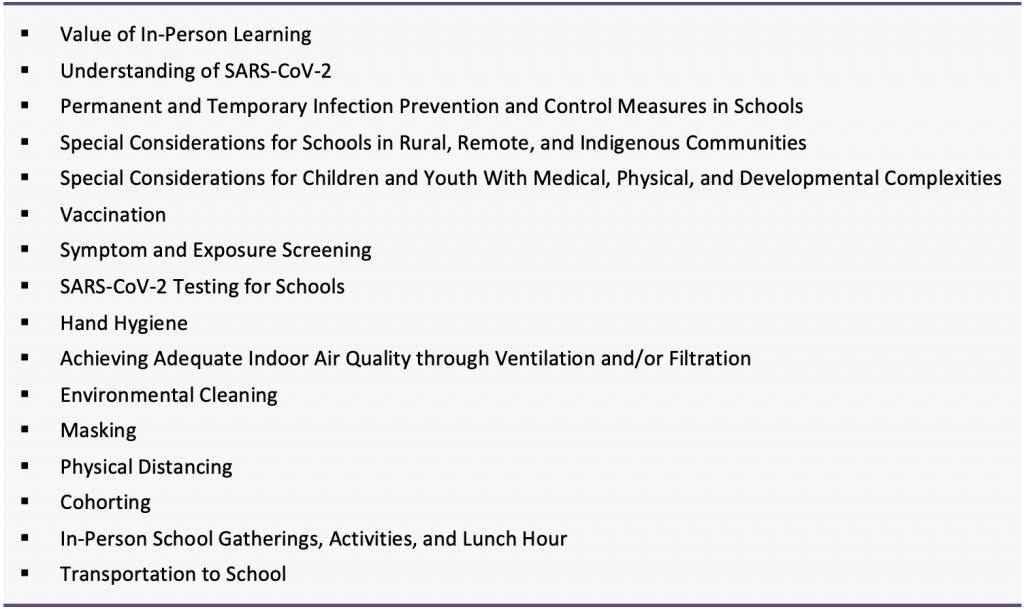
Key Message
In-person learning is essential for the learning and overall well-being of children and youth. Therefore, barring catastrophic circumstances, schools should remain open for in-person learning.
The level of community COVID-19 burden should inform the degree of school-based measures: the provided framework should be implemented at the regional level by public health units, considering local vaccination coverage rate and metrics of COVID-19 disease severity and to a lesser extent, SARS-CoV-2 transmission rate.
Permanent measures that support the ongoing operation of schools, irrespective of the COVID-19 pandemic, include vaccination of all eligible individuals, exclusion of sick students and staff, hand hygiene, adequate ventilation, and environmental cleaning.
Temporary measures (e.g., masking, physical distancing, cohorting) implemented in response to changes in COVID-19 disease burden should take into consideration student age, grade, and vaccination status.
Re-initiation and maintenance of extracurricular activities (e.g., music, sports, clubs) is an important component of return-to-school plans.
Summary
The physical, emotional, and developmental health of children and youth has been deeply impacted by the COVID-19 pandemic and restrictions placed on schools. School disruptions, including school closures and implementation of education models that have reduced direct interaction between children, their peers, and their teachers (e.g., online learning), have led to significant learning disruption, exacerbated educational inequities and deprived children of other supports and activities available through schools including food programs, physical activity and sports and clubs and teams.
It is therefore essential that moving forward the needs of students be prioritized to ensure sustained in-person school attendance and in-person learning. School closures, and the various distance learning strategies deployed to ensure educational continuity, should be part of a pandemic control strategy in only the most catastrophic of circumstances.
Given the high uptake of COVID-19 vaccines in Ontario, it is anticipated that SARS-CoV-2 transmission and severe disease requiring hospitalization will be substantially curtailed by September 2021; thus, the approach to school-based mitigation can be adjusted to reflect community risk. Emphasis should be placed on permanent measures that can aid in reducing infection transmission in general, including staying home when sick, achieving and maintaining adequate indoor air quality, environmental cleaning, and hand hygiene. Temporary mitigation measures, including active symptom-based screening, testing and contact tracing, use of non-medical or medical masks, physical distancing, and cohorting should be adjusted in accordance with COVID-19 disease burden.
With this in mind, we have defined three broad scenarios of COVID-19 disease burden: (1) low-risk, where severe disease requiring hospitalization is limited and sporadic; (2) moderate-risk, where there is early evidence of an upward trajectory in severe disease requiring hospitalization; and (3) high-risk, where there are high rates and continued upward trajectory of severe disease requiring hospitalization. SARS-CoV-2 transmission is an important secondary factor that can be considered in defining community risk, particularly early in the school year.
In the low-risk scenario, recommendations on temporary measures in the school environment include a strategy for contact tracing and low-barrier testing as an early warning system for emerging SARS-CoV-2 variants and increased transmission, a permissive approach to masking, and no requirement for physical distancing or cohorting.
In the moderate and high-risk scenarios, an increase in temporary measures would be warranted in schools, with emphasis on cohorting and age-dependent masking in kindergarten and elementary school students (without the need for physical distancing) and on masking with or without physical distancing (without the need for cohorting) in middle and high school students. It is recognized that individual jurisdictions in a low-risk scenario in September 2021 may choose more relaxed or more strict temporary measures depending on their local circumstances.
Background
The goal of this document is to provide guidance to policymakers on COVID-19 mitigation measures for kindergarten-to-grade 12 schools for September 2021. The document is anchored in the core principle that in-person learning is essential for children and youth and provides guidance on health and safety measures to support in-person education delivery and recovery strategies for September 2021 and beyond. It acknowledges that there is a range of risk tolerance both at the individual and community levels and provides a framework to adapt measures taking into consideration the community epidemiology, community readiness and information gained as the province and other jurisdictions re-open. While several jurisdictions are moving to focus on disease severity and health care system capacity as the predominant metrics for adjusting measures, we recognize that SARS-CoV-2 transmission is still of concern to many Ontarians. With this in mind, the framework considers moderate to severe disease resulting in hospital or ICU admissions as the primary metric used to determine the need to adjust mitigation measures but also considers transmission (effective reproduction number, Rt) an important secondary metric. It is anticipated that the importance of transmission as a metric will be reduced when re-opening of society is not associated with a substantial increase in SARS-CoV-2 related hospitalizations despite increasing case numbers, due to a high proportion of the population being fully vaccinated.
Several important domains related to education and children are not covered in detail in this document. A separate comprehensive guidance document covering the need for mental health awareness and support for all children is in development. Similarly, the importance of a strategy to manage the educational losses experienced thus far by some children is covered in a separate Science Brief.1 We do not address curricular reforms in this document. It must be recognized, however, that a period of (re-)adjustment for students and staff will be necessary at the beginning of the school year to: 1) address children’s mental health concerns and anxieties; 2) allow time for children to readjust to behavioural norms associated with in-class learning; and 3) support students who require school-based rehabilitation supports (e.g. physiotherapy, occupational therapy, speech and language therapy) and who may have fallen behind or regressed in their goals/abilities/health status. Children who may have fallen behind in their learning will need additional time and attention throughout the year.
This document was created by an interdisciplinary group of experts in pediatrics, infectious diseases, infection prevention and control, education, epidemiology, environmental and occupational health, indoor air quality, public health, school health, psychiatry and mental health, rural health, and Indigenous health. There was broad stakeholder engagement that included children’s hospitals in Ontario (The Hospital for Sick Children (SickKids), Children’s Hospital of Eastern Ontario (CHEO), McMaster Children’s Hospital, Kingston Health Sciences Centre, Holland Bloorview Kids Rehabilitation Hospital, London Health Sciences Centre, and Unity Health Toronto), education administration (school boards, principals), the school community (educators, parents, and students), and members of the Ontario COVID-19 Science Advisory Table.
Given that educators of elementary and secondary school students are best positioned to appreciate the operational and logistical considerations in adapting school and class routines to incorporate health and safety protocols, the following is not intended as an exhaustive school guidance document or implementation strategy. The ongoing safe operation of schools is the primary responsibility of the Ministry of Education and should include input from several key stakeholders, including the Chief Medical Officer of Health, Ministry of Health, Ministry of Labour, public health authorities, teachers and other educators, principals, other school-related authorities, parents, and children.
The recommendations in this document were drafted, reviewed, and approved by the authors. Evidence from the literature was routinely reviewed and used to form the basis of recommendations. However, several statements are made based on expert opinion with the rationale provided and evidence gaps highlighted. Recommendations may need to be adjusted as new evidence emerges.
Findings
Value of In-Person Learning
There is broad recognition that education is children’s ‘essential work’ and that schools are of critical importance to students’ learning and overall well-being. The Secretary-General of the United Nations described the impact of COVID-19-related school closures as a ‘generational catastrophe’.2 Ontario has had the longest interruption of face-to-face learning in Canada.1 In-person schooling is optimal for the vast majority of students because it enables access to a wide range of academic and social-emotional learning opportunities, promotes play, positive peer relationships, physical activity, and positive mental health. In-person schooling may contribute to other essentials, including nutrition, security, and health. Schools are also key sites to connect children and families with community, mental health, and developmental services. In addition, schools play a key role in enabling parents to work, particularly promoting labour participation of women and front-line service workers.3
Globally, school closures and transitions of entire classes or cohorts to remote learning led to the deployment of various distance learning strategies to enable educational continuity.4 Strategies in Ontario included synchronous or asynchronous classes taught online through a Learning Management System (LMS) or by using videoconferencing tools. In some cases, they were delivered through emails and print materials. Evidence from studies on school closures within Ontario, and in similar systems with shorter disruptions and with similar emergency virtual learning strategies indicate discernable learning losses.5, 6 However, negative effects have been more pronounced in communities and individuals most affected by COVID-19, and for those in pre-existing vulnerable circumstances.7 Comprehensive systems-level provincial data for Ontario are lacking. However, a simulation study with 157 countries predicted that, in high-income countries, generally assumed to be the best served, education continuity measures such as emergency remote digital learning would only mitigate between 15% to 60% of learning losses incurred.8 Furthermore, evidence from seven European countries with relatively well-resourced and broadly covered education systems found parental and child experiences of emergency home-schooling measures with distance virtual learning to be negative.9
There is increasing evidence that school closures and elimination of extracurricular activities for children have had substantial deleterious impact on their physical and mental health.10, 11 Parents report worsening mental health and ability to cope on the part of their children.12-14 High rates of anxiety and depression have been observed across children of all ages, with adverse psychological impacts, particularly among older children and adolescents compared to pre-pandemic periods.10, 15, 16 There has been a substantial increase in emergency department visits and hospitalizations for eating disorders.17 The loss of access to school-based healthcare services, special services for children with disabilities, and nutritional programs has profoundly affected the most vulnerable of children.18 Substantial disruptions to critical developmental milestones, including increase in speech delay, have been seen, and children have missed out on opportunities for skill development.19 Adverse general health effects, including increased sedentary behaviour and screen time, decreased physical activity, increased rates of child maltreatment, and delayed presentation with serious medical conditions, such as diabetic ketoacidosis, have also been noted.11, 20
It is therefore essential, that moving forward, the educational, physical, and mental needs of students be highly prioritized and protected to ensure sustained in-person school attendance and in-person learning. School closures, or transition to an online learning model, should not be used as a public health measure for pandemic control. Community-based public health measures (such as closure of non-essential workplaces, indoor capacity restrictions, use of non-medical or medical masks, testing, contact tracing, stay at home orders, travel restrictions) should be the preferred mechanisms for pandemic control. These restrictions should be employed for pandemic control in communities while schools continue to operate for in-person learning with appropriate mitigation measures in place, as outlined in this document.
School closures and transitions to remote learning should only be considered under a catastrophic scenario,21,22 based on the recommendation of the Chief Medical Officer of Health, when there is a clear signal of harm (morbidity and/or mortality) to children or the community at large that is directly attributable to children attending school for in-person learning despite the use of all available mitigation strategies, or when the harms associated with remote learning for students and their families are outweighed by identified health risks of in-person learning.
Current Understanding of SARS-CoV-2 as it Relates to Children and Education
SARS-CoV-2 is now widespread in almost all parts of the world, and its complete eradication is unlikely. Nevertheless, it is anticipated that the establishment of high levels of immunity in the general population through widespread immunization, and to a lesser extent, natural infection, will curtail infection rates and the adverse health impacts of SARS-CoV-2 on individuals and society to such an extent that full societal reopening is eventually feasible.23 Multiple factors will need to be taken into account on recommending the lifting of all pandemic-related restrictions in schools, including SARS-CoV-2 prevalence in the community, characteristics of the prevalent variants of concern (VOC; in particular immune/vaccine escape, but also transmissibility and disease severity), COVID-19 vaccine eligibility and uptake rates, and the degree to which vaccines protect against infection and severe disease.
It is expected that SARS-CoV-2 infections will continue to occur in the community as well as in schools. However, provided that the majority of infections continue to be associated with asymptomatic or mild disease in children and youth, and assuming that the broader community impact is manageable (i.e., no variant with vaccine escape leading to a substantial increase in hospitalizations/severe disease), the health and safety measures in schools can be adjusted to optimize the overall health, well-being, and learning for children and youth, while maintaining an in-person school model. It is essential in this context that there are mechanisms in place at local, regional and provincial levels to (1) promptly identify circulation of new VOCs associated with increasing transmission and/or disease severity; (2) monitor for any changes in the acute and chronic impacts of SARS-CoV-2 infection in children and youth; and (3) monitor the impacts of loosening restrictions in school and non-school settings on the risk of SARS-CoV-2 spread in the community, in households, and on the introduction and spread of SARS-CoV-2 in schools.
COVID-19 Disease in Children and Youth
The majority of children and youth who become infected with SARS-CoV-2 are either asymptomatic or have mild, self-limited symptoms such as cough, nasal congestion, runny nose, sore throat, fever, or gastrointestinal symptoms such as abdominal pain or diarrhea.24-28 Severe acute disease requiring intensive care has been described in a small minority of pediatric cases (0.06% of confirmed COVID-19 cases in children under 19 years of age in Canada),29 particularly among those with certain underlying medical conditions,30 but even in these patients the clinical course is usually much less severe than in adults, and deaths are extremely rare.31-35 In Canada, as of July 2, 2021, there have been 14 reported pediatric deaths out of 272,257 reported pediatric COVID-19 cases.29 The multisystem inflammatory syndrome in children (MIS-C) is an uncommon but serious post-infectious condition attributable to SARS-CoV-2 infection with an overall mortality of up to 2%, and responsive to immune modulating treatments.36-41 A recent population-based study in the US estimated the rate of MIS-C at 1 in 3,100 SARS-CoV-2 infections in persons younger than 21 years.42 At the present time there is no evidence in children to suggest that acute COVID-19 or MIS-C due to SARS-CoV-2 VOCs is more severe or frequent than that caused by non-VOC SARS-CoV-2.
While severe outcomes from acute COVID-19 in children are rare, it is important to monitor the frequency and severity of post-acute long-term sequelae of COVID-19 (long COVID) in children, and to follow its trends relative to other post-infectious syndromes (e.g., following gastroenteritis, infectious mononucleosis, and Lyme disease). In the UK, self-reported persistence of symptoms at 12 weeks after experiencing acute COVID-19 was 10% (95% Confidence Interval(CI): 5, 14) for children 2-11 years of age and 16% (95% CI: 12, 20) for children 12-16 years of age.43 In contrast, in a U.S. study involving 2,368 match-pairs of children, those with COVID-19 were no more likely to experience new diagnoses during the four-month follow-up period than children without COVID-19.44 Furthermore, a large cohort study of children in the United Kingdom found that only 1.8% of children had one or more residual symptoms (compared to 0.9% of SARS-CoV-2 negative controls) two months after their acute illness.45 Ongoing research into longer-term morbidities in children after SARS-CoV-2 infection is warranted, though findings so far are reassuring.46, 47
SARS-CoV-2 Epidemiologic Projections
Based on emerging data from other jurisdictions, the most reasonable assumption is that the Delta variant or other more transmissible variants will continue to be the dominant circulating strains of SARS-CoV-2 in Ontario over the coming months.48 Given the overdispersion of R0 originally described for SARS-CoV-2, most children with SARS-CoV-2 infection may transmit to relatively few people, while a minority of children with SARS-CoV-2 infection will transmit to larger numbers of people (super-spreader events). This means that mitigation measures in schools should aim to prevent super-spreader events.
SARS-CoV-2 Transmission
SARS-CoV-2 can be transmitted via aerosols (particles that remain suspended in the air for variable lengths of time) that are present at short ranges but may also contribute to long-range transmission;49 larger droplets that spread at short range; and direct contact with infected individuals or contaminated surfaces. This is similar to other respiratory viruses, where there is a spectrum of transmission, but certain modes predominate.50,51 In the case of SARS-CoV-2, current evidence suggests that it is transmitted most frequently and easily at short range through exposure to respiratory particles that range in size from smaller aerosols to larger droplets.52 Spread by suspended aerosols or droplets over longer ranges or time can occur particularly in crowded, enclosed spaces with poor ventilation. Spread by direct contact does not appear to be the predominant mode of transmission, although it remains plausible.53
Respiratory particles are produced from an infected person when they breathe, talk, cough, or sneeze. When a person has infection, whether or not transmission from that person occurs depends on multiple factors. Examples include how forcefully aerosols and droplets are expelled (e.g., singing or coughing are associated with higher risk), amount of virus present (e.g., more virus is present early in the infection), the duration of the exposure (i.e., longer contact with an infectious person is higher risk), environmental conditions (e.g., good ventilation and outdoors are associated with lower risk), and personal protective measures (e.g., physical distancing, wearing a well-fitted mask, and being fully vaccinated reduces the risk).54
Prevention of Transmission
While our understanding of how transmission occurs has evolved and the relative contribution of droplets and aerosols continues to be studied, several control measures are likely effective at reducing the risk of transmission irrespective of the relative contribution of larger droplets or aerosols to transmission. These include staying home when sick, wearing a well-fitted, non-medical or medical mask for source control and protection, practicing respiratory etiquette (coughing and sneezing into your arm), physical distancing, utilizing outdoor settings, and achieving and maintaining adequate indoor air quality through ventilation and/or filtration. Other important strategies that will reduce contact transmission include hand washing, cleaning frequently touched surfaces and avoiding touching the eyes, nose, and mouth.
Each of the control measures listed above likely provides some benefit in reducing SARS-CoV-2 spread. However, it is the combination and consistent application of these layered controls as a bundle that is most effective for reducing disease spread in schools. Immunization is the single most effective preventive intervention, and its widespread uptake will dramatically reduce infection rates even among unvaccinated children.23
COVID-19 Vaccine Uptake and Coverage Rates in Ontario
Early indications are that COVID-19 vaccine uptake among those eligible for a vaccine in Ontario is high. We can therefore expect that a substantial majority of persons 12 years of age and older will have received at least 1 dose, and likely 2 doses, prior to schools reopening in September 2021.55 With respect to children younger than 12 years of age, it is anticipated that a vaccine will not be approved and widely available prior to September 2021 and the timeline for eventual approval and roll-out remains uncertain. However, immunization of persons 12 years of age and older is anticipated to lead to lower SARS-CoV-2 community rates overall, leading to lower risk in schools.56 Outbreaks in schools remain a possibility among unvaccinated children, or if VOCs with vaccine escape become predominant.57
Transmission and Disease Rates as Measures of Pandemic Activity
There is considerable debate regarding the outcome measures that should be prioritized in determining the need for and extent of mitigation intervention for schools and the community at large. In the context of high vaccine uptake in individuals 12 years of age and older, metrics of severe disease (e.g., absolute COVID-19 hospital occupancy rates, rates per 100,000 population), or signals of vaccine escape are of primary importance. Measures of SARS-CoV-2 transmission (e.g., effective reproductive number, test positivity numbers, or test positivity rates) are expected to be less important when vaccine coverage is high but, in the near term, may be valuable for early detection of emerging variants less well covered by vaccines before a substantial increase in severe disease can be detected. In addition, robust measurement of transmission will allow for the detection of more infections, which would allow for better evaluation of adverse outcomes not reflected by hospitalization rates, such as long COVID.
Community Risk Framework
In each of the sections, we provide guidance based on level of community risk, categorized as low, moderate, and high (Table 1 and Figure 1). COVID-19-related metrics of disease severity (e.g., hospitalizations), and to a lesser extent SARS-CoV-2 transmissibility are key factors to consider in defining risk level, as they are anticipated to be influenced by vaccination rates and by the emergence of vaccine escape variants that cause disease in both unvaccinated and vaccinated individuals. Specific thresholds for vaccination rates, infection rates and disease rates have not been defined as these are somewhat arbitrary and because there may be differences in the weighting of individual criteria by jurisdiction, depending on their unique circumstances. However, in general terms, low-risk is applicable when there are limited and sporadic cases with severe disease requiring hospitalization, moderate-risk when there is early evidence of an upward trajectory in the number of cases with severe disease requiring hospitalization, and high-risk when there are high rates and continued upward trajectory of cases with severe disease requiring hospitalization. Measures of SARS-CoV-2 transmission is an important secondary factor that can be considered in defining community risk, particularly early in the school year.
Figure 1 illustrates the relationship of community transmission, as measured by the effective reproduction number (Rt), with disease severity, as measured by COVID-19-related hospital occupancy in absolute numbers and hospitalization rate per 100,000 population. A SARS-CoV-2 variant of concern that is more transmissible (e.g., Delta) would move the scenario up the y-axis (higher Rt) and the introduction of community mitigation measures to control community transmission would move the scenario back down the y-axis (by reducing Rt). Higher rates of severe disease would most often occur in the context of high community transmission (higher on the y axis and shifted to the right on the x-axis) but could potentially occur, even with lower community transmission rates in the case of an emerging variant with vaccine escape.
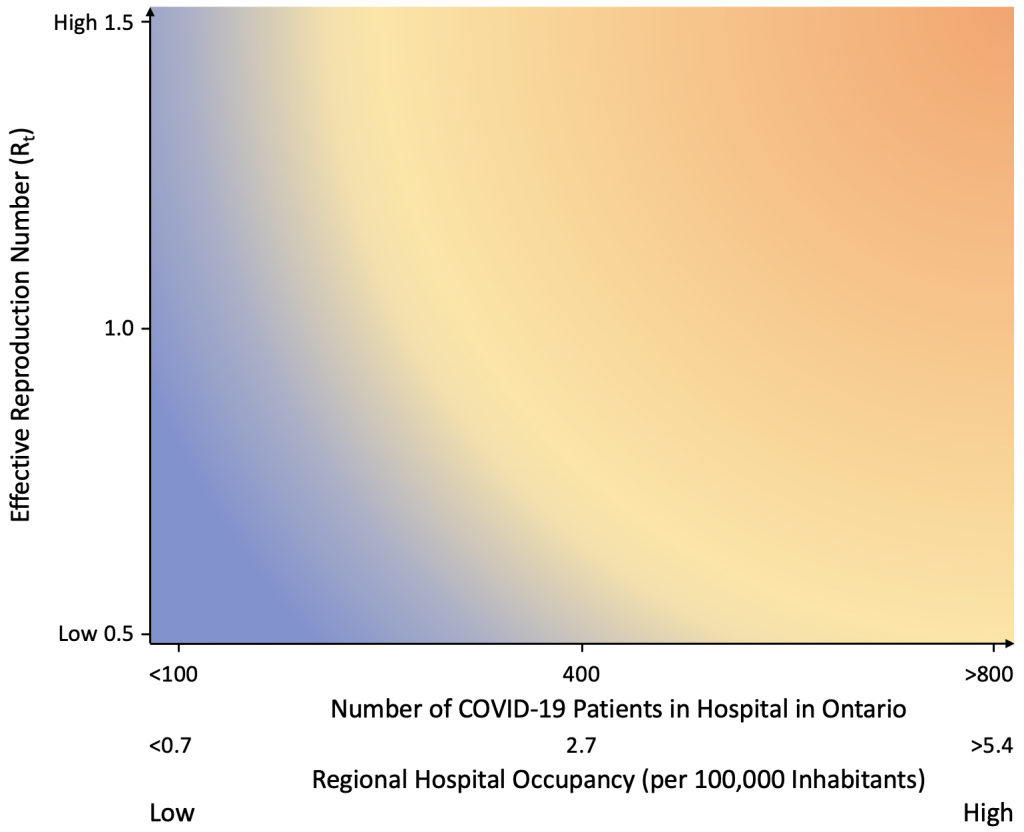
Rt: reproduction number 100K: 100,000
Permanent and Temporary Infection Prevention and Control (IPAC) Measures in Schools
As discussed, there is not one specific measure that will prevent transmissions from occurring in schools, but rather, there are several structural and individual elements that contribute to making schools healthier workplaces and reducing the risk of infection to in-person attendees. These are summarized within the Hierarchy of Hazard Controls (Figure 2).
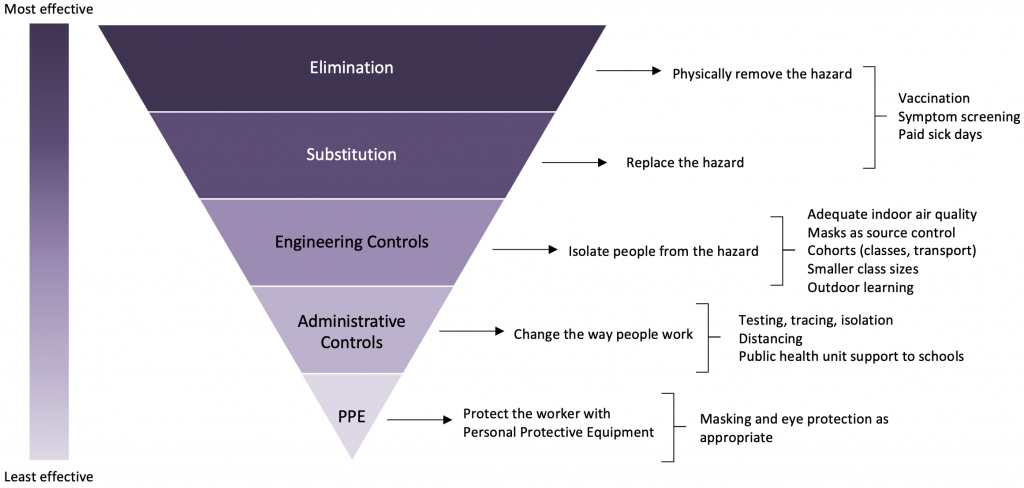
Figure adapted from CDC.58
Elimination measures are at the top of the hierarchy and are considered the most effective measures as they prevent infection from entering the school environment. With respect to SARS-CoV-2 and many other infectious diseases, these are primarily community-based and include measures such as vaccination, public health case and contact tracing, and symptom-based screening with exclusion from school if symptomatic or exposed and susceptible to SARS-CoV-2.
Within the school, permanent measures that help to reduce transmission of infectious diseases include:
- Vaccination of eligible students and those who interact with students (i.e., school staff, parents, caregivers)
- Exclusion of students and staff when they are symptomatic
- Hand hygiene
- Achieving and maintaining adequate indoor air quality via upgrade to school heating, ventilation, and air conditioning (HVAC) systems
- Appropriate environmental cleaning
Temporary measures that should be used during pandemic scenarios to reduce the risk of transmission of infectious disease in schools include:
- Symptom and exposure screening
- Diagnostic testing
- Use of non-medical or medical masks
- Physical distancing*
- Cohorting*
- Optimizing ventilation/filtration in classrooms, and increased use of outdoor space (when possible)
*Both physical distancing and small cohort sizes are facilitated by reduced class sizes.
With this in mind, the following sections of the document summarize the considerations for the safe, continued operation of schools based on the available evidence, as well as expert opinion. Where appropriate, recommendations have been provided for kindergarten, elementary school (Grades K-5), middle school (Grades 6-8), and high school (Grades 9-12) classes/students. For operational purposes, it is acknowledged that the approach in middle school may depend on whether the grades are associated with a kindergarten/elementary school (i.e., Grades K-8) or high school (i.e., Grades 7-12).
Implementation of the Framework
We recommend that this framework be interpreted at a regional level by public health units considering local vaccination coverage rate, metrics of disease severity, and, to a lesser extent, SARS-CoV-2 transmission rate. It is difficult to predict case numbers and health system occupancy related to COVID-19 as the province reopens and following the return to school in September 2021. Recent case trends in jurisdictions such as the UK, Israel, and the Netherlands demonstrate that outbreaks and increased numbers of hospitalizations have occurred among unvaccinated populations as the delta variant became predominant and restrictions were lifted.59 This experience highlights that a successful return to sustained in person learning and gradual relaxation of mitigation interventions in schools will require maintaining situational awareness with community responsiveness, and ultimately achieving high vaccine coverage among eligible persons throughout the province.
This framework is further predicated on the fact that children infected with SARS-CoV-2 generally have mild disease and that effective vaccines are available for those 12 years of age and older, meaning that even if there are occasional outbreaks in schools, they are not expected to be associated with severe disease among children, and that older children and adults should have excellent protection against severe disease as a result of vaccination. If a new VOC with vaccine escape emerges, and it is associated with increased transmission and significantly higher rates of severe illness among vaccinated populations, additional temporary mitigation measures as outlined in the moderate or high-risk scenarios of this framework should be adopted. Relaxation of temporary mitigation measures, such as masking, distancing, and cohorting should be considered when high vaccination rates are achieved and severe disease requiring hospitalization rates are low and stable. In these scenarios, permanent school-based health, and safety measures (symptom-based screening, hand hygiene, environmental cleaning, adequate ventilation) may be sufficient to limit spread from sporadic SARS-CoV-2 introductions into schools.
Table 1 provides a general approach to school-based health and safety measures in relation to low-, moderate-, and high-risk scenarios based on epidemiologic situations. In the context of high vaccine uptake, measures of disease severity are considered the most important metric for defining risk scenario, as they are expected to be strongly attenuated with high vaccine coverage. Measures of SARS-CoV-2 transmission may be of value for early detection of changes in patterns of disease transmission before a significant increase in severe disease can be detected.
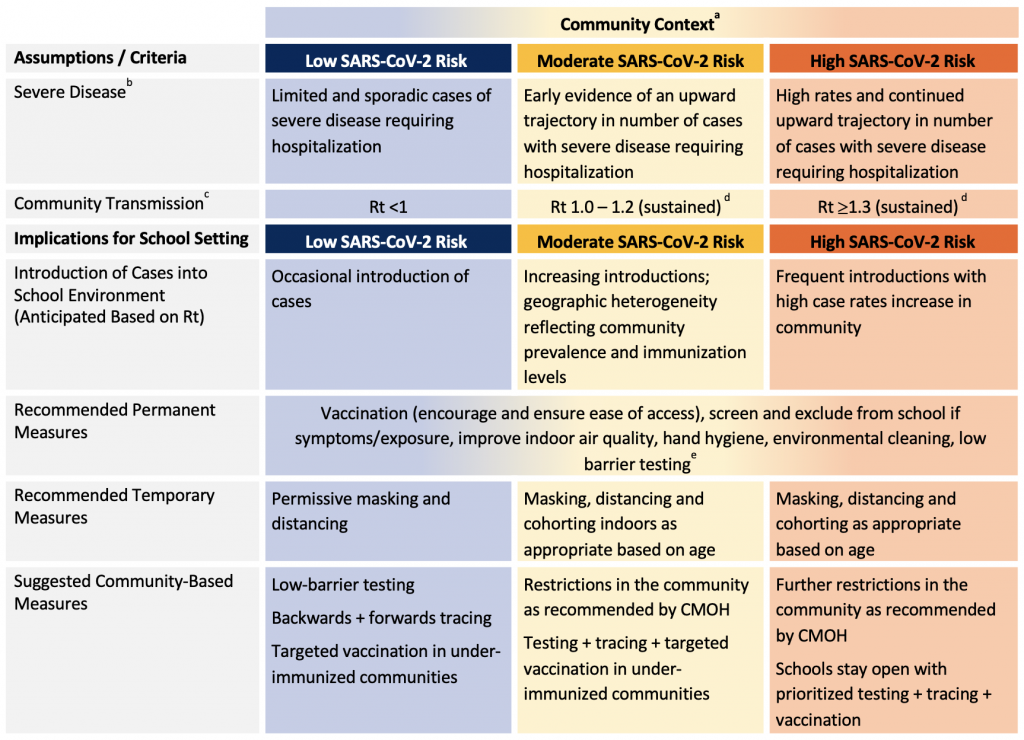
aIf in the low SARS-CoV-2 risk scenario based on metrics, some jurisdictions/schools may choose to maintain measures that can still afford layers of prevention that are less disruptive to the education and well-being (e.g., masking indoors) at the start of the September 2021 school year and reassess the ongoing need once in-person education has been resumed. bSevere disease can be assessed using the following metrics: COVID-19 hospitalizations, ICU admissions, and deaths. cPublic health tracing capacity is also an important consideration that may be impacted as case counts increase. dSustained SARS-CoV-2 transmission: 14 days or more. eRobust case and contact management with low-barrier testing (see Testing section) is important in all risk scenarios to identify and promptly isolate individuals with SARS-CoV-2 infection.
Special Considerations for Schools in Rural, Remote, and Indigenous Communities
For rural, remote, and Indigenous communities, the COVID-19 pandemic has presented additional distinctive and substantial challenges for education delivery which has expanded inequities. It is essential that there be special attention paid to how to appropriately support these communities such that health and education needs can be met moving forward. It must be acknowledged that each rural, remote and/or Indigenous community has unique strengths which contribute to their resiliency, and unique challenges; engagement with local community leadership is the critical first step in understanding the community needs, building relationships and tailoring public health strategies.60 Indigenous leaders and trusted professionals within the communities are well in tune with the strengths and challenges for families in the education system and can recommend the most appropriate strategies. It is important to take the lead from the Indigenous communities to determine strategies to support. The success of public health programs in preventing transmission of SARS-CoV-2 in such communities relies on close collaboration between public health units, local leadership and local health and social programs.
Important considerations for rural, remote, and Indigenous communities that need to be taken into account for all sections of this document:
- Ensure clear accountability for education support whether through federal or provincial resources.
- Transportation considerations will be different for children in rural, remote and First Nations communities because they may be in transit for prolonged time periods to and from school and school-based rehabilitation services.
- Limited access to clinical and support services have exacerbated the sense of isolation among children and youth, with educators concerned about students disconnecting from the virtual classroom.
- Remote learning is less accessible, due to technological challenges, in these communities.
- Social supports for the urban Indigenous population, which include off-reserve First Nations, Métis, and Inuit communities, have historically been connected with local Indigenous Friendship Centres and Aboriginal Health Access Centres, yet access to these types of services has been restricted during the pandemic.
- Restoring access to local friendship and health centres should be a priority to re-establish social connectivity among youth, families and elders, childcare and nutrition programs, and delivery of culturally sensitive health care and public health education from trusted leaders and healers.
- In communities with operational challenges around public health surveillance, it may be more prudent to consider additional, temporary measures up-front in the school year (please see sections titled Masking, Physical Distancing, Cohorting, Extra-Curricular Activities, and Transportation).
- Given the close-knit, multi-generational communities, it will be important that public health resources are available to strengthen testing and contact tracing, leveraging Indigenous contact tracers where applicable to ensure culturally safe care.
- Higher testing uptake will be seen with programs that are acceptable to children (e.g., oral-nasal or saliva sampling), accessible (e.g., pop-ups, flexible hours of operation, self-collection) and adoptable by the community (e.g., take-home testing kits with discreet drop-off locations and hours).
- Rapid molecular testing may be an additional consideration for communities with infection-related clusters if there are transportation-related challenges to accessing regional laboratories for molecular-based testing and results.
- Some rural and remote communities with smaller populations may more easily manage lower class sizes and physical distancing practices than those in densely populated urban areas.
- Ensure culturally appropriate messaging for Indigenous populations that takes into consideration historical factors contributing to vaccine hesitancy and medical mistrust. Include Elders and Knowledge Keepers in vaccine distribution and promotion plans.
- Aging infrastructure, including older HVAC and supplemental ventilation/filtration systems in many remote First Nations, Métis, and Inuit communities may impact the ability to properly ventilate schools and ensure adequate air quality, particularly during local outbreaks and in the colder months when opening windows is not an option.
- Schools in remote, rural, and First Nations, Métis, and Inuit communities that do not meet the appropriate minimum ventilation guidelines from ASHRAE Standard 62.1-2019 (see page 22), should be prioritized for upgrades.
- Overcrowded education infrastructure in some remote First Nations, Métis, and Inuit communities could make preventative measures such as cohorting and physical distancing difficult and could result in the need to shift to remote learning in some instances, further contributing to high rates of disengagement. Appropriate resources should be provided to ensure adequate space is available to support consistent in-person learning in these communities, and to ensure equitable access to digital learning resources.
- Where First Nations, Métis, and Inuit students must relocate to larger urban areas to attend a provincially operated secondary school, students should have access to adequate housing options which include sufficient space to allow for distancing and cohorting, if necessary, to ensure safe access to in-person learning.
Special Considerations for Children and Youth with Medical, Physical, and/or Developmental Complexities
Return to school must be inclusive of all children, including those with disabilities, developmental and behavioural challenges, and medical complexities. This includes children requiring intensive supports for activities of daily living and/or medical conditions, such as feeding, positioning, toileting or breathing supports, as well as those who depend on schools for therapies and other critical supports for their learning, development, and well-being. Many of the families of these children have had a prolonged period of time in home isolation compounded by a lack of respite and/or homecare supports. In particular, challenges for families and children/youth with neurodevelopmental disorders caused by cessation of school during the pandemic have been identified.61 Consultation with their parents and families to better understand their individual circumstances and needs is recommended. Virtual learning can be extremely challenging for many children and youth with complexities. Moreover, they rely on caregivers for optimizing their own health; high vaccine uptake among this vulnerable group, and those who are in contact with them, is important.35, 62
The additional resource requirements to facilitate safe return to school should not be a barrier to meaningful access to in-person education for any child. Detailed guidelines for specific groups of children and youth with complex needs have been developed by teams at SickKids,63 Holland Bloorview Kids Rehabilitation Hospital,64 and CHEO.65
Vaccination
Immunization is the single most effective preventive intervention and its widespread uptake will dramatically reduce infection rates even among unvaccinated people, including children.23 As such, it is essential that vaccines are easily accessible and encouraged for all approved age groups, and offered as a permanent community-based measure across all risk groups to improve regional vaccination coverage when local school or community outbreaks are occurring.
Under the Ontario Immunization of School Pupils Act (ISPA), all students attending primary or secondary school are required to provide proof of immunization against nine vaccine-preventable infectious diseases including diphtheria, tetanus, pertussis (whooping cough), poliomyelitis, measles, mumps, rubella, meningococcal disease, and varicella (chickenpox, for those born on/after 2010), or provide the required documentation for a medical or non-medical exemption to immunization.66
Recommendations for vaccination:
- Strongly encourage COVID-19 vaccination for all eligible individuals, including youth and those who interact regularly with children and youth, including (but not limited to) parents / caregivers, school staff, education workers, coaches, and tutors.
- Initiate robust vaccine campaigns to reduce barriers to access and improve vaccine confidence. Specific efforts should include support for families and communities in more severely impacted COVID-19 hotspot neighbourhoods.
- Ensure culturally appropriate messaging for Indigenous and other racialized populations, taking into consideration historical factors contributing to vaccine hesitancy and medical mistrust.
- Promote vaccine distribution plans that are focused on ease of access (i.e., on-site school-based vaccine clinics for students and their families), education and youth ambassador engagement to optimize vaccine coverage rates. These strategies should be promoted prior to the beginning of the school year and offered throughout the year to reach schools with low student vaccine coverage.
Vaccination status reporting considerations:
- We recommend that COVID-19 vaccination status for staff and students be reported to school authorities and public health at the start of the school year and updated regularly (e.g., mandated through the Reopening of Ontario Act or added to the ISPA), to help inform public health efforts.
- Schools and school boards should only have access to anonymized and aggregated information (i.e., proportion of eligible students with 1 or 2 doses of vaccine) to support targeted education / campaigns to improve accessibility and uptake in schools and regions with low vaccine rates.
- Access to individual level vaccination status should be available to public health officials, as it is essential to support timely contact management. This will help to reduce loss of in-person learning as appropriate (i.e., vaccination status can be considered during outbreak management and case and contact tracing).
- Careful attention to confidentiality and anonymity of this data is essential. Schools and school boards should only have access to aggregated data, and individual level data should only be available to public health officials for the purposes of outbreak management, and case and contact tracing.
- The Ministry of Education and the Office of the Chief Medical Officer of Health should explore options, including vaccination policies, to optimize vaccine coverage and reporting of vaccination status for staff and students.
Symptom and Exposure Screening, School Exclusions
In order to prevent the spread of SARS-CoV-2 infection within schools during the 2020/21 school year it was recommended that students, teachers, and other school employees who had signs or symptoms of COVID-19 (according to Ministry of Health and local public health guidance) stay home. Decisions about testing and return to school were to be guided by provincial and local public health authorities. These recommendations remain valid for the upcoming school year, since daily symptom screening has been associated with significant risk reduction of SARS-CoV-2 infection67(assuming school exclusion) and is an important strategy for the prevention of other infectious disease transmission within schools (i.e., influenza, respiratory syncytial virus, norovirus). A system whereby there is easy access to less invasive testing for school attendees (students and staff) and their household members will facilitate early detection of SARS-CoV-2 cases and monitor for the emergence of variants in schools (see Testing Section).
Recommendations for symptom and exposure screening:
- Screening and exclusion policies should be in place for students and employees who are symptomatic or have had an exposure to SARS-CoV-2 and directed to self-isolate by public health (policies may vary by vaccination status).
- If community transmission remains low after school returns and public health measures are lifted, the use of daily screening tools can eventually be eliminated, and a return to the practice of exclusion based on presence of infectious symptoms in general can be considered. Keeping staff and students at home when sick is an important health and safety measure that should be continued beyond the pandemic.
- The need for confirmation of screening, the location of screening (home vs. school) and the screening / exclusion criteria (i.e., number of symptoms, duration of symptoms, presence of symptomatic household members, recent exposure), should be adjusted based on the local SARS-CoV-2 risk scenario (Table 2).
- Confirmation of screening: This refers to a process whereby schools confirm that the screening has occurred at home. This attestation could be verbal, virtual, such as a smartphone app, web-based, QR-based or on paper for those unable to do so virtually, but the process should not be so onerous that it disadvantages groups with limited technological access or supports.
- Number of symptoms: Using any one symptom will be a more sensitive screening approach. However, this is less specific and will lead to more children being excluded from school (with associated learning impact). Availability of paid sick days is an important initiative to ensure that families can follow public health guidance on school exclusion and testing.68
- Selection of symptoms: The specific symptoms to screen for should take into consideration their positive predictive value as well as community rates of SARS-CoV-2 and other respiratory viruses. If COVID-19 risk scenario increases (i.e., high-risk scenario, suggesting a variant with vaccine escape), the threshold for school exclusion and testing should be lower (i.e., screen for any single symptom, even non-specific).69
- Duration of symptoms: Non-specific symptoms that are short-lived (< 24 hours) can be monitored in low- and moderate-risk scenarios and may not require immediate testing or prolonged isolation.
- SARS-CoV-2 exposure: The risk of infection following exposure is lower in fully vaccinated individuals. Vaccine status should be taken into consideration in post-exposure management. School screening tools should align with current public health case and contact management guidance (e.g., regarding fully vaccinated high-risk contacts of a case).
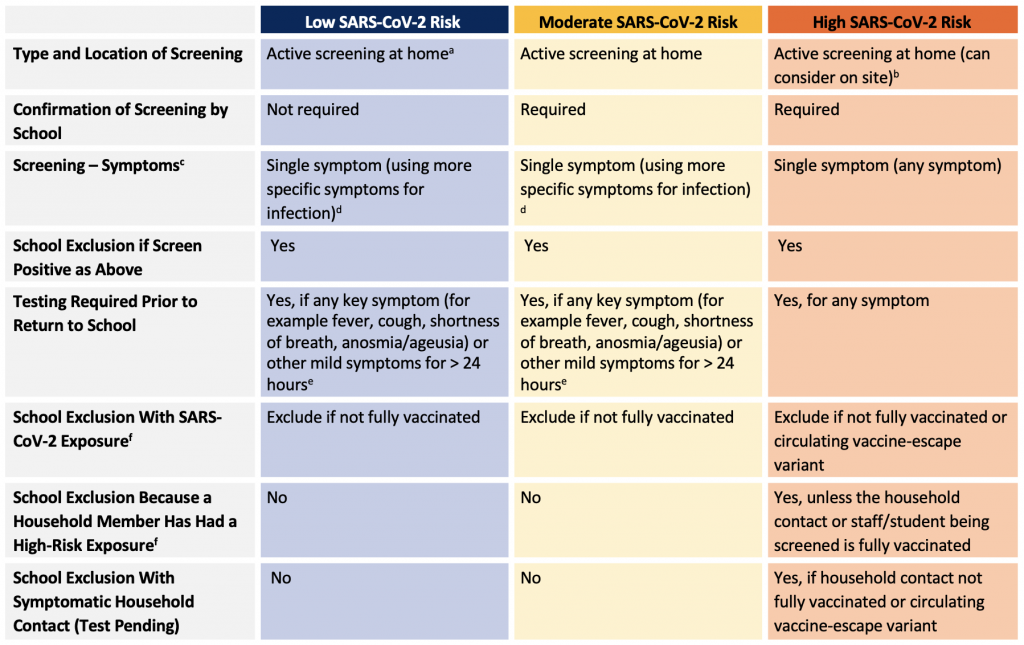
aThis should be reconsidered as restrictions are relaxed in the context of high vaccine coverage, low transmission rates and low hospitalizations rates. bOn site screening is associated with significant operational challenges and should only be introduced in discussion with schools and school boards taking into consideration feasibility. cThere is large variation in signs and symptoms of SARS-CoV-2 in children. Predominant symptoms have included fever and cough in more than half the cases, followed by rhinorrhea/nasal congestion, myalgia/fatigue and sore throat in 10%–20% of cases and gastrointestinal symptoms and headache in fewer than 10% of cases.70 dExamples of more specific symptoms for SARS-CoV-2 infection and other infectious diseases include fever, cough, shortness of breath, anosmia/ageusia, vomiting and diarrhea. eGuidance around key symptoms for testing are likely to evolve as information is gathered with new variants and in the context of other respiratory viruses. Refer to provincial guidance for final list of symptoms that require testing and recommendations for return to school if testing is not completed (i.e., by provincial case and contact management guidance). fRefer to provincial case and contact management for definitions of exposure and management.
SARS-CoV-2 Testing for Schools
The focus of testing should continue to be diagnostic testing for those with symptoms compatible with COVID-19 and those with a high-risk exposure to a case of COVID-19. It is essential that barriers to testing continue to be reduced for these groups to improve testing uptake, including easily accessible and acceptable testing options. This, along with testing in the community at-large, will facilitate early detection of SARS-CoV-2 cases and allow for close monitoring for the emergence of VOCs.
Asymptomatic screen testing (i.e., asymptomatic testing in the absence of documented exposure), is not routinely recommended, especially in the low to moderate COVID-19 risk scenarios.71,72 The use of asymptomatic screen testing as a temporary measure in the high COVID-19 risk scenario is an area that requires further study and should not be broadly implemented without further pilot data. There are substantial logistical and equity concerns that need to be taken into consideration (Table 3). If studied, consideration should be given to using the strategy to promote equity of access to participate in close contact clubs and sports (Test-to-Play strategy)73 and in situations where screening and/or adherence to public health measures may be more challenging (e.g., students with special needs), without exacerbating inequities based on race, ethnicity or wealth. A COVID-19 Science Advisory Table Science Brief on asymptomatic screen testing for schools is forthcoming.
Recommendations for SARS-CoV-2 testing for schools in symptomatic children and youth:
- Children with symptoms compatible with COVID-19 should undergo testing for SARS-CoV-2 (See Screening).
- Laboratory-based molecular tests are preferred as they are more sensitive than current point-of-care rapid molecular or antigen tests.
- Testing with a rapid molecular test may be considered if accessibility to laboratory testing is a barrier, for example in rural areas. In these situations, a lower sensitivity test with rapid turnaround is preferred over limited or significantly delayed test results.
- Testing with a rapid antigen test is not recommended.
- Laboratories should prioritize tests for rapid turnaround to minimize the time out of school for students should they test negative.
- The use of non-invasive specimen types (e.g., saliva, buccal-nares swab or throat-nares swab) should be strongly considered as this will likely increase cooperation among children and promote willingness for future testing among households.
- Testing should be made easily accessible to school students and staff to facilitate early case identification (e.g., take home testing kits, self-test with collection and drop off at school).
Recommendations for SARS-CoV-2 testing for schools in asymptomatic children and youth with a known exposure:
- Asymptomatic children who have had a high-risk exposure to an individual with SARS-CoV-2 infection should be tested for SARS-CoV-2.
- Consideration should be given to revising the definition of high-risk exposure in schools such that it minimizes education disruption without increasing in-school transmission.74
- Laboratory-based molecular testing is recommended for this population. The use of alternative specimens, particularly saliva or oral-nares swab, is acceptable and may increase compliance with testing recommendations and willingness for future testing.
- At this time, rapid antigen testing is not recommended based on the lower sensitivity of the test and inferior performance in asymptomatic individuals, particularly in communities in low- and moderate-risk. Rapid molecular testing may be useful in communities where there is limited access to laboratory-based testing (i.e., rural, remote, and Indigenous communities).
- The optimal timing of testing after an exposure is unclear. Testing immediately after case identification would determine if transmission has already occurred and identify infected secondary cases sooner, which may improve adherence with public health guidance and be more effective at interrupting chains of transmission.75 Testing later (≥ 5-7 days after the last close contact) is more likely to identify a student who has become infected after exposure to the known case. While testing at multiple time points post-exposure would identify both scenarios, this is likely not practical in schools and could have implications on regional testing capacity. Testing asymptomatic high-risk contacts at 5-7 days after exposure, would balance the need to catch secondary cases early with the optimal timing to detect cases post exposure.
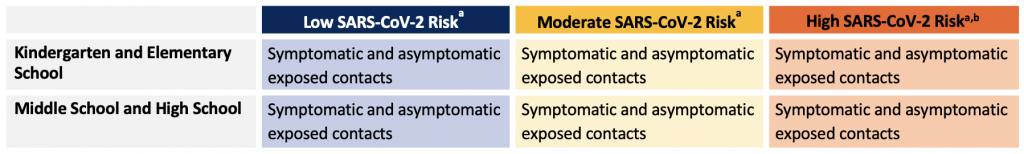
aTesting recommendations and requirements are likely to change over time in response to high levels of immunity in communities. bThe use of asymptomatic screening in the high-risk scenario is an area of further study and should not be broadly implemented without further pilot data. Logistical and equity considerations are essential prior to the implementation of asymptomatic screen testing.
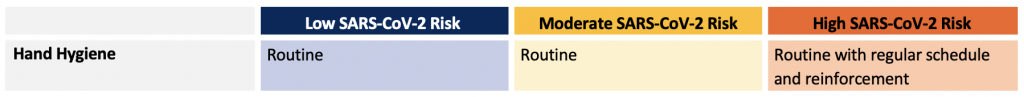
Hand Hygiene
SARS-CoV-2 and other respiratory viruses can be spread by respiratory droplet and contact transmission. As a result, and because virus shedding may occur prior to symptom onset or in the absence of symptoms, routine, frequent and proper hand hygiene (soap and water or hand sanitizer) is important in limiting transmission76 and should continue to be encouraged in schools. Routine hand hygiene is also beneficial for the prevention of many other childhood infections that have the potential to disrupt school attendance (e.g., gastrointestinal viral illnesses).
Recommendations for hand hygiene:
- Children and youth should be taught how to clean their hands properly (with developmentally and age-appropriate material)77 and taught to avoid touching their face, eyes, nose and mouth as much as possible. This should be done in a non-judgmental and positive manner and should be reinforced regularly.
- Respiratory etiquette: children and youth who have symptoms of a respiratory tract infection (not otherwise explained by underlying conditions, allergies) should stay home and should be reminded to sneeze or cough into a tissue followed by hand hygiene, or their elbow/sleeve if no tissue is available. In the event a mask is worn and becomes soiled, it should be changed.
- Students and staff should perform routine hand hygiene upon entering and before exiting the building, after using the washroom, before and after eating, and before and after playtime with shared equipment/toys.
- Access to hand hygiene facilities (hand sanitizer dispensers and sinks/soap) is recommended. Hand sanitizer (60-90% USP grade alcohol, not technical grade alcohol) should be available and easily accessible in all classrooms. Safety precautions to avoid toxic exposure (e.g., ingestion) from hand sanitizers should be in place.
- In settings of high community transmission, a regular schedule for hand hygiene, above and beyond what is usually recommended, is advised. Possible options include regularly-scheduled hand hygiene breaks based on a pre-specified schedule. For practical reasons and to avoid excess traffic in the hallways, the preferred strategy for these extra hand hygiene breaks would be alcohol-based hand rub unless sinks are readily available in the classroom.
Achieving and Maintaining Adequate Air Quality through Ventilation and Filtration
SARS-CoV-2 is primarily transmitted by aerosols and respiratory droplets during close unprotected contact, and it is recognized that aerosols play a role in longer range transmission of SARS-CoV-2, especially in poorly ventilated indoor areas.78-80 As such, it is expected that environmental conditions, exposure time and the air exchange rate in a space influence the transmissibility of SARS-CoV-2 and likely other respiratory viruses.81,82 Therefore, adequately ventilated classroom environments are important measures to reduce the likelihood of transmission.80, 83, 84
Similar to all other interventions within the hierarchy of control (Figure 1, 2), it is important to note that adequate ventilation alone will not eliminate the potential for SARS-CoV-2 transmission, especially related to close, unprotected contact. However, given the importance of indoor air quality for overall health and learning,85 achieving adequate ventilation in schools is an important investment to support improved health, academic performance and to assist in preventing the spread of several infectious diseases.
Recommendations for achieving and maintaining adequate air quality through ventilation and filtration:
- A systematic approach to identifying and prioritizing schools for ventilation upgrades should be undertaken. As a starting point, schools that do not meet the appropriate minimum ventilation guidelines from The American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) Standard 62.1-2019, should be prioritized for upgrades.86
- Invest in school heating, ventilation, and air conditioning (HVAC) system infrastructure and regular maintenance. This is of particular importance in schools where the system does not support good indoor air quality. HVAC systems can be optimized for a variety of objectives which may change in priority depending on the context, e.g., COVID-19 pandemic, extreme cold/heat events.
- During the pandemic, HVAC system function has been recommended to be optimized for respiratory particle removal (e.g., use of the highest rated Minimum Efficiency Reporting Value (MERV) filter that can be accommodated by the system, regular inspection of filters assembly, routine replacement of filters).84,87 In consultation with experts in physical plant design, air exchange rate and outdoor air intake can be increased. The limits of what is possible may be dictated by thermal comfort, humidity, and outdoor air quality.
- Consideration can be given to increasing ventilation/filtration above the minimum ASHRAE guidelines, where possible, where more respiratory aerosols are likely to be generated (e.g., music room, auditorium, cafeteria, gymnasium).
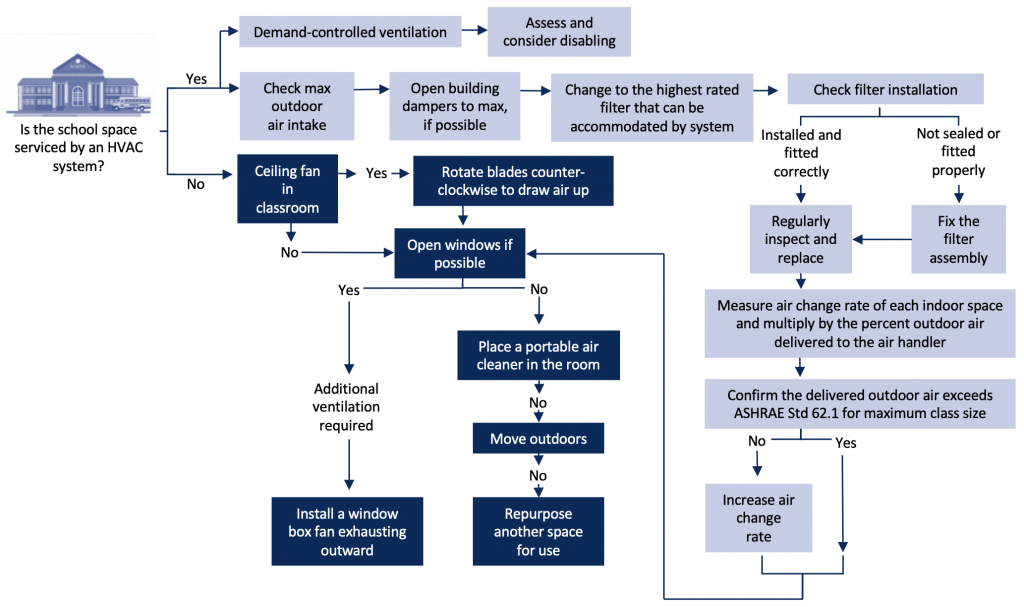
Adapted from Li et al. 2021.88
Additional strategies can be used to improve air quality while awaiting HVAC system upgrades (see engineering control flow diagram) including:
- The use of available outdoor learning environments when weather permits. It is acknowledged that some schools have limited usable space or limitations related to available spaces off property.67
- In naturally ventilated schools (i.e., no HVAC system), windows can be kept open, if safe, and according to weather conditions. Opening windows for short times at intermittent intervals can be of benefit.89 Box fans can be placed into windows to achieve supplemental ventilation; the fan should be oriented to exhaust outdoors.
- The use of portable air cleaners with high efficiency particulate air (HEPA) filter units in classrooms may be considered in spaces/classrooms with limited ability to achieve adequate ventilation (i.e., unable to open windows, no/insufficient HVAC ventilation), taking into consideration the transmission risk (e.g., age, classroom activities, community epidemiology).90-92
- Commercially available air cleaners with HEPA filter units can provide supplemental filtration in an indoor space.89, 93 Portable air cleaners can also be constructed by attaching a MERV13 (or other high efficiency) filter to a box fan. These devices can achieve similar ventilation/filtration efficiency as commercial units.
- The position of portable air cleaners in a classroom or other indoor school space should take into consideration the likelihood that aerosols/droplets are being captured by the intake and that the exhaust is not directed to occupants. Placement near the center of the room or near potential sources of SARS-CoV-2 droplets/aerosols (i.e., choir, playing of wind and brass instruments, lunch tables) is helpful.94, 95
- For commercially available units, manufacturer’s instructions on maintenance should be followed.87
- Portable air cleaners should be sized for the space; larger spaces with higher occupancy may require multiple units.
- Operation of a fan in the air cleaner unit will generate noise (~40-70 decibels). The noise rating of a device should be considered prior to use.
- Commercially available ionizing air cleaners and other unproven technologies should be avoided. Despite marketing claims, the efficacy of many of these devices is low and many can generate chemical byproducts.96
- Any supplemental ventilation/filtration strategy should be purchased and used in consultation with individuals with expertise.
Monitoring ventilation:
- It is important that HVAC and supplemental ventilation/filtration systems are regularly maintained and that measures are checked with the goal of optimization (e.g., air exchange rates, outdoor air intake, temperature, humidity).
- Carbon dioxide (CO2) levels can serve as a proxy measure for overall ventilation, but the CO2 level does not necessarily correlate with SARS-CoV-2 transmission risk. While CO2 monitoring has been suggested to be helpful when done properly, it requires expertise and communication and should not detract from ventilation upgrades.
Environmental Cleaning
SARS-CoV-2 has been detected on a variety or surfaces97 and survival depends on the surface material. It is possible that infection can be transmitted via fomites by touching contaminated surfaces and then touching mucous membranes (i.e. mouth, nose, eyes).52 The understanding of the role of fomites in SARS-CoV-2 transmission has evolved since the first wave, and they are no longer thought to be a primary mode of transmission.52,98 However, they may contribute highly to transmission of other respiratory and gastrointestinal pathogens.99 Therefore, environmental cleaning is an important permanent measure.
Recommendations for environmental cleaning:
- There should be a regular cleaning schedule (at least once a day), using Health Canada- approved disinfectants ensuring directions are followed (e.g., contact time is observed) with an emphasis on high-touch surfaces. Washrooms should be cleaned at least twice daily. There are many Health Canada approved non-quaternary ammonium-based disinfectants approved for use against COVID-19.100
- Efforts should be made to reduce the need to touch objects/doors (no-touch waste containers, prop doors open).
- Recommendations and any policies to ensure there is “no sharing” of food, water bottles or cutlery should continue.
- Regular cleaning of shared equipment (e.g., toys for imaginative play, manipulatives for math, lab materials, equipment for physical education) between students is operationally challenging and the risk associated with transmission is low. Instead, the focus should be on regular hand hygiene to reduce the risk of infection related to shared equipment.
- Similarly, there is no need to quarantine paper products (e.g., books, schoolwork, tests) as they are unlikely to be a significant source of transmission and these practices may contribute to reduced access to learning resources. Hand hygiene should be prioritized over quarantining.
Masking
The use of non-medical masks (NMMs) and medical masks for source control is one of several public health measures that has been effective at reducing SARS-CoV-2 transmission in the community.101, 102 When worn correctly, NMMs and medical masks reduce respiratory droplets and aerosols generated by the wearer from entering the environment.103Medical masks and well-fitting NMMs also provide protection for the wearer by preventing virus from coming into contact with the nose and mouth.104 While there are limited studies directly evaluating the effectiveness of NMM use in children, there are several ecological studies evaluating SARS-CoV-2 incidence in schools that have found that mask mandates have been associated with lower incidence of SARS-CoV-2 infections.83, 105-107 However, in the setting of low community transmission, the absence of masks in elementary school was associated with minimal transmission, despite regular class sizes.108
Potential negative consequences related to masking include impact on communication, impaired facial recognition, or identification, altered interactions (i.e., decreased emotional signaling / visual connection) and physical side effects (e.g., discomfort, irritation).109-111
Decisions around NMM use in schools should take into consideration the benefit from source control (which may vary by age) balanced with the negative consequences of NMM use. Other factors to consider include availability of other risk mitigation strategies (e.g., adequate ventilation, physical distancing), local epidemiology and community public health directives around masking in indoor spaces. As public health guidance changes with increasing vaccination and sustained decrease in infection rates, so should the masking guidance in schools.
Recommendations for masking:
- Masking is one of the temporary measures that can be more easily adjusted throughout the school year.
- The use of NMMs in the school setting should be driven by local epidemiology with age-specific considerations.
- When adequate vaccination rates are obtained such that infection rates and severe disease remain low and stable, masking guidance in schools should follow community guidance for indoor settings.
- Even when no longer mandated, mask use should remain permissive as some persons may choose to do so for a variety of reasons (e.g., underlying health concerns).
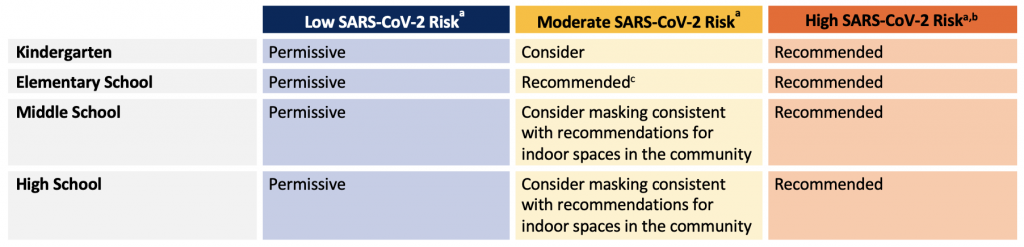
aOutdoor masking is permissive and not specifically recommended except when community transmission is high and physical distancing is not feasible (align with community guidance). bGiven our current and anticipated COVID-19 vaccine coverage, high-risk scenarios imply the presence of a circulating variant of concern with vaccine escape causing significant severe disease. cSome jurisdictions may elect to be more permissive given previous experience in the lower elementary age group.
Physical Distancing
Physical distancing can be a useful temporary measure because SARS-CoV-2 transmission occurs most commonly with close, unprotected contact. However, social interaction is central to child development and should be encouraged, especially in younger children. In low-risk scenarios, distancing should not be recommended or required. In moderate or high-risk scenarios, re-initiation of physical distancing recommendations should be considered, while taking into account the downsides of distancing according to age. Thus, for younger children in particular, cohorting (discussed in the Cohorting Section) and masking are strategies that should be prioritized over physical distancing to allow for close interactions.112 For older students, masking and distancing are preferred strategies to cohorting because of the latter’s adverse impact on schooling, social interactions, sports and extra-curricular activities (see sections on Cohorting and Activities). Modifications to physical distancing recommendations can be accomplished practically during the school year by the type of interactive work. However, significant limitations to group/interactive work should be reserved for the high-risk scenario as groups are an integral component of teaching and learning, and other effective temporary measures can be layered in to reduce the risk of spread in the classroom.
The current physical distancing recommendation in Canada is 2 metres. The WHO and CDC have recommended a distance of at least 1 metre.22,113 A 1-metre separation does provide a degree of protection,102 particularly in the school setting when children are wearing masks during periods of high community prevalence.114 We emphasize that distancing is not an all-or-nothing proposition and increasing distancing will likely diminish SARS-CoV-2 transmission.
Recommendations for physical distancing:
- Physical distancing is not required for any age group in low-risk scenarios.
- In moderate- and high -risk scenarios, distancing should be considered depending on age as follows:
- In kindergarten and elementary years, cohorting and masking should be emphasized over distancing, as outlined in the Cohorting and Masking sections, respectively.
- In middle school and high school, masking should be prioritized over cohorting (see section titled Masking) to optimize the learning model (e.g., allow students to participate in the regular class schedule, avoid condensed learning) and support independent development. Distancing can also be encouraged, while allowing for small group work with a consistent group of students within classes (with mask use as outlined in the section titled Achieving Adequate Indoor Air Quality Through Ventilation and/or Filtration).
- A 1-metre distance between students should be aimed for when distancing is required, provided students are masked.22,113,115 If space in the classroom does not allow for adequate distancing, attention should be paid to other mitigation measures such as ventilation and filtration rather than a return to adaptive models.
- Changes in physical distancing can be accomplished practically during the school year by the type of interactive work. However, it will be important to plan for in-person spacing requirements should individual desk work be required.
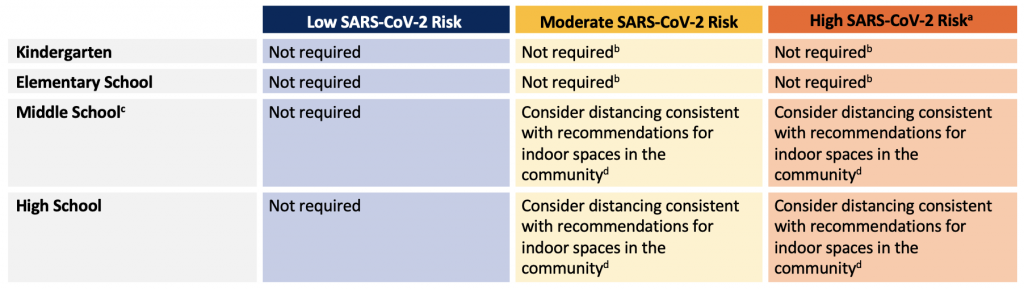
aGiven our current and anticipated vaccine coverage, high-risk scenarios imply the presence of a circulating variant of concern with vaccine escape. bWhile physically distancing within cohorts is not recommended, distancing between cohorts may be recommended when community transmission increases. cThe strategy used in middle school students should take into consideration the strategy used in the rest of the school to optimize processes. d 1-metre distances between students are acceptable for classrooms provided students are masked.
Cohorting
School-based cohorting seeks to limit the number of student and staff who come into close contact with each other and reduce the number of exposures to SARS-CoV-2 infection. It also allows for more timely case and contact follow-up. For kindergarten and elementary school, cohorting reflects the natural state of in-school instruction, and it is an important mitigation strategy in the moderate to high-risk scenarios in this age group.
Cohorting in high schools through the use of adaptive learning models (e.g., quadmester or octomester schedules, blended learning with reduced in-person instruction, hybrid learning, reduced specialized academic instruction/single teacher instruction), during the 2020-2021 school year aimed to reduce contact rates among students. It also enabled public health units to identify specific cohorts with high-risk exposures needing to isolate at home. However, for many students, the adaptive learning models used to deliver education in cohorts were not optimal for learning, development, or social interactions.116,117 Given the lead time required for scheduling /timetabling, it is unlikely that changes will be immediately possible. However, in the context of broad vaccine availability, efforts should be made to return to normal scheduling at the earliest opportunity.
Recommendations for cohorting:
- In kindergarten and elementary school (+/- middle school) and for children and youth with medical complexities:
- The classroom is a natural cohort. In all scenarios, classroom cohorts should be reinforced at the start of the school year so that students stay mostly with the same class group indoors and there is less mixing between classes and years (with allowances for cohort mixing to support specialized education programs, rehabilitation and therapeutic services, transportation).
- These cohorts should be as small as possible; therefore, the smallest class sizes possible should be implemented at the start of the school year to optimize learning and facilitate smaller cohorts should community transmission increase.
- Classroom cohort mixing should be permitted outdoors (e.g., recess).
- In high school (+/- middle school):
- Masking and physical distancing are preferred strategies over cohorting in moderate to high-risk scenarios, alongside vaccine campaigns in under-immunized communities.
- A certain degree of cohorting may be required at the start of the school year to minimize the number of contacts associated with a case and to allow for timely case and contact management. However, efforts should be made to return to normal scheduling at the earliest opportunity.
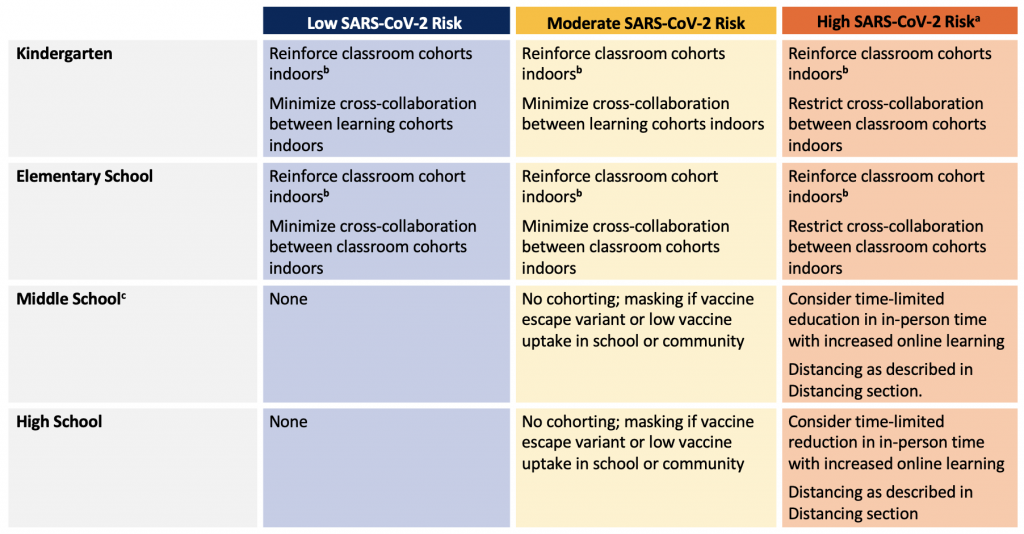
aGiven our current and anticipated vaccine coverage, high-risk scenarios imply the presence of a circulating variant of concern with vaccine escape. bMixing of cohorts should be permitted to allow for access of specialized education programs, rehabilitation and therapeutic services, transportation. cThe strategy used in Middle school students should take into consideration the strategy used in the rest of the school to optimize processes.
In-Person School Gatherings, Activities, and Lunch Hour
Schools provide an environment in which children and youth can participate in physical activities and enriching extra-curricular activities.1 Restrictions were put into place during the 2020-2021 academic year on in-person gatherings, with limited school assemblies, music/theatre instruction, physical education, and extra-curricular clubs and sports, as a health and safety measure.118 These losses have had a substantial impact on children and youth’s physical and mental health and overall wellbeing.119
Other jurisdictions were able to conduct in-person gatherings, music education, clubs and sports during the 2020-2021 academic year, with school-based measures responsive to community burden.120,121 With high vaccine uptake in the community and reduced community transmission, there should be a return to offering these enriching activities to Ontario students during the 2021-2022 academic year, with appropriate mitigation measures as required, and cancellation considered only in high-risk scenarios. The health and safety measures implemented for school-based programs should be consistent with those for similar community-based programs. A mechanism should also be in place to link between the activity and classroom cohorts for prompt identification of SARS-CoV-2 cases and contact tracing.
Music Education (Singing and Instruments)
Recommendations on the delivery of music programs within schools has been developed for Ontario schools that precede a gradual return to regular operations.122 As noted, qualified music teachers are uniquely situated to offer creative solutions, and rely on close administrative collaboration to deliver quality music education to all students. For choir and orchestra in the moderate-risk scenario, instruction can be taken outdoors in smaller, well-spaced groups (weather permitting) or remain indoors with distancing, masking, low-volume singing, and materials for safe wind instrument playing; this could be complemented by music theory, theatre history, or vocal anatomy lessons.123 Students should be offered personal wind instruments, or instructed on proper sanitization of mouthpiece and instrument between uses. Where there are smaller practice rooms that may be difficult to properly ventilate, masks should be worn if possible or the room restricted to individual use. Temporary measures in arts and theatre classes include rehearsing monologues, remote performances, and performances with small casts that do not require close interaction or outdoor rehearsals and performances.
Sports and Physical Education
Recommendations on physical education planning in Ontario schools include raising awareness among students of infection-related risks associated with the activity, administrative support to develop policies and procedures, and communication with the school community as temporary public health measures are introduced or lifted.124
Lunchtime
In high-risk scenarios with standard class sizes, additional measures may reduce transmission risks during lunch hours, when students are in close proximity for prolonged periods of time without masks. For example, lunch and snack times can occur outdoors, when weather permits, with hand hygiene amenities readily accessible at designated locations. When indoors, measures to enable distancing of students during lunch hour include: use of additional indoor spaces such as gyms or other school spaces, shorter lunch times, or staggered lunch breaks. Closing cafeterias has not been shown to significantly reduce SARS-CoV-2 transmission, possibly due to the presence of other mitigation measures.67
General Considerations
Large, well-ventilated spaces should be prioritized for activities where aerosols are likely to be generated outside of the school cohort (e.g., music room for choir and band practice, auditorium for woodwind and brass orchestra and dramatic arts, gymnasium for periods of strenuous physical activity). Plexiglass barriers are generally not recommended, as they have not been shown to reduce SARS-CoV-2 transmission and may in fact alter the airflow, leading to turbulence and recirculation in the room.61,117 Similarly, closing cafeterias, playgrounds and libraries, and wiping down and quarantining books, have not been shown to reduce SARS-CoV-2 transmission, possibly because of the presence of other mitigation measures and the limited role of fomite transmission.67
In high community risk scenarios, the use of rapid antigen screen testing may be considered in order to maintain function of extra-curricular clubs and athletics, particularly those associated with significant aerosol dispersion indoors, such as choir, wind instruments, football and wrestling (“Test-To-Play” strategy, see Testing section).73 Of note, rapid antigen screen testing is most effective alongside other mitigation measures, including distancing, masking, efforts to improve air quality, and outdoor activities and play.125
The following table summarizes recommendations for in-person curricular and extra-curricular programs offered through school settings. Local SARS-CoV-2 patterns and public health decisions during school-related outbreak investigations may influence the risk determination and implementation of temporary measures and/or restrictions.
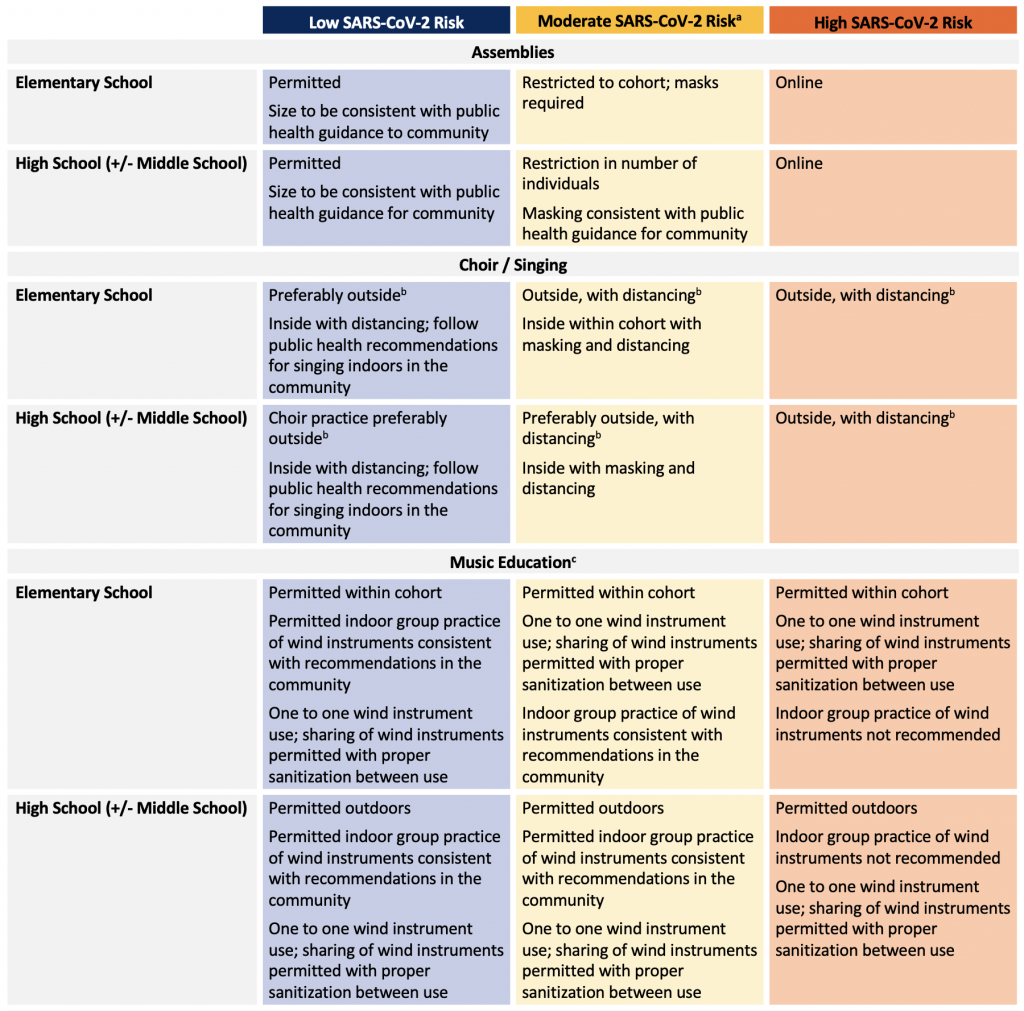

aMeasures reflect in-class instruction with natural cohorts unless otherwise specified; extra-curricular activities should align with specific regional public health guidance. bPublic health units may consider limiting these activities for the outdoors and/or with distancing in the context of local SARS-CoV-2 activity and vaccine coverage rates in schools. cFurther guidance, including the use of materials for safe wind instrument playing, can be found at https://www.omea.on.ca/2021/06/safe-singing-and-playing-in-ontario-schools-document-available-now/ dTest-to-play was a strategy73 implemented in Utah that required testing every 14 days for participants in high school extracurricular activities. It is described in the Utah COVID-19 School Manual126 eDistancing may not be required in middle and high school if the vaccination rate is high.
Transportation to School
School transportation-related guidance from Canada and the US recognizes that communal transportation, such as busing, can increase the risk of SARS-CoV-2 transmission among susceptible children, youth, and adults due to many factors that include variable age ranges and compliance with masking and distancing, prolonged close contact while waiting in line and on the bus, and lack of supervision in some cases.127,128 During periods of low community transmission risk, bus transport should follow local public health guidance as for public transportation. Notably, when students were masked on school buses in North Carolina, the number of children per bus seat (1, 2, or 3) did not affect secondary transmission rates.107
Recommendations for transportation to school:
- In moderate- and high-risk scenarios, temporary health and safety measures should be considered on public transportation, regardless of mask policies at school.
- Measures include active symptom screening by parents or caregivers prior to entering the bus, reducing the number of children on the bus at one time, and masking, particularly when the first two measures are not feasible.
- Windows should be open, weather permitting, to improve air circulation.
Interpretation
We have defined three broad scenarios of COVID-19 disease burden: (1) low-risk, where severe disease requiring hospitalization is limited and sporadic; (2) moderate-risk, where there is early evidence of an upward trajectory in severe disease requiring hospitalization and (3) high-risk, where there are high rates and continued upward trajectory of severe disease requiring hospitalization. SARS-CoV-2 transmission is an important secondary factor that can be considered in defining community risk, particularly early in the school year.
In the low-risk scenarios, recommendations on temporary measures in the school environment include a strategy for contact tracing and low-barrier testing as an early warning system for emerging variants and increased transmission, a permissive approach to masking, and no requirement for distancing or cohorting.
In the moderate-to-high community risk scenarios, an increase in temporary measures would be warranted in schools with emphasis on cohorting and age-dependent masking in kindergarten and elementary school students (without the need for physical distancing) and on masking with or without physical distancing (without the need for cohorting) in middle and high school students. It is recognized that individual jurisdictions in a low-risk scenario in September 2021 may choose more relaxed or more strict temporary measures depending on their local circumstances.
References
1. Gallagher-Mackay K, Srivastava P, Underwood K, et al. COVID-19 and Education Disruption in Ontario: Emerging Evidence on Impacts. Available at: https://doi.org/10.47326/ocsat.2021.02.34.1.0 (accessed June 14, 2021)
2. United Nations. Launch of the Poligy Brief: Education During COVID-19 and Beyond. Available at: https://www.un.org/en/coronavirus/future-education-here (accessed July 9, 2021).
3. Fuller S, Qian Y. Covid-19 and The Gender Gap in Employment Among Parents of Young Children in Canada. Gender & Society. 2021/04/01 2021;35(2):206-217. https://doi.org/10.1177/08912432211001287
4. United Nations Educational Scientific and Cultural Organization (UNESCO). Global tracking of COVID-19 caused school closures and re-openings. Available at: https://en.unesco.org/sites/default/files/en_methogological_note_-_unesco_map_on_covid-19_caused_school_closures_reopening_final.pdf (accessed July 7, 2021).
5. Engzell P, Frey A, Verhagen MD. Learning Loss Due to School Closures During the COVID-19 Pandemic.https://doi.org/10.31235/osf.io/ve4z7.
6. Toronto District School Board. Preliminary Findings on the Impact to Learning Due to the Pandemic. March 31, 2021. Available at: https://pub-tdsb.escribemeetings.com/filestream.ashx?DocumentId=8209 (accessed July 7, 2021).
7. European Commission. Science For Policy Briefs. Educational inequalities in Europe and physical school closures during COVID-19. Available at: https://ec.europa.eu/jrc/sites/default/files/fairness_pb2020_wave04_covid_education_jrc_i1_19jun2020.pdf (accessed July 14, 2021).
8. Azevedo JP, Hasan A, Goldemberg D, Iqbal SA, Geven K. Simulating the Potential Impacts of COVID-19 School Closures on Schooling and Learning Outcomes: A Set of Global Estimates. Available at: https://openknowledge.worldbank.org/bitstream/handle/10986/33945/Simulating-the-Potential-Impacts-of-COVID-19-School-Closures-on-Schooling-and-Learning-Outcomes-A-Set-of-Global-Estimates.pdf?sequence=1&isAllowed=y(accessed July 9, 2021).
9. Thorell L.B., Skoglund C., de la Peña A.G., al. e. Parental experiences of homeschooling during the COVID-19 pandemic: differences between seven European countries and between children with and without mental health conditions. Eur Child Adolesc Psychiatry (2021). https://doi.org/10.1007/s00787-020-01706-1.
10. Cost KT, Crosbie J, Anagnostou E, al. e. Mostly worse, occasionally better: impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. Eur Child Adolesc Psychiatry (2021). https://doi.org/10.1007/s00787-021-01744-3.
11. Ontario Agency for Health Protection and Promotion (Public Health Ontario). Negative impacts of community-based public health measures on children, adolescents and families during the COVID-19 pandemic: update. Toronto, ON: Queen’s Printer for Ontario; 2020. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/he/2021/01/rapid-review-neg-impacts-children-youth-families.pdf?la=en
12. Thorell LB, Skoglund C, de la Pena AG, et al. Parental experiences of homeschooling during the COVID-19 pandemic: differences between seven European countries and between children with and without mental health conditions. European child & adolescent psychiatry. Jan 7 2021;https://doi.org/10.1007/s00787-020-01706-1
13. Grumi S, Provenzi L, Gardani A, et al. Rehabilitation services lockdown during the COVID-19 emergency: the mental health response of caregivers of children with neurodevelopmental disabilities. Disabil Rehabil. Jan 2021;43(1):27-32. https://doi.org/10.1080/09638288.2020.1842520
14. Statistics Canada. Canadians health and COVID-19, by age and gender. Available at: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310080601&pickMembers%5B0%5D=1.8&pickMembers%5B1%5D=3.2&pickMembers%5B2%5D=4.1 (accessed July 7, 2021).
15. De France K, Hancock GR, Stack DM, Serbin LA, Hollenstein T. The mental health implications of COVID-19 for adolescents: Follow-up of a four-wave longitudinal study during the pandemic. Am Psychol. May 24 2021; https://doi.org/10.1037/amp0000838
16. Larsen L, Helland MS, Holt T. The impact of school closure and social isolation on children in vulnerable families during COVID-19: a focus on children’s reactions. European child & adolescent psychiatry. Mar 26 2021; https://doi.org/10.1007/s00787-021-01758-x
17. Couturier J, Pellegrini D, Miller C, et al. The COVID-19 pandemic and eating disorders in children, adolescents, and emerging adults: virtual care recommendations from the Canadian consensus panel during COVID-19 and beyond. J Eat Disord. Apr 16 2021;9(1):46. https://doi.org/10.1186/s40337-021-00394-9
18. Chaabane S, Doraiswamy S, Chaabna K, Mamtani R, Cheema S. The Impact of COVID-19 School Closure on Child and Adolescent Health: A Rapid Systematic Review. Children (Basel). May 19 2021;8(5) https://doi.org/10.3390/children8050415
19. de Lannoy L, Rhodes RE, Moore SA, Faulkner G, Tremblay MS. Regional differences in access to the outdoors and outdoor play of Canadian children and youth during the COVID-19 outbreak. Can J Public Health. Dec 2020;111(6):988-994. https://doi.org/10.17269/s41997-020-00412-4
20. Lynn RM, Avis JL, Lenton S, Amin-Chowdhury Z, Ladhani SN. Delayed access to care and late presentations in children during the COVID-19 pandemic: a snapshot survey of 4075 paediatricians in the UK and Ireland. Archives of disease in childhood. Feb 2021;106(2):e8. https://doi.org/10.1136/archdischild-2020-319848
21. European Centre for Disease Prevention and Control. COVID-19 in children and the role of school settings in transmission – second update (July 8, 2021). Available at: https://www.ecdc.europa.eu/en/publications-data/children-and-school-settings-covid-19-transmission (accessed July 10, 2021).
22. Centers for Disease Control and Prevention (CDC). Guidance for COVID-19 Prevention in Kindergarten (K)-12 Schools. Updated July 9, 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/k-12-guidance.html (accessed July 10, 2021).
23. Milman O, Yelin I, Aharony N, et al. Community-level evidence for SARS-CoV-2 vaccine protection of unvaccinated individuals. Nature medicine. Jun 10 2021; https://doi.org/10.1038/s41591-021-01407-5
24. Hoang A, Chorath K, Moreira A, et al. COVID-19 in 7780 pediatric patients: A systematic review. EClinicalMedicine. Jul 2020;24:100433. https://doi.org/10.1016/j.eclinm.2020.100433
25. Parri N, Lenge M, Buonsenso D, Coronavirus Infection in Pediatric Emergency Departments Research G. Children with Covid-19 in Pediatric Emergency Departments in Italy. The New England journal of medicine. Jul 9 2020;383(2):187-190. https://doi.org/10.1056/NEJMc2007617
26. Hurst JH, Heston SM, Chambers HN, et al. SARS-CoV-2 Infections Among Children in the Biospecimens from Respiratory Virus-Exposed Kids (BRAVE Kids) Study. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. Nov 3 2020; https://doi.org/10.1093/cid/ciaa1693
27. Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta paediatrica. Jun 2020;109(6):1088-1095. https://doi.org/10.1111/apa.15270
28. CDC COVID-19 Response Team. Coronavirus Disease 2019 in Children – United States, February 12-April 2, 2020. MMWR Morbidity and mortality weekly report. Apr 10 2020;69(14):422-426. https://doi.org/10.15585/mmwr.mm6914e4
29. Public Health Agency of Canada. COVID-19 daily epidemiology update. Available at: https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html (accessed July 9, 2021).
30. Kompaniyets L, Agathis NT, Nelson JM, et al. Underlying Medical Conditions Associated With Severe COVID-19 Illness Among Children. JAMA Netw Open. Jun 1 2021;4(6):e2111182. https://doi.org/10.1001/jamanetworkopen.2021.11182
31. Bixler D, Miller AD, Mattison CP, et al. SARS-CoV-2-Associated Deaths Among Persons Aged <21 Years – United States, February 12-July 31, 2020. MMWR Morbidity and mortality weekly report. Sep 18 2020;69(37):1324-1329. https://doi.org/10.15585/mmwr.mm6937e4
32. Gotzinger F, Santiago-Garcia B, Noguera-Julian A, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. The Lancet Child & adolescent health. Sep 2020;4(9):653-661. https://doi.org/10.1016/S2352-4642(20)30177-2
33. Kim L, Whitaker M, O’Halloran A, et al. Hospitalization Rates and Characteristics of Children Aged <18 Years Hospitalized with Laboratory-Confirmed COVID-19 – COVID-NET, 14 States, March 1-July 25, 2020. MMWR Morbidity and mortality weekly report. Aug 14 2020;69(32):1081-1088. https://doi.org/10.15585/mmwr.mm6932e3
34. Leeb RT, Price S, Sliwa S, et al. COVID-19 Trends Among School-Aged Children – United States, March 1-September 19, 2020. MMWR Morbidity and mortality weekly report. Oct 2 2020;69(39):1410-1415. https://doi.org/10.15585/mmwr.mm6939e2
35. Shekerdemian LS, Mahmood NR, Wolfe KK, et al. Characteristics and Outcomes of Children With Coronavirus Disease 2019 (COVID-19) Infection Admitted to US and Canadian Pediatric Intensive Care Units. JAMA pediatrics. Sep 1 2020;174(9):868-873. https://doi.org/10.1001/jamapediatrics.2020.1948
36. Tam H, El Tal T, Go E, Yeung RSM. Pediatric inflammatory multisystem syndrome temporally associated with COVID-19: a spectrum of diseases with many names. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne. Sep 21 2020;192(38):E1093-E1096. https://doi.org/10.1503/cmaj.201600
37. Jiang L, Tang K, Levin M, et al. COVID-19 and multisystem inflammatory syndrome in children and adolescents. The Lancet Infectious diseases. Nov 2020;20(11):e276-e288. https://doi.org/10.1016/S1473-3099(20)30651-4
38. Abrams JY, Oster ME, Godfred-Cato SE, et al. Factors linked to severe outcomes in multisystem inflammatory syndrome in children (MIS-C) in the USA: a retrospective surveillance study. The Lancet Child & adolescent health. May 2021;5(5):323-331. https://doi.org/10.1016/S2352-4642(21)00050-X
39. Dufort EM, Koumans EH, Chow EJ, et al. Multisystem Inflammatory Syndrome in Children in New York State. The New England journal of medicine. Jul 23 2020;383(4):347-358. https://doi.org/10.1056/NEJMoa2021756
40. Feldstein LR, Rose EB, Horwitz SM, et al. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. The New England journal of medicine. Jul 23 2020;383(4):334-346. https://doi.org/10.1056/NEJMoa2021680
41. Whittaker E, Bamford A, Kenny J, et al. Clinical Characteristics of 58 Children With a Pediatric Inflammatory Multisystem Syndrome Temporally Associated With SARS-CoV-2. Jama. Jul 21 2020;324(3):259-269. https://doi.org/10.1001/jama.2020.10369
42. Payne AB, Gilani Z, Godfred-Cato S, et al. Incidence of Multisystem Inflammatory Syndrome in Children Among US Persons Infected With SARS-CoV-2. JAMA Netw Open. Jun 1 2021;4(6):e2116420. https://doi.org/10.1001/jamanetworkopen.2021.16420
43. Office for National Statistics. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 4 June 2021. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/4june2021/(accessed June 26, 2021).
44. Chevinsky JR, Tao G, Lavery AM, et al. Late conditions diagnosed 1-4 months following an initial COVID-19 encounter: a matched cohort study using inpatient and outpatient administrative data – United States, March 1-June 30, 2020. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. Apr 28 2021; https://doi.org/10.1093/cid/ciab338
45. Molteni E, Sudre CH, Canas LS, et al. Illness duration and symptom profile in a large cohort of symptomatic UK school-aged children tested for SARS-CoV-2. medRxiv : the preprint server for health sciences. 2021:2021.05.05.21256649. https://doi.org/10.1101/2021.05.05.21256649
46. Ontario Agency for Health Protection and Promotion (Public Health Ontario). Pediatric post-acute COVID-19 and multisystem inflammatory syndrome in children (MIS-C) – what we know so far. Toronto, ON: Queen’s Printer for Ontario; 2021. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/covid-wwksf/2021/05/wwksf-children-long-term-sequelae.pdf?la=en
47. Radtke T, Ulyte A, Puhan MA, Kriemler S. Long-term Symptoms After SARS-CoV-2 Infection in Children and Adolescents. Jama. Jul 15 2021;doi:10.1001/jama.2021.11880
48. Ontario COVID-19 Science Advisory Table and Modelling Consensus Table. Update on COVID-19 Projections. Available at: https://covid19-sciencetable.ca/sciencebrief/update-on-covid-19-projections-9/ (accessed June 26, 2021).
49. Bourouiba L. The Fluid Dynamics of Disease Transmission. Annual Review of Fluid Mechanics. 2021/01/05 2021;53(1):473-508. https://doi.org/10.1146/annurev-fluid-060220-113712
50. Cowling BJ, Ip DK, Fang VJ, et al. Aerosol transmission is an important mode of influenza A virus spread. Nat Commun. 2013;4:1935. https://doi.org/10.1038/ncomms2922
51. Tellier R, Li Y, Cowling BJ, Tang JW. Recognition of aerosol transmission of infectious agents: a commentary. BMC infectious diseases. Jan 31 2019;19(1):101. https://doi.org/10.1186/s12879-019-3707-y
52. Ontario Agency for Health Protection and Promotion (Public Health Ontario). COVID-19 routes of transmission – what we know so far. Toronto, ON: Queen’s Printer for Ontario; 2020. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/covid-wwksf/2020/12/routes-transmission-covid-19.pdf?sc_lang=en (accessed July 7, 2021)
53. Ontario Agency for Health Protection and Promotion (Public Health Ontario). COVID-19 What We Know So far About….. Routes of Transmission. July 16, 2020. Available at https://www.publichealthontario.ca/-/media/documents/ncov/wwksf-routes-transmission-mar-06-2020.pdf?la=en (accessed December 24, 2020).
54. Ontario Agency for Health Protection and Promotion (Public health Ontario). COVID-19 transmission through large respiratory droplets and aerosols…what we know so far. Toronto, ON: Queen’s Printer for Ontario; 2021. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/covid-wwksf/2021/05/wwksf-transmission-respiratory-aerosols.pdf?sc_lang=en (accessed July 7, 2021).
55. Ontario Agency for Health Protection and Promotion (Public Health Ontario). COVID-19 vaccine uptake in Ontario: December 14, 2020 to June 26, 2021. Toronto, ON: Queen’s Printer for Ontario; 2021. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/epi/covid-19-vaccine-uptake-ontario-epi-summary.pdf?sc_lang=en (accessed July 2, 2021).
56. Lewis D. Does vaccinating adults stop kids from spreading COVID too? Nature Briefing. Available at: https://www.nature.com/articles/d41586-021-01549-z (accessed June 14, 2021).
57. Reuters. School COVID-19 cases spur Israeli parents to vaccinate kids. Available at: https://www.reuters.com/world/middle-east/school-covid-19-cases-spur-israeli-parents-vaccinate-kids-2021-06-22/(accessed June 26, 2021)
58. Centers for Disease Control and Prevention. Hierarchy of Controls. Available at https://www.cdc.gov/niosh/topics/hierarchy/default.html (accessed July 4, 2020).
59. Appel C, Beltekian D, Gavrilov D, et al. Our World in Data: COVID-19 Data Explorer [Internet]. Our World in Data. [cited 2021 Jul 11];Available from: https://ourworldindata.org/coronavirus-data-explorer (accessed July 12, 2021).
60. Public Health Agency of Canada. Individual and community-based measures to mitigate the spread of COVID-19 in Canada. Available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/public-health-measures-mitigate-covid-19.html#a6 (accessed July 10, 2021).
61. Gentles SJ, White C, Murphy S, Cnudde M, Bethel J, M S. Readiness for the safe and successful return to school: Findings from the 2020 Autism Ontario education survey [Report]. Toronto, ON: Autism Ontario; July, 2020. Available at: https://www.autismontario.com/sites/default/files/2020-07/Autism%20Ontario%20Readiness%20for%20School%2030_7_20-1.pdf (accessed July 6, 2021).
62. Rotenberg S, Downer MB, Brown H, et al. COVID-19 Vaccination for People with Disabilities. Updated June 15, 2021. Version 1.1. Available at: https://doi.org/10.47326/ocsat.2021.02.35.1.0.
63. The Hospital for Sick Children. COVID-19: Guidelines for the Delivery of Home and Community Care Services for Children with Medical Complexity at School. Available at: http://www.sickkids.ca/PDFs/About-SickKids/81571-covid19-school-guidelines-medical-complexity.pdf (accessed July 6, 2021).
64. Holland Bloorview Kids Rehabilitation Hospital. Return to School Recommendations for Children with Special Needs. Available at: https://hollandbloorview.ca/sites/default/files/2020-07/HB-BackToSchool-Recommendations.pdf(accessed July 2, 2021).
65. Children’s Hospital of Eastern Ontario. Considerations for the return to school of children and youth with specialized care needs. Available at: https://www.cheo.on.ca/en/about-us/resources/OHT/Return-to-school-of-students-with-specialized-care-needs_English.pdf (accessed July 6, 2021).
66. Government of Ontario. Immunization of School Pupils Act, R.S.O. 1990, c I.1. Available at: https://www.ontario.ca/laws/statute/90i01 (accessed July 12, 2021).
67. Lessler J, Grabowski MK, Grantz KH, et al. Household COVID-19 risk and in-person schooling. Science. Jun 4 2021;372(6546):1092-1097. https://doi.org/10.1126/science.abh2939
68. Thompson A, Stall N, Born K, et al. Benefits of Paid Sick Leave During the COVID-19 Pandemic. Available at: https://covid19-sciencetable.ca/sciencebrief/benefits-of-paid-sick-leave-during-the-covid-19-pandemic/ (accessed May 25, 2021).
69. Ontario Agency for Health Protection and Promotion (Public Health Ontario). COVID-19 prevention measurs in K-12 schools: optimizing screening and masking. December 18, 2020. Availabel at: https://www.publichealthontario.ca/-/media/documents/ncov/sch/2020/12/covid-19-focus-on-optimizing-screening-and-masking.pdf?la=en (accessed January 10, 2021).
70. Ontario Agency for Health Protection and Promotion (Public Health Ontario). Coronavirus disease 2019 and the pediatric population: an umbrella review. November 4, 2020. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/ipac/2020/10/covid-19-pediatric-population-umbrella-review-synthesis.pdf?la=en (accessed January 10, 2021).
71. Kain DC, Stall NM, McGeer AJ, Evans GA, Allen VG, Johnstone J. Low yield of severe acute respiratory coronavirus virus 2 (SARS-CoV-2) asymptomatic routine screen testing, despite high community incidence. Infect Control Hosp Epidemiol. Jun 24 2021:1-2. https://doi.org/10.1017/ice.2021.304
72. Kain D, Stall N, Allen V, et al. Routine Asymptomatic SARS-CoV-2 Screen Testing of Ontario Long-Term Care Staff After COVID-19 Vaccination. Available at: https://covid19-sciencetable.ca/sciencebrief/routine-asymptomatic-sars-cov-2-screen-testing-of-ontario-long-term-care-staff-after-covid-19-vaccination/ (accessed May 25, 2021).
73. Lanier WA, Babitz KD, Collingwood A, et al. COVID-19 Testing to Sustain In-Person Instruction and Extracurricular Activities in High Schools – Utah, November 2020-March 2021. MMWR Morbidity and mortality weekly report. May 28 2021;70(21):785-791. https://doi.org/10.15585/mmwr.mm7021e2
74. Centers for Disease Control and Prevention (CDC). Case Investigation & Contact Tracing Guidance. Available at: https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/appendix.html#contact(accessed July 10, 2021).
75. Ontario Agency for Health Protection and Promotion (Public Health Ontario). Focus on: backward contact tracing. Toronto, ON: Queen’s Printer for Ontario; 2021. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/phm/2021/05/covid-19-backward-contact-tracing.pdf?sc_lang=en (accessed July 1, 2021).
76. Ontario Agency for Health Protection and Promotion (Public Health Ontario) – Provincial Infectious Diseases Advisory Committee. Routine Practices and Additional Precautions in All Health Care Settings. 3rd Edition. Toronto, ON: Queen’s Printer for Ontario; November 2012. Available at: https://www.publichealthontario.ca/-/media/documents/b/2012/bp-rpap-healthcare-settings.pdf?sc_lang=en (accessed July 7, 2021).
77. Clean Hands Save Lives. The Handwashing Song. Available at: https://cleanhandssavelives.org/hand-washing-song/ (accessed July 7, 2021).
78. Somsen GA, van Rijn C, Kooij S, Bem RA, Bonn D. Small droplet aerosols in poorly ventilated spaces and SARS-CoV-2 transmission. The Lancet Respiratory medicine. Jul 2020;8(7):658-659. https://doi.org/10.1016/S2213-2600(20)30245-9
79. Vuorinen V, Aarnio M, Alava M, et al. Modelling aerosol transport and virus exposure with numerical simulations in relation to SARS-CoV-2 transmission by inhalation indoors. Safety science. Oct 2020;130:104866. https://doi.org/10.1016/j.ssci.2020.104866
80. Leclerc Q, Fuller N, Knight L, null n, Funk S, Knight G. What settings have been linked to SARS-CoV-2 transmission clusters? [version 2; peer review: 2 approved]. Wellcome Open Research. 2020;5(83) https://doi.org/10.12688/wellcomeopenres.15889.2
81. Morawska L, Milton DK. It is Time to Address Airborne Transmission of COVID-19. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. Dec 3 2020;71(9):2311-2313. https://doi.org/10.1093/cid/ciaa939
82. Morawska L, Tang JW, Bahnfleth W, et al. How can airborne transmission of COVID-19 indoors be minimised? Environment international. Sep 2020;142:105832. https://doi.org/10.1016/j.envint.2020.105832
83. Gettings J, Czarnik M, Morris E, et al. Mask Use and Ventilation Improvements to Reduce COVID-19 Incidence in Elementary Schools – Georgia, November 16-December 11, 2020. MMWR Morbidity and mortality weekly report. May 28 2021;70(21):779-784. https://doi.org/10.15585/mmwr.mm7021e1
84. Public Health Agency of Canada. COVID-19: Guidance on indoor ventilation during the pandemic. Available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/guide-indoor-ventilation-covid-19-pandemic.html (accessed July 7, 2021).
85. Vakalis D, Lepine C, MacLean HL, Siegel JA. Can green schools influence academic performance? Critical Reviews in Environmental Science and Technology. 2021/07/03 2021;51(13):1354-1396.https://doi.org/10.1080/10643389.2020.1753631
86. American Society of Heating Refridgerating and Air Conditioning Engineers (ASHRAE). Standard 62.1-2019 — Ventilation for Acceptable Indoor Air Quality (ANSI Approved). Available at: www.ashrae.org.
87. Ontario Agency for Health Protection and Promotion (Public Health Ontario). COVID-19: Heating, Ventilation and Air Conditioning (HVAC) Systems in Buildings. August 31, 2020. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/ipac/2020/09/covid-19-hvac-systems-in-buildings.pdf?la=en (accessed September 15, 2020).
88. Li D., Lin E.Z., Brault M.A., Paquette J., Vermund S.H., Godri Pollitt K.J. (2021) Reopening Schools After a Novel Coronavirus Surge. In: Rezaei N. (eds) Coronavirus Disease – COVID-19. Advances in Experimental Medicine and Biology, vol 1318. Springer, Cham. https://doi.org/10.1007/978-3-030-63761-3_44. .
89. Curtius J, Granzin M, Schrod J. Testing mobile air purifiers in a school classroom: Reducing the airborne transmission risk for SARS-CoV-2. Aerosol Science and Technology. 2021/05/04 2021;55(5):586-599. https://doi.org/10.1080/02786826.2021.1877257
90. Ontario Agency for Health Protection and Promotion (Public Health Ontario). Use of portable air cleaners and transmission of COVID-19. December 31, 2020. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/ipac/2021/01/faq-covid-19-portable-air-cleaners.pdf?la=en (accessed January 10, 2021).
91. Amin R, Keilty K, Science M, Orkin J. COVID-19: Guidelines for the delivery of home and community care services for children with medical complexity at school. Available at: https://www.sickkids.ca/siteassets/news/news-archive/2020/covid19-school-guidelines-medical-complexity.pdf (accessed January 10, 2021).
92. Lindsley WG, Derk RC, Coyle JP, al. e. Efficacy of Portable Air Cleaners and Masking for Reducing Indoor Exposure to Simulated Exhaled SARS-CoV-2 Aerosols — United States, 2021. MMWR Morb Mortal Wkly Rep. ePub: 2 July 2021. http://dx.doi.org/10.15585/mmwr.mm7027e1.
93. Xiang J, Huang C-H, Shirai J, et al. Field measurements of PM2.5 infiltration factor and portable air cleaner effectiveness during wildfire episodes in US residences. Science of The Total Environment. 2021/06/15/ 2021;773:145642.https://doi.org/10.1016/j.scitotenv.2021.145642
94. Crowe J, Schnaubelt AT, Schmidt-Bonne S, et al. Pilot program for test-based SARS-CoV-2 screening and environmental monitoring in an urban public school district. medRxiv : the preprint server for health sciences. 2021:2021.04.14.21255036. https://doi.org/10.1101/2021.04.14.21255036
95. Dougherty K, Mannell M, Naqvi O, Matson D, Stone J. SARS-CoV-2 B.1.617.2 (Delta) Variant COVID-19 Outbreak Associated with a Gymnastics Facility – Oklahoma, April-May 2021. MMWR Morbidity and mortality weekly report. Jul 16 2021;70(28):1004-1007. https://doi.org/10.15585/mmwr.mm7028e2
96. Zeng Y, Manwatkar P, Laguerre A, et al. Evaluating a commercially available in-duct bipolar ionization device for pollutant removal and potential byproduct formation. Building and Environment. 2021/05/15/ 2021;195:107750. https://doi.org/10.1016/j.buildenv.2021.107750
97. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. medRxiv : the preprint server for health sciences. Mar 13 2020; https://doi.org/10.1101/2020.03.09.20033217
98. Goldman E. Exaggerated risk of transmission of COVID-19 by fomites. The Lancet Infectious diseases. Aug 2020;20(8):892-893. https://doi.org/10.1016/S1473-3099(20)30561-2
99. World Health Organization. Transmission of SARS-CoV-2: implication for infection prevention precautions. July 9, 2020. Available at: https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions (accessed July 25, 2020).
100. Government of Canada. Hard-surface disinfectants and hand sanitizers (COVID-19): List of disinfectants with evidence for use against COVID-19. Available at: https://www.canada.ca/en/health-canada/services/drugs-health-products/disinfectants/covid-19/list.html (accessed July 14, 2021).
101. Prather KA, Wang CC, Schooley RT. Reducing transmission of SARS-CoV-2. Science. Jun 26 2020;368(6498):1422-1424. https://doi.org/10.1126/science.abc6197
102. Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. Jun 27 2020;395(10242):1973-1987. https://doi.org/10.1016/S0140-6736(20)31142-9
103. Ontario Agency for Health Protection and Promotion (Public Health Ontario). COVID-19 – What We Know So Far About….. Wearing Masks in Public. Last updated 14 Sept 2020. Available at https://www.publichealthontario.ca/-/media/documents/ncov/covid-wwksf/what-we-know-public-masks-apr-7-2020.pdf?la=en (accessed December 24, 2020).
104. Brooks JT, Butler JC. Effectiveness of Mask Wearing to Control Community Spread of SARS-CoV-2. Jama. Mar 9 2021;325(10):998-999. https://doi.org/10.1001/jama.2021.1505
105. Doyle T, Kendrick K, Troelstrup T, et al. COVID-19 in Primary and Secondary School Settings During the First Semester of School Reopening – Florida, August-December 2020. MMWR Morbidity and mortality weekly report. Mar 26 2021;70(12):437-441. https://doi.org/10.15585/mmwr.mm7012e2
106. Falk A, Benda A, Falk P, Steffen S, Wallace Z, Hoeg TB. COVID-19 Cases and Transmission in 17 K-12 Schools – Wood County, Wisconsin, August 31-November 29, 2020. MMWR Morbidity and mortality weekly report. Jan 29 2021;70(4):136-140. https://doi.org/10.15585/mmwr.mm7004e3
107. The ABC Collaborative. COVID-19 and Schools: The Year in Review and a Path Forward. Available at: https://urldefense.com/v3/__https://abcsciencecollaborative.org/wp-content/uploads/2021/06/ABC_year-in-review_29jun2021-final.pdf (accessed July 2, 2021).
108. Brandal LT, Ofitserova TS, Meijerink H, et al. Minimal transmission of SARS-CoV-2 from paediatric COVID-19 cases in primary schools, Norway, August to November 2020. Euro surveillance : bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin. Jan 2021;26(1) https://doi.org/10.2807/1560-7917.ES.2020.26.1.2002011
109. Esposito S, Principi N. To mask or not to mask children to overcome COVID-19. Eur J Pediatr. Aug 2020;179(8):1267-1270. https://doi.org/10.1007/s00431-020-03674-9
110. Nobrega M, Opice R, Lauletta MM, Nobrega CA. How face masks can affect school performance. Int J Pediatr Otorhinolaryngol. Nov 2020;138:110328. https://doi.org/10.1016/j.ijporl.2020.110328
111. Ruba AL, Pollak SD. Children’s emotion inferences from masked faces: Implications for social interactions during COVID-19. PloS one. 2020;15(12):e0243708. https://doi.org/10.1371/journal.pone.0243708
112. Public Health Agency of Canada. COVID-19 guidance for schools Kindergarten to Grade 12. Updated February 12, 2021. Available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/guidance-schools-childcare-programs.html (accessed April 11, 2021).
113. van den Berg P, Schechter-Perkins EM, Jack RS, et al. Effectiveness of three versus six feet of physical distancing for controlling spread of COVID-19 among primary and secondary students and staff: A retrospective, state-wide cohort study. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. Mar 10 2021; https://doi.org/10.1093/cid/ciab230
114. Hershow RB, Wu K, Lewis NM, et al. Low SARS-CoV-2 Transmission in Elementary Schools – Salt Lake County, Utah, December 3, 2020-January 31, 2021. MMWR Morbidity and mortality weekly report. Mar 26 2021;70(12):442-448. https://doi.org/10.15585/mmwr.mm7012e3
115. Tomshine JR, Dennis KD, Bruhnke RE, et al. Combined Effects of Masking and Distance on Aerosol Exposure Potential. Mayo Clinic Proceedings. Available at: https://doi.org/10.1016/j.mayocp.2021.05.007.
116. Toronto District School Board. Student Winter 2021 Check-in Survey. Available at: https://www.tdsb.on.ca/Portals/research/docs/School%20During%20the%20Pandemic/Student_Check-in_Survey_202021_Ward.pdf (accessed June 26, 2021)
117. Fraser Mustard Institute for Human Development: Policy Bench. Effects of School Closures During the COVID-19 Pandemic on Achievement Gaps and Learning Inequalities: Literature Review. Available at: https://socialwork.utoronto.ca/projects/ (accessed July 10, 2021).
118. Office of the Premier. Ontario Releases COVID-19 Management Plan for Schools. Available at: https://news.ontario.ca/en/release/58136/ontario-releases-covid-19-management-plan-for-schools
119. People for Education. The far-reaching costs of losing extracurricular activities during COVID-19. Available at: https://peopleforeducation.ca/wp-content/uploads/2021/04/People-for-Education-The-Cost-of-Losing-Extra-Curricular-Activities-April-2021.pdf (accessed June 26, 2021).
120. Honein MA, Barrios LC, Brooks JT. Data and Policy to Guide Opening Schools Safely to Limit the Spread of SARS-CoV-2 Infection. Jama. Mar 2 2021;325(9):823-824. https://doi.org/10.1001/jama.2021.0374
121. Centers for Disease Control and Prevention (CDC). Operating schools during COVID-19. Updated October 29, 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/schools.html (accessed December 24, 2020).
122. Ontario Music Educators’ Association. Safe Singing and Playing in Ontario Schools Document available NOW. Available at: https://www.omea.on.ca/2021/06/safe-singing-and-playing-in-ontario-schools-document-available-now/(accessed July 7, 2021).
123. Ontario Agency for Health Protection and Promotion (Public Health Ontario). Singing and playing wind instruments – environmental scan related to COVID-19. Toronto, ON: Queen’s Printer for Ontario; 2020. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/main/2021/01/covid-19-environmental-scan-singing-wind-instruments.pdf?la=en (accessed June 26, 2021).
124. Ontario Physical Activity Safety Standards in Education. COVID-19 Considerations for Physical Education. Available at: https://safety.ophea.net/tools-resources/covid-19-considerations-physical-education (accessed July 7, 2021).
125. Moreno GK, Braun KM, Pray IW, et al. SARS-CoV-2 transmission in intercollegiate athletics not fully mitigated with daily antigen testing. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. May 12 2021; https://doi.org/10.1093/cid/ciab343
126. Utah Department of Health. COVID-19 School Manual: K-12 public, private, and charter schools. Available at: https://coronavirus-download.utah.gov/School/COVID-19_School_Manual_FINAL.pdf (accessed July 11, 2021).
127. Public Health Agency of Canada. COVID-19 guidance for schools Kindergarten to Grade 12. Date modified: August 12, 2020. Available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/guidance-schools-childcare-programs.html (accessed June 11, 2021).
128. American Academy of Pediatrics. COVID-19 Planning Considerations: Guidance for School Re-entry. Available at: https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-planning-considerations-return-to-in-person-education-in-schools/#.XvZQ5fK-xNs.email (accessed July 10, 2021).
Document Information & Citation
Author Contributions: MS, NT, and AB conceived the Science Brief. MS, NT, AB, RC, PJ, and KB wrote the first draft of the Science Brief. All authors revised the Science Brief critically for important intellectual content and approved the final version.
Additional members of the writing group:
Hospital for Sick Children: Carolyn Beck, Cindy Bruce-Barrett, Aaron Campigotto, Jeremy Friedman, Ian Kitai, Shaun Morris, Julia Orkin, Stanley Read, Rachel Solomon, Laurie Streitenberger, Anupma Wadhwa, and Valerie Waters.
Unity Health: Justine Cohen-Silver, Sloane Freeman, and Kevin Schwartz.
Children’s Hospital of Eastern Ontario: Charles Hui, Lindy Samson, and Ken Farion.
Holland Bloorview Kids Rehabilitation Hospital: Golda Milo-Manson.
Children’s Hospital at London Health Sciences Centre: Michelle Barton-Forbes and Michael Silverman.
McMaster Children’s Hospital: Dominik Mertz, Jeffery Pernica, Fiona Smaill, and Jacqueline Wong.
The authors would like to thank Nigel Bariffe, Stacie Carroll, Ruth Dawson, Michelle Foote, Michele Giroux, Monica Hau, Ryan Imgrund, Norah Marsh, Laura McCoy, Giovanna Panzera, Tony Pontes, Abdu Sharkawy, the Ontario Principals’ Council (OPC), the Catholic Principals’ Council of Ontario (CPCO), and the Association Des Directions et Directions Adjointes des Ecoles Franco-Ontariennes (ADFO) for their contribution to this Science Brief.
Citation: Science M, Thampi N, Bitnun A, et al. School Operation for the 2021-2022 Academic Year in the Context of the COVID-19 Pandemic. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2(38). https://doi.org/10.47326/ocsat.2021.02.38.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners can be found at https://covid19-sciencetable.ca/. The declarations of interest of external authors can be found under Additional Resources.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners.
