Key Message
Increasing physical activity and decreasing sedentary behaviour have positive effects on mental well-being and are associated with reduced symptoms of depression and anxiety. These effects were well-established prior to the COVID-19 pandemic. Overall, movement behaviours and mental health status worsened among Canadians during the COVID-19 pandemic. Physical activity in some groups, including children, has been disproportionately affected during the pandemic by measures such as school and recreation closures. Further, a lack of safe, accessible physical activity opportunities for some populations will persist past the pandemic due to structural inequities such as inequities in access to indoor or outdoor recreation spaces, as well as built environment features, which may ultimately negatively impact mental health. Promoting physical activity can help optimize both physical and mental health among Ontarians during and beyond the COVID-19 pandemic. Maintaining and improving emotional well-being through engagement in physical activity may be facilitated by providing publicly accessible and proportionally distributed indoor and outdoor recreation spaces, as well as supporting policies which address the relationship between the built environment and physical activity.
Summary
Background
Optimal movement behaviours through regular physical behaviour and minimizing sedentary behaviour to promote mental and physical well-being are outlined in the Canadian 24-hour Movement Behaviour Guidelines and by the World Health Organization (WHO). These guidelines recommend that all Canadians be routinely active, engaging in a minimum of 150 minutes of moderate-to-vigorous intensity physical activity per week for adults, and limit sedentary behaviour by reducing low-movement activities during awake hours. Evidence suggests clear associations between engaging in physical activity and lower rates of depression and anxiety across the lifespan. Even when minimal physical activity levels are not met, some physical activity is better than doing none. Prior to the COVID-19 pandemic, Statistics Canada reported that Canadians spent the majority of time being sedentary and did not meet guidelines.
Questions
What has been the impact of changes in levels of physical activity or sedentary behaviour during the COVID-19 pandemic on mental health in the general population?
How can levels of physical activity be optimized during the pandemic and beyond?
Findings
Patterns of declining rates of physical activity worsened during the COVID-19 pandemic, as Ontarians and other Canadians were significantly less active and even more sedentary. Studies have associated these rapid declines with pandemic-related measures, including closures of schools and recreation. However, physical activity patterns across Ontario’s diverse population prior to and during the COVID-19 pandemic are demonstrative of inequities in the availability of supports needed by Ontarians to maintain, re-engage, start and sustain regular performance of optimal movement behaviours, with some demographic groups having fewer resources (such as living in crowded or small spaces, lack of private yard/green space, inadequate childcare or caregiving support) to engage in physical activity. Built environment factors, including neighbourhood walkability, are also important drivers of physical activity. Global data indicates that participation in physical activity has been associated with improved quality of life, well-being, and reduced depressive symptoms and anxiety during the pandemic.
Interpretation
Considerations of equity, access and the social determinants of health that limit the ability of all Ontarians to become more active in the context of the COVID-19 pandemic and beyond are critical for policymakers. This includes the availability, safety and accessibility of indoor, outdoor or green spaces for physical activity. However, access to recreation and green spaces is not equitably distributed across neighbourhoods in many Ontario communities. Further, considerations of the built environment, and ways to encourage physical activity through increased walkability can have impactful changes on opportunities for physical activity to a broad segment of Ontarians, which may in turn enhance mental well-being. Policymakers should consider health-in-all policies and public health should collaborate with municipal and regional planners to promote healthy community design. Opportunities to improve and encourage physical activity as a means to promote mental wellness are a critical step in the recovery process from the COVID-19 pandemic.
Full Text
Background
Movement behaviours include physical activity (PA), which is movement done at any level of skill, and sedentary behaviour (SB), referring to any low-movement awake behaviour (e.g., activities performed while sitting or reclining.1 Both PA and SB impact health across the lifespan.2–5 While the benefits of regular PA on physical health are well-established, the 2020 World Health Organization (WHO) guidelines acknowledge the impact of PA on mental health for the first time. Mental health refers to a state of well-being in which an individual realizes his or her own abilities, can cope with the normal stresses of life, work productively, and can contribute to his or her community.6 The beneficial effects of PA on mental health appear to be attributable to improved ability to manage stress7 and increased resilience, or ability to buffer stressful events.8,9 Although a bi-directional connection between PA levels and MH has been documented,10,11 studies that experimentally withdraw exercise behaviour in healthy individuals consistently demonstrate increases in depressive symptoms and anxiety.12 The associations between PA and mental health in the general population are evidenced by cross-sectional and prospective studies, as well as clinical trials, with PA being associated with a lower prevalence of depression and anxiety.13–18 Two recent Canadian studies showed that a combination of high PA and low SB were associated with better mental well-being.19,20 The benefits of PA on mental health have been demonstrated for healthy individuals, as well as those with a previous history of depression.14,21
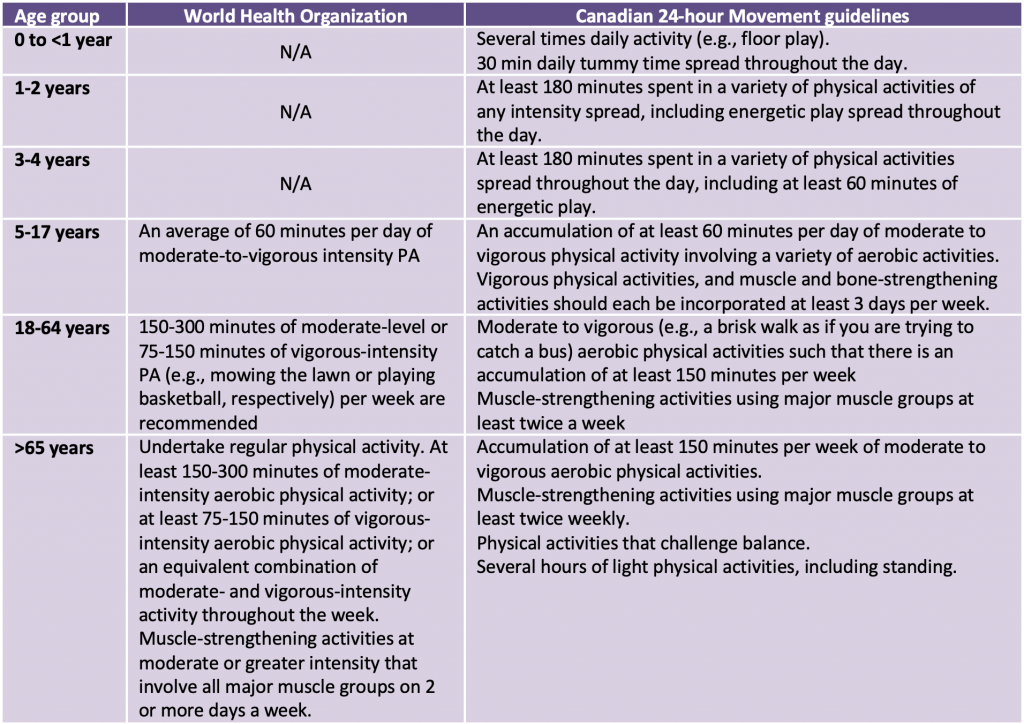
Guidelines for PA vary by age group and approach. Table 1 outlines the WHO guidelines, as well as the Canadian 24-hour Movement guidelines. Consistent with the minimum recommendations for PA, reduced mental health burden was most strongly associated with 45 minutes of activity performed 3 to 5 times a week.14,21
Prior to the COVID-19 pandemic, only half of Canadians reported meeting the Canadian 24-hour Movement guidelines for PA (2018 and 2019 Canadian Health Measures Survey),22 although activity tracking devices that monitor actual movement suggest that the proportion of Canadian adults achieving recommended PA guidelines may be much lower.23 However, there is evidence of physical and mental health benefits even for those not meeting PA or movement guidelines. Light-intensity PA, such as vacuuming or other activities of daily living, reduces the amount of time spent sedentary and improves physical and mental health outcomes.24,25Healthy individuals who performed PA of any type were more likely to report greater emotional and physical well-being regardless of individual baseline fitness level.26
In Ontario, public health measures to mitigate the spread of SARS-CoV-2 have included periods of closures of both indoor and outdoor recreational facilities alongside stay-at-home orders. This brief explores the impact of the COVID-19 pandemic on PA and also considers opportunities to optimize and increase PA among Ontarians.
Questions
What has been the impact of changes in levels of physical activity (PA) or sedentary behaviour (SB) during the COVID-19 pandemic on mental health in the general population?
How can levels of physical activity be optimized during the pandemic and beyond?
Findings
Changes to Physical Activity and Sedentary Behaviour during the COVID-19 Pandemic
Stay-at-home orders, as well as closures of indoor and outdoor spaces to mitigate the spread of SARS-CoV-2 both globally and in Ontario have led to the unintended consequence of reducing PA.27,28 In Canada, PA significantly declined following the start of the pandemic in March 2020, as evidenced by decreases in moderate-to-vigorous PA, light PA, the average number of steps taken and increased time spent sedentary during the early part of the pandemic.29,30 Further, light PA and average number of steps taken remained low, suggesting fewer opportunities to engage in incidental PA and sustained increases in SB overall.29 A survey of Canadian adults undertaken in December 2020 and March 2021 that asked about current physical activity and sport participation, and how it relates to pre-pandemic activity, found that moderate-to-vigorous intensity PA decreased and SB increased across age groups.31
Overall, Canadians who reported having better mental health during the first few months of the pandemic were more likely to have had higher levels of physical activity during this time.32 These findings parallel global studies of the pandemic showing that PA was associated with improved quality of life and well-being, and fewer depressive and anxiety symptoms in the general adult population in the US and beyond.8,33–41 In one of the first Canadian studies of PA during the pandemic, lack of access to adequate space and equipment due to the widespread closure of gyms and other shared facilities, lack of time and poor motivation were cited as key reasons for decreased PA levels among the general public.29 Lack of space and equipment contributed to decreased motivation to engage in PA, while other factors accounting for poor motivation were anxiety and inadequate social support in a survey of 1,669 Canadians, comprised primarily of women aged 18-29 years.42
Global studies reported that amongst individuals who engaged in regular PA pre-pandemic, reductions in PA following onset of the pandemic were associated with increase in negative mood states including depression.43–45 However, reduction in PA frequency with the onset of the pandemic was not universal. Those who were previously inactive but who maintained or increased their PA levels during the pandemic had higher social, emotional, and psychological health and lower generalized anxiety symptoms compared to those who decreased their PA levels.46 These findings were also observed in older adults: those with low levels of PA pre-pandemic showed immediate physical and psychological benefits upon starting PA.45
In terms of level of intensity of PA and its association with mental health, moderate-to-vigorous levels of PA, as typically prescribed by WHO and other guidelines, have been linked to reduced levels of depression and anxiety during the pandemic.37,47–49 However, it is notable that other studies have shown that engaging in any intensity level of PA, which can include household chores such as vacuuming or active transport such as walking while conducting errands, was associated with improved quality of life and decline in negative psychosocial effects of pandemic-related restrictions.34,48
A recent systematic review and meta-analysis of 65 studies on the effects of the pandemic on SB showed that across all age groups (children and youth, adults), SB increased during the pandemic and was attributable to increased “screen time” or greater use of computers or other devices,50 including 5 Canadian studies.51–55Further, the review established that increased time spent in SB was associated with poorer overall mental health and increased risk of depression and anxiety across all age groups. A more recently published Canadian study reported that increases in SB were evident within the first month of the pandemic.30 Thus, both increased SB and reduced PA during the pandemic have been linked to poorer mental health outcomes, while maintenance or increase of pre-pandemic levels of PA was associated with better mental health in Canada and globally.
Physical Activity and Sedentary Behaviour during COVID-19 for Specific Subgroups
Children and Youth
PA during childhood and adolescence is associated with improved physical and cognitive outcomes56 and increased physical self-perception and self-esteem.57 Before the COVID-19 pandemic, 12.7% of children and youth ages 5 to 17 met 24-hour movement guidelines.58 During the first months of the COVID-19 pandemic in Canada, fewer than 5% of children and 1% of youth met 24-hour movement guidelines.59 This drop in PA persisted during the first two waves of the pandemic with fewer than 5% of children and less than 2% of youth meeting the movement guidelines.60 Given closures of schools and recreation, the extent to which children and youth engage in PA during the pandemic has been tightly linked to parental encouragement and support and parents’ own PA behaviour,54 which in turn has been impacted by the availability of leisure time for parents and childcare or caregiving.30,61 Sharp increases in screen time for children and youth have been observed in Ontario and globally during the COVID-19 pandemic.62
Young Adults
Pre-pandemic, only 10% of Canadian post-secondary students met the Canadian 24-Hour Movement Guidelines.20 A recent population-based survey found that the association between low PA and increased stress during the pandemic was the strongest in this age group.63 Students who engaged in PA had lower levels of anxiety and depression compared to inactive students.64 However, access to safe spaces for PA and recreation differed by community and neighbourhood. There is a growing body of Canadian literature identifying a relationship between the built environment and PA across age groups. A study of families with children aged 9-14 years in Saskatoon found that those living in neighbourhoods with high density of destinations and neighbourhood recreation amenities such as parks and green space were less sedentary overall and that this was more pronounced during spring and summer months.65 A large national sample of adolescents in the United States surveyed early in the COVID-19 pandemic found that a lower proportion of racial/ethnic minority adolescents and those from lower socioeconomic status households met moderate-to-vigorous physical activity guidelines during the pandemic compared to those from higher socioeconomic status households.66
Older Adults
The mental health benefits of PA in older adults include greater resilience and fewer depressive symptoms and negative emotions.45 Pre-pandemic, about 20% of older adults in Canada 65+ years of age met PA guidelines, as compared with 45% of 18-64-year-olds, and slightly less than 12% of older adults met the SB guidelines, as compared to 19.4% of 18-64-year-olds.67 Within the 60-70 year old age group in Canada, women are less likely to achieve PA recommendations compared to men.23,68 Increased caution amongst older adults about the risk of complications post-SARS-CoV-2 infection has led to greater social isolation and decreased PA in this age group globally which was particularly pronounced for older adults living in long-term care or other congregate settings.45 Maintaining social ties was identified as essential for encouraging older adults to exercise during the pandemic.59 Older adults who met the minimum WHO recommendations for moderate-vigorous and vigorous PA during the pandemic showed increased positive affect and fewer depressive symptoms.8 Even older adults with low levels of PA prior to the COVID-19 pandemic experienced acute physical and psychological benefits upon starting PA.45
Women
Prior to the COVID-19 pandemic, Canadian women were less likely to meet PA guidelines compared to men.23,67 This trend has continued during the pandemic, with women less physically active than men, reporting more barriers and fewer facilitators to engaging in PA and, in addition, experiencing significantly more generalized anxiety or stress due to the pandemic compared to men.46,69 One contributing factor may be that women have been disproportionately impacted by child-care responsibilities due to the closures of schools and daycare, and have had reduced labour force participation during the pandemic.70 These factors have a downstream effect of increased responsibilities within the home and reduced time for PA. Amongst older adults, women in Canada experienced a greater increase in social isolation during the pandemic compared to men.71 Lower levels of PA and increased SB during the pandemic, compared to 6 months prior, were associated with greater deterioration in mental health in Canadian women in early adulthood, although one motivator of PA was relief of anxiety.42
Strategies to Optimize Physical Activity during the Pandemic and Beyond
During the pandemic, disruptions to usual routines and additional stress and workload shifts created inequities in the support needed by Ontarians to maintain, re-engage, start and sustain regular performance of optimal movement behaviours. Strategies described below were categorized according to the health impact pyramid, when relevant, which describes a framework for public health action considering the level of population impact and individual effort required at various levels.72 Policies need to extend beyond simply raising awareness about the need for increased PA and their benefits to mental health, and instead offer definitive guidance to the public, address inequities in access to spaces for PA, and offer supports to help specific groups engage in PA.
Public Education
There is a need for public engagement and education on relevant guidelines related to movement behaviours and engagement in PA. (Table 1).73,74 Furthermore, broader public messaging of the benefits of increased PA and lower SB on mental health, in addition to physical health, is needed. A national survey of Canadians suggested that additional education is needed to inform the general public that behavioural activation is important for overall mental health and effective in treating and preventing depression.75 Indeed, education about the role of PA to lower mood and anxiety symptoms could increase intentions to engage in PA during the pandemic.76
Finally, promoting messaging that even small lifestyle changes that involve PA may contribute to mental and physical well-being may encourage individuals to reduce levels of SB by engaging in PA. A growing body of movement behaviour research, along with recent WHO guidelines, suggests that any level of movement can constitute PA.1,77,78 Measurable physical benefits are observed when individuals change from habitual sedentary behaviour to being physically active for 30 minutes twice a week, which is lower than most guideline recommendations.79 In a Canadian context, it has already been suggested that rather than only focusing on recommending the regular performance of moderate to vigorous levels of physical activity, health promotion messaging should encourage individuals to replace SB with any type of PA.20
Clinical Interventions: Prescribing Exercise
Physicians can help encourage PA by recommending exercise, and time in green space for patients, such as the recent PaRx program launched in Canada in November 2020 whereby health care professionals can prescribe a Parks Canada Discovery Pass to patients.80 Exercise prescribing, training and education have been incorporated in the management of diabetes,81 cancer82 and cardiac rehabilitation,83 but overall, is not regularly emphasized by healthcare professionals.81 This may be attributable to lack of time, training and support for HCP to optimally prescribe exercise for a variety of patients and the suitability of these highly contextual interventions to the broad Canadian public.84 There is also a lack of consensus about the frequency, dose, and type of physical training suitable for most clinical populations.83
Socioeconomic Factors: Address Inequities in Access to Spaces for Physical Activity
The closure of indoor and outdoor recreational settings sporadically since the onset of the COVID-19 pandemic in March 2020 has had unequal impacts on PA. Living in a house with access to a backyard, as opposed to an apartment, and away from major streets was associated with increased participation in outdoor activities among Canadian children and adults during the early months of the COVID-19 pandemic, which included orders to reduce mobility and stay at home.53,85 In addition, access to parks in high-density neighbourhoods increased outdoor activity and the likelihood of meeting movement guidelines among Canadian youths during that period.53 During the pandemic, there were a number of temporary initiatives, such as reallocation of roadway space from cars to forms of active transit such as bicycles (e.g., Active TO) to improve access to outdoor recreation. However, sustainable and long-term solutions that acknowledge the role of the built environment on PA engagement and on mental health are needed.
Access to PA in a natural environment or green space can help facilitate PA,86 reduce SB,87,88 and enhance both physical and mental health.89–91 During the pandemic, Canadians who engaged in outdoor PA reported better mental health.32,46 Other global data suggested that green spaces encouraged health-promoting behaviours, including PA and social engagement during the pandemic.92
A 2015 evidence-based review from Toronto Public Health highlighted the need for access to green space for physical and mental health.93 However, green space is not equitably distributed across neighbourhoods in many Ontario cities. Forest canopy coverage tends to increase with household income across urban neighbourhoods.94 Overall, low-income and racialized neighbourhoods have reduced access to green space in urban settings95 and are either located within downtown areas with a high concentration of high-rise buildings or on the periphery of the city with low walkability.
At the same time, the relationship between the built environment and mental health is complex. A systematic review reported that in low-income neighbourhoods in Toronto, mental health appeared to decrease with increasing green space.96 The report suggested that increases in the quantity of green space must also be accompanied by improvements in access and quality of the environment, such as ensuring public perception of safety, lower levels of crime and violence, and the availability of facilities such as public toilets, benches, and playground equipment in these spaces. Investments are needed to increase equitable access to public indoor and outdoor facilities or spaces through improvements in safety of existing spaces, development of additional facilities in low-income or racialized neighbourhoods, and increased availability of public transportation to green spaces outside of urban areas.
Changing the Context to Make Individuals’ Default Decisions Healthy: Policies Related to the Built Environment
The term built environment refers to the human-made environment that provides the setting for human activity, including homes, buildings, zoning, streets, sidewalks, open spaces, transportation options, and other features.97 More simply, it can be defined as “the human-made space in which people live, work, and recreate on a day-to-day basis.”98 An emerging consensus is that more dense and compact communities with access to green space are a best practice in urban planning.99 Further, built environment features such as increased neighbourhood density, improving neighbourhood walkability, quality of parks and playgrounds, and providing adequate active transport infrastructure as well as other amenities are associated with increased levels of PA.100 These built environment features are the result of policy development and collaboration across public sectors such as urban planning, land use, parks and recreation and transportation at local municipal, regional, provincial/territorial and federal levels. Given that many levers for changing the existing built environment are found in other policy arenas, beyond the scope of public health practice and policy, collaboration between public health professionals and the various public sectors are needed. Such collaborations can inform the development of external policies to endorse improvements in infrastructure to support population health and healthy lifestyle behaviours, including regular PA.
Further, built environment features need to be equitably distributed, yet Canadian and other evidence suggests that infrastructure improvements tend to benefit socioeconomically advantaged groups.100,101 Policies that support equal distribution of built environment features that facilitate PA will require endorsement by public health professionals, decision-makers and the public. Consideration should be placed on prioritizing enhancement of the built environment in low socioeconomic neighbourhoods, expanding and improving diverse forms of accessible and connected green spaces in underserved and disadvantaged areas to support physical and mental health, and creating opportunities for vulnerable or priority populations (e.g., low socioeconomic status, older adults, those with disabilities or chronic health conditions) to contribute to decision-making processes for interventions to the built environment.102 In order to address ongoing inequities in the distribution of, and access to, factors in the built environment that increase PA,100 it is necessary to integrate health and equity into regular planning processes with the support of trusted and resourced partnerships across public sectors.103
In addition to the policy window approach referenced above, public health professionals can establish project-specific collaborations with urban planning and other policy professionals in these external arenas to offer their expertise in health data, evidence synthesis, and evaluation to both describe current conditions and advance the profile of built environments that support PA.104,105
Interpretation
Optimal movement behaviours (i.e., increased PA and reduced SB) provide protective effects on mental well-being across the lifespan. Prior to COVID-19, at least 1/3rd of Canadians were not meeting international or national recommendations for PA, and instead spent much of the time sedentary. These patterns were exacerbated by pandemic-related closures of schools and recreation spaces.
In Canada, all forms of PA (e.g., moderate-to-vigorous, light, and steps) significantly declined, accompanied by increased SB, following the start of the pandemic.29 The available evidence suggests that individuals who engaged in PA during the pandemic have been less likely to experience depression and anxiety, while those who engaged in regular PA prior to the pandemic and continued have been less likely to experience negative mental health effects during this challenging time. Thus, it has been suggested that those who are more sedentary and inactive should be prioritized for mental health support.37 A recent commentary in the Canadian Journal of Public Health stated that the preservation and promotion of access to outdoor play, especially as children recover from periods of school closures in Ontario from March-June 2020, January -June 2021, and January 2022 should be a top public health priority.106
Strategies to increase physical activity in the population should be comprehensive and address individual, clinical, policy and underlying socioeconomic factors to enable participation across the life course.
At the individual level, public education to build knowledge and motivation to engage in PA are critical requirements for participation. Such messaging should also consider the cultural, sociological, and economic differences that reflect a target audience’s existing views, needs and practices (e.g., young and older Ontarians, lower-income and under-resourced communities, Indigenous communities, newcomer groups, Ontarians living with a disability). In addition, health promotion efforts may need to differentially target Ontarians depending on their current activity levels, and various motivational and anxiety-reducing strategies are needed to integrate movement behaviours into daily life.49,107
The healthcare sector also plays an important role with clinicians having numerous regular opportunities to emphasize the importance of physical activity to health and prescribe exercise to their patients to improve health outcomes. Further efforts to increase the knowledge and efficacy of healthcare providers and access to referrals for physical activity may support increased participation for some patient populations.
Policies related to the built environment play a critical role in creating enabling environments where physical activity becomes less of an onerous choice for individuals and creates healthy communities where daily movement is the norm. Policymakers should consider health-in-all policies and public health should collaborate with municipal and regional planners to promote healthy community design to facilitate PA, with the goals of benefiting mental, as well as physical, well-being.
Methods Used for This Science Brief
A rapid review of PubMed, Google Scholar, the COVID-19 Rapid Evidence Reviews, and the World Health Organization’s Global Literature on Coronavirus Disease, as well as a cited literature search in Web of Science began on May 17, 2021 and was completed on June 28, 2021. Reports citing relevant articles and reference lists of identified articles were also reviewed during this time. Keywords used in this review were: physical activity, exercise, sedentary behaviours, movement behaviours, mental health, and COVID-19, however, these were tailored for each database. Specific literature describing these topics was identified manually or through key informants by brief authors following these preliminary database searches.
References
1. Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451-1462. https://doi.org/10.1136/bjsports-2020-102955
2. Edwardson CL, Gorely T, Davies MJ, et al. Association of sedentary behaviour with metabolic syndrome: A meta-analysis. PLOS ONE. 2012;7(4):e34916. https://doi.org/10.1371/journal.pone.0034916
3. Kandola A, Lewis G, Osborn DPJ, Stubbs B, Hayes JF. Depressive symptoms and objectively measured physical activity and sedentary behaviour throughout adolescence: A prospective cohort study. Lancet Psychiatry. 2020;7(3):262-271. https://doi.org/10.1016/S2215-0366(20)30034-1
4. Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults. Ann Intern Med. 2015;162(2):123-132. https://doi.org/10.7326/M14-1651
5. Kraus WE, Powell KE, Haskell WL, et al. Physical activity, all-cause and cardiovascular mortality, and cardiovascular disease. Med Sci Sports Exerc. 2019;51(6):1270-1281. https://doi.org/10.1249/MSS.0000000000001939
6. World Health Organization. Global action plan on physical activity 2018-2030: More active people for a healthier world.; 2019. https://apps.who.int/iris/handle/10665/353809
7. Overwijk WW, Tagliaferri MA, Zalevsky J. Engineering IL-2 to give new life to t-cell immunotherapy. Annu Rev Med. 2021;72(1):281-311. https://doi.org/10.1146/annurev-med-073118-011031
8. Carriedo A, Cecchini JA, Fernandez-Rio J, Méndez-Giménez A. COVID-19, psychological well-being and physical activity levels in older adults during the nationwide lockdown in Spain. Am J Geriatr Psychiatry. 2020;28(11):1146-1155. https://doi.org/10.1016/j.jagp.2020.08.007
9. O’Keefe EL, O’Keefe JH, Lavie CJ. Exercise counteracts the cardiotoxicity of psychosocial stress. Mayo Clin Proc. 2019;94(9):1852-1864. https://doi.org/10.1016/j.mayocp.2019.02.022
10. Steinmo S, Hagger-Johnson G, Shahab L. Bidirectional association between mental health and physical activity in older adults: Whitehall II prospective cohort study. Prev Med. 2014;66:74-79. https://doi.org/10.1016/j.ypmed.2014.06.005
11. Azevedo Da Silva M, Singh-Manoux A, Brunner EJ, et al. Bidirectional association between physical activity and symptoms of anxiety and depression: The Whitehall II study. Eur J Epidemiol. 2012;27(7):537-546. https://doi.org/10.1007/s10654-012-9692-8
12. Weinstein AA, Koehmstedt C, Kop WJ. Mental health consequences of exercise withdrawal: A systematic review. Gen Hosp Psychiatry. 2017;49:11-18. https://doi.org/10.1016/j.genhosppsych.2017.06.001
13. Teychenne M, White RL, Richards J, Schuch FB, Rosenbaum S, Bennie JA. Do we need physical activity guidelines for mental health: What does the evidence tell us? Ment Health Phys Act. 2020;18:100315. https://doi.org/10.1016/j.mhpa.2019.100315
14. Chekroud SR, Gueorguieva R, Zheutlin AB, et al. Physical activity and mental health – Author’s reply. Lancet Psychiatry. 2018;5(11):874. https://doi.org/10.1016/S2215-0366(18)30354-7
15. Gordon BR, McDowell CP, Lyons M, Herring MP. The effects of resistance exercise training on anxiety: A meta-analysis and meta-regression analysis of randomized controlled trials. Sports Med. 2017;47(12):2521-2532. https://doi.org/10.1007/s40279-017-0769-0
16. Gordon BR, McDowell CP, Hallgren M, Meyer JD, Lyons M, Herring MP. Association of efficacy of resistance exercise training with depressive symptoms: Meta-analysis and meta-regression analysis of randomized clinical trials. JAMA Psychiatry. 2018;75(6):566-576. https://doi.org/10.1001/jamapsychiatry.2018.0572
17. Pérez-López FR, Martínez-Domínguez SJ, Lajusticia H, Chedraui P. Effects of programmed exercise on depressive symptoms in midlife and older women: A meta-analysis of randomized controlled trials. Maturitas. 2017;106:38-47. https://doi.org/10.1016/j.maturitas.2017.09.001
18. Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, Vandelanotte C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev. 2015;9(3):366-378. https://doi.org/10.1080/17437199.2015.1022901
19. Weatherson K, Gierc M, Patte K, Qian W, Leatherdale S, Faulkner G. Complete mental health status and associations with physical activity, screen time, and sleep in youth. Ment Health Phys Act. 2020;19:100354. https://doi.org/10.1016/j.mhpa.2020.100354
20. Weatherson KA, Joopallyr H, Wunderlich K, Kwan MYW, Tomasone JR, Faulkne G. Post-secondary students’ adherence to the Canadian 24-Hour Movement Guidelines for Adults: Results from the first deployment of the Canadian Campus Wellbeing Survey (CCWS). Published June 23, 2021. https://www.canada.ca/en/public-health/services/reports-publications/health-promotion-chronic-disease-prevention-canada-research-policy-practice/vol-41-no-6-2021/post-secondary-students-24-hour-movement-guidelines-adults-canadian-campus-wellbeing-survey.h
21. Ross R, Chaput JP, Giangregorio LM, et al. Canadian 24-hour movement guidelines for adults aged 18–64 years and adults aged 65 years or older: An integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2020;45(10 (Suppl. 2)):S57-S102. https://doi.org/10.1139/apnm-2020-0467
22. Statistics Canada Government of Canada. Canadian health measures survey: Activity monitor data, 2018-2019. Published September 1, 2021. https://www150.statcan.gc.ca/n1/daily-quotidien/210901/dq210901c-eng.htm
23. Clarke J, Colley R, Janssen I, Tremblay MS. Accelerometer-measured moderate-to-vigorous physical activity of Canadian adults, 2007 to 2017. Published August 21, 2019. https://www150.statcan.gc.ca/n1/pub/82-003-x/2019008/article/00001-eng.htm
24. Chastin SFM, Craemer MD, Cocker KD, et al. How does light-intensity physical activity associate with adult cardiometabolic health and mortality? Systematic review with meta-analysis of experimental and observational studies. Br J Sports Med. 2019;53(6):370-376. https://doi.org/10.1136/bjsports-2017-097563
25. Ekelund U, Tarp J, Steene-Johannessen J, et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all-cause mortality: Systematic review and harmonised meta-analysis. BMJ. 2019;366:l4570. https://doi.org/10.1136/bmj.l4570
26. Buecker S, Simacek T, Ingwersen B, Terwiel S, Simonsmeier BA. Physical activity and subjective well-being in healthy individuals: A meta-analytic review. Health Psychol Rev. 2021;15(4):574-592. https://doi.org/10.1080/17437199.2020.1760728
27. Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID-19 international online survey. Nutrients. 2020;12(6):1583. https://doi.org/10.3390/nu12061583
28. Constandt B, Thibaut E, De Bosscher V, Scheerder J, Ricour M, Willem A. Exercising in times of lockdown: An analysis of the impact of COVID-19 on levels and patterns of exercise among adults in Belgium. Int J Environ Res Public Health. 2020;17(11):4144. https://doi.org/10.3390/ijerph17114144
29. Di Sebastiano KM, Chulak-Bozzer T, Vanderloo LM, Faulkner G. Don’t walk so close to me: Physical distancing and adult physical activity in Canada. Front Psychol. 2020;11. https://www.frontiersin.org/article/10.3389/fpsyg.2020.01895
30. Woodruff SJ, Coyne P, St-Pierre E. Stress, physical activity, and screen-related sedentary behaviour within the first month of the COVID-19 pandemic. Appl Psychol Health Well-Being. 2021;13(2):454-468. https://doi.org/10.1111/aphw.12261
31. Monitoring & tracking the field: Changes in behaviour due to the pandemic. CFLRI’S bulletin series monitoring sport and recreation in Canada; 2021. https://cflri.ca/sites/default/files/2022-03/CFLRI-TrackingTheField-Covid19-Changes-Behaviour-EN.pdf
32. Gilmour H. Self-perceived mental health and health-related behaviours of Canadians during the COVID-19 pandemic. Statistics Canada Government of Canada. Published May 12, 2020. https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00011-eng.htm
33. Meyer J, McDowell C, Lansing J, et al. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int J Environ Res Public Health. 2020;17(18):6469. https://doi.org/10.3390/ijerph17186469
34. Slimani M, Paravlic A, Mbarek F, Bragazzi NL, Tod D. The relationship between physical activity and quality of life during the confinement induced by COVID-19 outbreak: A pilot study in Tunisia. Front Psychol. 2020;11. https://www.frontiersin.org/article/10.3389/fpsyg.2020.01882
35. Bauer LL, Seiffer B, Deinhart C, et al. Associations of exercise and social support with mental health during quarantine and social-distancing measures during the COVID-19 pandemic: A cross-sectional survey in Germany. medRxiv. Published online July 2, 2020:2020.07.01.20144105.https://doi.org/10.1101/2020.07.01.20144105
36. Chouchou F, Augustini M, Caderby T, Caron N, Turpin NA, Dalleau G. The importance of sleep and physical activity on well-being during COVID-19 lockdown: Reunion island as a case study. Sleep Med. 2021;77:297-301. https://doi.org/10.1016/j.sleep.2020.09.014
37. Jacob L, Tully MA, Barnett Y, et al. The relationship between physical activity and mental health in a sample of the UK public: A cross-sectional study during the implementation of COVID-19 social distancing measures. Ment Health Phys Act. 2020;19:100345. https://doi.org/10.1016/j.mhpa.2020.100345
38. Maugeri G, Castrogiovanni P, Battaglia G, et al. The impact of physical activity on psychological health during COVID-19 pandemic in Italy. Heliyon. 2020;6(6):e04315. https://doi.org/10.1016/j.heliyon.2020.e04315
39. Deng CH, Wang JQ, Zhu LM, et al. Association of web-based physical education with mental health of college students in wuhan during the COVID-19 outbreak: Cross-sectional survey study. J Med Internet Res. 2020;22(10):e21301. https://doi.org/10.2196/21301
40. Zheng C, Huang WY, Sheridan S, Sit CHP, Chen XK, Wong SHS. COVID-19 pandemic brings a sedentary lifestyle in young adults: A cross-sectional and longitudinal study. Int J Environ Res Public Health. 2020;17(17):6035. https://doi.org/10.3390/ijerph17176035
41. Stanton R, To QG, Khalesi S, et al. Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020;17(11):4065. https://doi.org/10.3390/ijerph17114065
42. Marashi MY, Nicholson E, Ogrodnik M, Fenesi B, Heisz JJ. A mental health paradox: Mental health was both a motivator and barrier to physical activity during the COVID-19 pandemic. PLOS ONE. 2021;16(4):e0239244. https://doi.org/10.1371/journal.pone.0239244
43. Anyan F, Hjemdal O, Ernstsen L, Havnen A. Change in physical activity during the coronavirus disease 2019 lockdown in norway: The buffering effect of resilience on mental health. Front Psychol. 2020;11. https://www.frontiersin.org/article/10.3389/fpsyg.2020.598481
44. Chang YK, Hung CL, Timme S, Nosrat S, Chu CH. Exercise behavior and mood during the COVID-19 pandemic in Taiwan: Lessons for the future. Int J Environ Res Public Health. 2020;17(19):7092. https://doi.org/10.3390/ijerph17197092
45. Zach S, Zeev A, Ophir M, Eilat-Adar S. Physical activity, resilience, emotions, moods, and weight control of older adults during the COVID-19 global crisis. Eur Rev Aging Phys Act. 2021;18(1):5. https://doi.org/10.1186/s11556-021-00258-w
46. Lesser IA, Nienhuis CP. The impact of COVID-19 on physical activity behavior and well-being of Canadians. Int J Environ Res Public Health. 2020;17(11):3899. https://doi.org/10.3390/ijerph17113899
47. Schuch FB, Vancampfort D, Firth J, et al. Physical activity and incident depression: A meta-analysis of prospective cohort studies. Am J Psychiatry. 2018;175(7):631-648. https://doi.org/10.1176/appi.ajp.2018.17111194
48. Fornili M, Petri D, Berrocal C, et al. Psychological distress in the academic population and its association with socio-demographic and lifestyle characteristics during COVID-19 pandemic lockdown: Results from a large multicenter Italian study. PLOS ONE. 2021;16(3):e0248370. https://doi.org/10.1371/journal.pone.0248370
49. Wolf S, Seiffer B, Zeibig JM, et al. Is physical activity associated with less depression and anxiety during the COVID-19 pandemic? A rapid systematic review. Sports Med. 2021;51(8):1771-1783. https://doi.org/10.1007/s40279-021-01468-z
50. Runacres A, Mackintosh KA, Knight RL, et al. Impact of the COVID-19 pandemic on sedentary time and behaviour in children and adults: A systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18(21):11286. https://doi.org/10.3390/ijerph182111286
51. Carroll N, Sadowski A, Laila A, et al. The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income canadian families with young children. Nutrients. 2020;12(8):2352. https://doi.org/10.3390/nu12082352
52. McCormack GR, Doyle-Baker PK, Petersen JA, Ghoneim D. Parent anxiety and perceptions of their child’s physical activity and sedentary behaviour during the COVID-19 pandemic in Canada. Prev Med Rep. 2020;20:101275. https://doi.org/10.1016/j.pmedr.2020.101275
53. Mitra R, Moore SA, Gillespie M, et al. Healthy movement behaviours in children and youth during the COVID-19 pandemic: Exploring the role of the neighbourhood environment. Health Place. 2020;65:102418. https://doi.org/10.1016/j.healthplace.2020.102418
54. Moore SA, Faulkner G, Rhodes RE, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: A national survey. Int J Behav Nutr Phys Act. 2020;17(1):85. https://doi.org/10.1186/s12966-020-00987-8
55. Zajacova A, Jehn A, Stackhouse M, Denice P, Ramos H. Changes in health behaviours during early COVID-19 and socio-demographic disparities: A cross-sectional analysis. Can J Public Health. 2020;111(6):953-962. https://doi.org/10.17269/s41997-020-00434-y
56. Perez EC, Bravo DR, Rodgers SP, Khan AR, Leasure JL. Shaping the adult brain with exercise during development: Emerging evidence and knowledge gaps. Int J Dev Neurosci. 2019;78:147-155. https://doi.org/10.1016/j.ijdevneu.2019.06.006
57. Lubans D, Richards J, Hillman C, et al. Physical activity for cognitive and mental health in youth: A systematic review of mechanisms. Pediatrics. 2016;138(3):e20161642. https://doi.org/10.1542/peds.2016-1642
58. Rhodes RE, Spence JC, Berry T, et al. Parental support of the Canadian 24-hour movement guidelines for children and youth: Prevalence and correlates. BMC Public Health. 2019;19(1):1385. https://doi.org/10.1186/s12889-019-7744-7
59. Goethals L, Barth N, Guyot J, Hupin D, Celarier T, Bongue B. Impact of home quarantine on physical activity among older adults living at home during the COVID-19 pandemic: Qualitative interview study. JMIR Aging. 2020;3(1):e19007. https://doi.org/10.2196/19007
60. Moore SA, Faulkner G, Rhodes RE, et al. Few Canadian children and youth were meeting the 24-hour movement behaviour guidelines 6-months into the COVID-19 pandemic: Follow-up from a national study. Appl Physiol Nutr Metab. 2021;46(10):1225-1240. https://doi.org/10.1139/apnm-2021-0354
61. Riazi NA, Wunderlich K, Gierc M, et al. “You can’t go to the park, you can’t go here, you can’t go there”: Exploring parental experiences of COVID-19 and its impact on their children’s movement behaviours. Children. 2021;8(3):219. https://doi.org/10.3390/children8030219
62. Toombs E, Mushquash CJ, Mah L, et al. Increased screen time for children and youth during the COVID-19 pandemic. Sci Briefs Ont COVID-19 Sci Advis Table. 2022;3(59). https://doi.org/10.47326/ocsat.2022.03.59.1.0
63. Allesøe K, Lau CJ, Buhelt LP, Aadahl M. Physical activity, self-rated fitness and stress among 55,185 men and women in the Danish Capital Region Health survey 2017. Prev Med Rep. 2021;22:101373. https://doi.org/10.1016/j.pmedr.2021.101373
64. Rogowska AM, Pavlova I, Kuśnierz C, Ochnik D, Bodnar I, Petrytsa P. Does physical activity matter for the mental health of university students during the COVID-19 pandemic? J Clin Med. 2020;9(11):3494. https://doi.org/10.3390/jcm9113494
65. Lotoski L, Fuller D, Stanley KG, Rainham D, Muhajarine N. The effect of season and neighbourhood-built environment on home area sedentary behaviour in 9-14 year old children. Int J Environ Res Public Health. 2021;18(4):1968. https://doi.org/10.3390/ijerph18041968
66. Nagata JM, Cortez CA, Dooley EE, Iyer P, Ganson KT, Pettee Gabriel K. Moderate-to-vigorous intensity physical activity among adolescents in the USA during the COVID-19 pandemic. Prev Med Rep. 2022;25:101685. https://doi.org/10.1016/j.pmedr.2021.101685
67. Rollo S, Roberts KC, Bang F, et al. Sociodemographic factors associated with meeting the Canadian 24-hour movement guidelines among adults: Findings from the Canadian health measures survey. J Phys Act Health. 2022;19(3):194-202. https://doi.org/10.1123/jpah.2021-0542
68. Statistics Canada Government of Canada. Table 3: Percentage of adults meeting the Canadian physical activity guidelines (≥150 minutes per week of MVPAbouts), by Canadian health measures survey cycle, sex and age group, household population aged 18 to 79 years, Canada, 2007 to 2017. Published August 21, 2019. https://www150.statcan.gc.ca/n1/pub/82-003-x/2019008/article/00001/tbl/tbl03-eng.htm
69. Leigh JP, Brundin-Mather R, Soo A, et al. Public perceptions during the first wave of the COVID-19 pandemic in Canada: A demographic analysis of self-reported beliefs, behaviors, and information acquisition. BMC Public Health. 2022;22(1):699. https://doi.org/10.1186/s12889-022-13058-3
70. Alon T, Doepke M, Olmstead-Rumsey J, Tertilt M. This time it’s different: The role of women’s employment in a pandemic recession. Published online August 2020. https://doi.org/10.3386/w27660
71. Social isolation amongst older adults during the pandemic. Government of Canada. http://www12.esdc.gc.ca/sgpe-pmps/h.4m.2@-eng.jsp?utm_campaign=not-applicable&utm_medium=vanity-url&utm_source=canada-ca_publicentre-esdc
72. Frieden TR. A framework for public health action: The health impact pyramid. Am J Public Health. 2010;100(4):590-595. https://doi.org/10.2105/AJPH.2009.185652
73. CDC. Overcoming barriers to physical activity. Centers for Disease Control and Prevention. Published June 3, 2022. https://www.cdc.gov/physicalactivity/basics/adding-pa/barriers.html
74. Guy F, Lira Y, Mark S. T, John C. S. Exploring the impact of the ‘new’ ParticipACTION: Overview and introduction of the special issue. Health Promot Chronic Dis Prev Can Res Policy Pract. 2018;38(4):153-161. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5983879/
75. Dozois DJA. Anxiety and depression in Canada during the COVID-19 pandemic: A national survey. Can Psychol Can. 2021;62(1):136-142. https://doi.org/10.1037/cap0000251
76. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912-920. https://doi.org/10.1016/S0140-6736(20)30460-8
77. Ekkekakis P, Hall EE, VanLanduyt LM, Petruzzello SJ. Walking in (affective) circles: Can short walks enhance affect? J Behav Med. 2000;23(3):245-275. https://doi.org/10.1023/A:1005558025163
78. Werneck AO, Oyeyemi AL, Silva DR. Physical activity and depression: Is 150 min/week of moderate to vigorous physical activity a necessary threshold for decreasing risk of depression in adults? Different views from the same data. Soc Psychiatry Psychiatr Epidemiol. 2018;53(3):323-324. https://doi.org/10.1007/s00127-018-1490-5
79. Arena R, Lavie CJ. Moving more and sitting less – Now more than ever-an important message for the prevention and treatment of chronic disease and pandemics. Prog Cardiovasc Dis. 2021;64:1-2. https://doi.org/10.1016/j.pcad.2020.10.001
80. CBC News. Nature is healing: Doctors in B.C., other provinces can prescribe Parks Canada passes to patients. CBC. Published February 9, 2022. https://www.cbc.ca/news/canada/british-columbia/bc-parks-canada-prescription-1.6344141
81. Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: A position statement of the American diabetes association. Diabetes Care. 2016;39(11):2065-2079. https://doi.org/10.2337/dc16-1728
82. Bland KA, Bigaran A, Campbell KL, Trevaskis M, Zopf EM. Exercising in isolation? The role of telehealth in exercise oncology during the COVID-19 pandemic and beyond. Phys Ther. 2020;100(10):1713-1716. https://doi.org/10.1093/ptj/pzaa141
83. Marzolini S, Ghisi GL de M, Hébert AA, Ahden S, Oh P. Cardiac rehabilitation in canada during COVID-19. CJC Open. 2021;3(2):152-158. https://doi.org/10.1016/j.cjco.2020.09.021
84. Yarnall KSH, Pollak KI, Østbye T, Krause KM, Michener JL. Primary care: Is there enough time for prevention? Am J Public Health. 2003;93(4):635-641. https://doi.org/10.2105/AJPH.93.4.635
85. Zachary Z, Brianna F, Brianna L, et al. Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obes Res Clin Pract. 2020;14(3):210-216. https://doi.org/10.1016/j.orcp.2020.05.004
86. Thompson Coon J, Boddy K, Stein K, Whear R, Barton J, Depledge MH. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental well-being than physical activity indoors? A systematic review. Environ Sci Technol. 2011;45(5):1761-1772. https://doi.org/10.1021/es102947t
87. WHO Regional Office for Europe. Urban Green Spaces and Health: A Review of Evidence.; 2016. https://apps.who.int/iris/bitstream/handle/10665/345751/WHO-EURO-2016-3352-43111-60341-eng.pdf?sequence=1&isAllowed=y
88. Storgaard RL, Hansen HS, Aadahl M, Glümer C. Association between neighbourhood green space and sedentary leisure time in a Danish population. Scand J Public Health. 2013;41(8):846-852. https://doi.org/10.1177/1403494813499459
89. Barton J, Rogerson M. The importance of green space for mental health. BJPsych Int. 2017;14(4):79-81. https://doi.org/10.1192/S2056474000002051
90. Kardan O, Gozdyra P, Misic B, et al. Neighborhood green space and health in a large urban center. Sci Rep. 2015;5(1):11610. https://doi.org/10.1038/srep11610
91. Richardson EA, Pearce J, Mitchell R, Kingham S. Role of physical activity in the relationship between urban green space and health. Public Health. 2013;127(4):318-324. https://doi.org/10.1016/j.puhe.2013.01.004
92. Zhang R, Zhang CQ, Rhodes RE. The pathways linking objectively-measured green space exposure and mental health: A systematic review of observational studies. Environ Res. 2021;198:111233. https://doi.org/10.1016/j.envres.2021.111233
93. Toronto Public Health. Green City: Why Nature Matters to Health – an Evidence Review.; 2015:37. https://www.toronto.ca/legdocs/mmis/2015/hl/bgrd/backgroundfile-83421.pdf
94. Greene CS, Robinson PJ, Millward AA. Canopy of advantage: Who benefits most from city trees? J Environ Manage. 2018;208:24-35. https://doi.org/10.1016/j.jenvman.2017.12.015
95. Doiron D, Setton EM, Shairsingh K, et al. Healthy built environment: Spatial patterns and relationships of multiple exposures and deprivation in Toronto, Montreal and Vancouver. Environ Int. 2020;143:106003. https://doi.org/10.1016/j.envint.2020.106003
96. Carver H, Parkes T, Masterton W. Parks and green spaces are important for our mental health – but we need to make sure that everyone can benefit. The Conversation. http://theconversation.com/parks-and-green-spaces-are-important-for-our-mental-health-but-we-need-to-make-sure-that-everyone-can-benefit-142322
97. CDC. The built environment assessment tool manual. Published August 26, 2021. https://www.cdc.gov/nccdphp/dnpao/state-local-programs/built-environment-assessment/index.htm
98. Roof K, Oleru N. Public health: Seattle and King County’s push for the built environment. J Environ Health. 2008;71(1):24-27. https://pubmed.ncbi.nlm.nih.gov/18724501/
99. Russo A, Cirella GT. Modern compact cities: How much greenery do we need? Int J Environ Res Public Health. 2018;15(10):2180. https://doi.org/10.3390/ijerph15102180
100. Smith M, Hosking J, Woodward A, et al. Systematic literature review of built environment effects on physical activity and active transport – an update and new findings on health equity. Int J Behav Nutr Phys Act. 2017;14(1):158. https://doi.org/10.1186/s12966-017-0613-9
101. Health Equity and Community Design: What Is the Canadian Evidence Saying? https://www.cip-icu.ca/Files/Resources/FACTSHEETS-Equity-FINALenglish.aspx
102. HEALTH EQUITY AND ENVIRONMENTAL PUBLIC HEALTH (EPH). Fact sheet: Supporting health equity through the built environment. http://www.bccdc.ca/resource-gallery/Documents/Educational%20Materials/EH/BCCDC_equity-fact-sheet_web.pdf
103. Pineo H, Zimmermann N, Davies M. Integrating health into the complex urban planning policy and decision-making context: A systems thinking analysis. Palgrave Commun. 2020;6(1):1-14. https://doi.org/10.1057/s41599-020-0398-3
104. Schoner J, Chapman J, Brookes A, et al. Bringing health into transportation and land use scenario planning: Creating a National Public Health Assessment Model (N-PHAM). J Transp Health. 2018;10:401-418. https://doi.org/10.1016/j.jth.2018.04.008
105. Mukhtar M. An objective walkability index for public health and planning in Peel Region, Ontario, Canada. Prev Chronic Dis. 2019;16. https://doi.org/10.5888/pcd16.180469
106. de Lannoy L, Rhodes RE, Moore SA, Faulkner G, Tremblay MS. Regional differences in access to the outdoors and outdoor play of Canadian children and youth during the COVID-19 outbreak. Can J Public Health. 2020;111(6):988-994. https://doi.org/10.17269/s41997-020-00412-4
107. Gardner B, Smith L, Lorencatto F, Hamer M, Biddle SJ. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol Rev. 2016;10(1):89-112. https://doi.org/10.1080/17437199.2015.1082146
Document Information & Citation
Author Contributions: LM conceived the Science Brief. CT, LM and LZ wrote the first draft of the Science Brief. LM and KB led subsequent revisions to the Science Brief. All authors revised the Science Brief critically for important intellectual content and approved the final version.
The authors would like to thank James Dunn, Christine Bushey, Sherry Diaz, Lisa Simon and Loren Vanderlinden for their comments and review of this Science Brief.
Citation: Tao CS, Zhu L, Strudwick G, et al. The impact of physical activity on mental health outcomes during the COVID-19 pandemic. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2022;3(62). https://doi.org/10.47326/ocsat.2022.03.62.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners can be found at https://covid19-sciencetable.ca/. The declarations of interest of external authors can be found under Additional Resources.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners.
