A systematic review and meta-analysis. Front Public Health. 2022;9. https://www.frontiersin.org/article/10.3389/fpubh.2021.793868
102. O’Keeffe GS, Clarke-Pearson K, Council on Communications and Media. The impact of social media on children, adolescents, and families. Pediatrics. 2011;127(4):800-804. https://doi.org/10.1542/peds.2011-0054
103. Kelly Y, Zilanawala A, Booker C, Sacker A. Social media use and adolescent mental health: Findings from the UK millennium cohort study. eClinicalMedicine. 2018;6:59-68. https://doi.org/10.1016/j.eclinm.2018.12.005
104. Singh S, Balhara YPS. “Screen-time” for children and adolescents in COVID-19 times: Need to have the contextually informed perspective. Indian J Psychiatry. 2021;63(2):192-195. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_646_20
105. Byrne R, Terranova CO, Trost SG. Measurement of screen time among young children aged 0–6 years: A systematic review. Obes Rev. 2021;22(8). https://doi.org/10.1111/obr.13260
106. K. Kaye L, Orben A, A. Ellis D, C. Hunter S, Houghton S. The conceptual and methodological mayhem of “screen time.” Int J Environ Res Public Health. 2020;17(10):3661. https://doi.org/10.3390/ijerph17103661
107. Wu L, Sun S, He Y, Jiang B. The effect of interventions targeting screen time reduction: A systematic review and meta-analysis. Medicine (Baltimore). 2016;95(27):e4029. https://doi.org/10.1097/MD.0000000000004029
108. Maniccia DM, Davison KK, Marshall SJ, Manganello JA, Dennison BA. A meta-analysis of interventions that target children’s screen time for reduction. Pediatrics. 2011;128(1):e193-e210. https://doi.org/10.1542/peds.2010-2353
109. Schmidt ME, Haines J, O’Brien A, et al. Systematic review of effective strategies for reducing screen time among young children. Obesity. 2012;20(7):1338-1354. https://doi.org/10.1038/oby.2011.348
110. Vanderloo LM, Carsley S, Aglipay M, Cost KT, Maguire J, Birken CS. Applying harm reduction principles to address screen time in young children amidst the COVID-19 pandemic. J Dev Behav Pediatr. 2020;41(5):335-336. https://doi.org/10.1097/DBP.0000000000000825
111. Wong CW, Tsai A, Jonas JB, et al. Digital screen time during the COVID-19 pandemic: Risk for a further myopia boom? Am J Ophthalmol. 2021;223:333-337. https://doi.org/10.1016/j.ajo.2020.07.034
112. Hale L, Kirschen GW, LeBourgeois MK, et al. Youth screen media habits and sleep: Sleep-friendly screen behavior recommendations for clinicians, educators, and parents. Child Adolesc Psychiatr Clin N Am. 2018;27(2):229-245. https://doi.org/10.1016/j.chc.2017.11.014
113. Yilmaz G, Demirli Caylan N, Karacan CD. An intervention to preschool children for reducing screen time: a randomized controlled trial. Child Care Health Dev. 2015;41(3):443-449. https://doi.org/10.1111/cch.12133
114. Loh K, Redd S. Understanding and preventing computer vision syndrome. Malays Fam Physician Off J Acad Fam Physicians Malays. 2008;3(3):128-130. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4170366/
115. Zulkarnain BS, Budiatin AS, Aryani T, Loebis R. The effect of 20-20-20 rule dissemination and artificial tears administration in high school students diagnosed with computer vision syndrome. J Pengabdi Kpd Masy Indones J Community Engagem. 2021;7(1):24-29. https://doi.org/10.22146/jpkm.54121
Document Information & Citation
Author Contributions: The Mental Health Working Group Members conceived the Science Brief. ET wrote the first draft of the Science Brief and performed the literature synthesis. CJM and KBB led revisions of the Science Brief. All authors revised the Science Brief critically for important intellectual content and approved the final version.
The authors would like to Charles Gardner, Christine Bushey and Stephanie Wolfe for their review of this Science Brief.
Citation: Toombs E, Mushquash CJ, Mah L, et al. Increased screen time for children and youth during the COVID-19 pandemic. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2022;3(59). https://doi.org/10.47326/ocsat.2022.03.59.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners can be found at https://covid19-sciencetable.ca/. The declarations of interest of external authors can be found under Additional Resources.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners.
