Key Message
The post COVID-19 condition is a complex and heterogeneous syndrome that develops in people with prior SARS-CoV-2 infection. More than 100 symptoms have been reported in people with the post COVID-19 condition, and these appear to be associated with reduced quality of life, reduced function, and impairments in people’s ability to work and care for themselves. There remains significant uncertainty in the definition, magnitude of prevalence, causes, risk factors, prevention, and prognosis of the post COVID-19 condition, as well as its impact on people’s quality of life, function, and ability to work. Nonetheless, the reported range of these effects in the published literature suggests that the post COVID-19 condition poses substantial health risks to adults across a diverse range of outcomes that have the potential to impart a considerable burden on individuals and healthcare systems. More contemporary evidence in the era of widespread vaccination and emerging variants resulting in less severe illness than earlier variants suggests that the post COVID-19 condition may now be less frequent following SARS-CoV-2 infection. Still, a proactive and comprehensive strategy to manage the post COVID-19 condition needs to be developed by health systems and policy makers. This strategy should include substantial investments in research and health system resources to mitigate the long-term health, social, and economic impacts of the post COVID-19 condition in Ontario.
Summary
Background
The post COVID-19 condition is a complex and heterogeneous syndrome that can develop in people with prior SARS-CoV-2 infection. The goal of this Science Brief is to identify and support the healthcare care needs of adults living with the post COVID-19 condition and their caregivers, and to inform health system and social resource planning to be able to meet those needs.
Questions
How has the post COVID-19 condition been defined?
What are the potential underlying causes of the post COVID-19 condition?
What is the prevalence of the post COVID-19 condition?
What are the symptoms and sequelae of the post COVID-19 condition?
Who is at risk of developing the post COVID-19 condition, and can this risk be mitigated?
What is the impact of the post COVID-19 condition on functional limitations, health system utilization, and utilization of long-term disability and unemployment benefits?
How are healthcare systems delivering care to people with the post COVID-19 condition?
What barriers exist to providing clinical support to those with the post COVID-19 condition?
What are the current knowledge gaps about the post COVID-19 condition?
Findings
The post COVID-19 condition is variably defined as the persistence of symptoms or sequelae occurring at least 4 or 12 weeks after probable or confirmed SARS-CoV-2 infection. Combined evidence estimates the prevalence of new or persistent symptoms at 4 or more weeks from SARS-CoV-2 infection to be 43% (54% among hospitalized persons, including those admitted to the intensive care unit, and 34% among those who are not hospitalized) and between 10-20% at 12 or more weeks, depending on the definition and data used to inform those estimates. Data from more recent pandemic time periods suggests a much lower overall prevalence. The five most frequently observed individual symptoms were fatigue (23%, 95% confidence interval (CI) 17-30), memory deficits (14%, 95% CI 10-19), shortness of breath (13%, 95% CI 0.11-0.15), sleep problems (11%, 95% CI 5-23), and joint pain (10%, 95% CI 4-22). The systemic nature of the condition is believed to be related to viral persistence, inflammation, autoimmunity, and/or coagulopathy. More than 100 symptoms have been reported in people with the post COVID-19 condition, and these appear to be associated with reduced function, impairments in people’s ability to work and care for themselves, poor quality of life, and high healthcare use. Vaccination against COVID-19 with one or two doses of vaccine prior to SARS-CoV-2 infection was associated with a reduction of approximately 50% in the risk of developing lingering symptoms at either time point. The benefits of vaccination in reducing the development of the post COVID-19 condition were also observed in people who were vaccinated after SARS-CoV-2 infection, as well as potentially in those with established post COVID–19 condition. High-quality care for people with the post COVID-19 condition is limited by a lack of proven therapies, potential inequities in care that are driven by limited access to primary and specialized care, and inconsistent application of insurance policies for reimbursement. There is also variable use of and lack of diagnostic and physician fee codes to track and evaluate care delivery and outcomes at a population level.
Interpretation
The post COVID-19 condition poses substantial health risks across a diverse range of outcomes that may result in a considerable burden for Ontarians, the economy, and the healthcare system. More contemporary evidence in the era of widespread vaccination and emerging variants resulting in less severe illness than earlier variants suggests that the post COVID-19 condition may now be less frequent following SARS-CoV-2 infection. Due to limitations in the quality of available published evidence, however, there remains significant uncertainty in the definition, prevalence, causes, risk factors, prevention, and prognosis of the post COVID-19 condition, as well as its impact on people’s quality of life, function, and ability to work. There is also considerable uncertainty about the magnitude of these potential effects. Nonetheless, a proactive and comprehensive strategy to manage the post COVID-19 condition needs to be developed by health systems and policymakers. This strategy should include substantial investments in research and health system resources to mitigate the long-term health, social, and economic impacts of the post COVID-19 condition in Ontario.
Full Text
Background
Globally, there have been more than 500 million SARS-CoV-2 infections to date.1 Early in the pandemic, a substantial burden of symptoms and sequelae were noted to persist for months after the resolution of the acute COVID-19 illness. Advocacy groups initially referred to this syndrome as “long COVID”, which has since been described using several other terms. For the purposes of this Science Brief, the term “post COVID-19 condition” will be used.
This Science Brief draws on a comprehensive review of existing literature to characterize the expected burden of the post COVID-19 condition for adults in Ontario since there appears to be a substantial risk of negative health outcomes associated with it. However, there remains significant uncertainty in the definition, prevalence, causes, risk factors, prevention, and prognosis of the post COVID-19 condition, and its impact on healthcare systems and society due to limitations in the quality of available published evidence. There is also considerable uncertainty about the magnitude of its potential effects.
This work is an update of our 2021 Science Brief entitled: “Understanding the Post COVID-19 Condition (Long COVID) and the Expected Burden for Ontario”.2 It does not review the evidence for the post COVID-19 condition in children as children manifest disease in distinct ways with often distinct mechanisms. Every attempt has been made to acknowledge the uncertainty in the spectrum of risks associated with the post COVID-19 condition throughout the Science Brief. The goal of this Science Brief is to support the healthcare care needs of people living with the post COVID-19 condition and their caregivers, and to inform health system resource planning to meet those needs.
Questions
How has the post COVID-19 condition been defined?
What are the potential underlying causes of the post COVID-19 condition?
What is the prevalence of the post COVID-19 condition?
What are the symptoms and sequelae of the post COVID-19 condition?
Who is at risk of developing the post COVID-19 condition, and can this risk be mitigated?
What is the impact of the post COVID-19 condition on functional limitations, health system utilization, and utilization of long-term disability and unemployment benefits?
How are healthcare systems delivering care to people with the post COVID-19 condition?
What barriers exist to providing clinical support to those with the post COVID-19 condition?
What are the current knowledge gaps about the post COVID-19 condition?
Findings
Defining the Post COVID-19 Condition
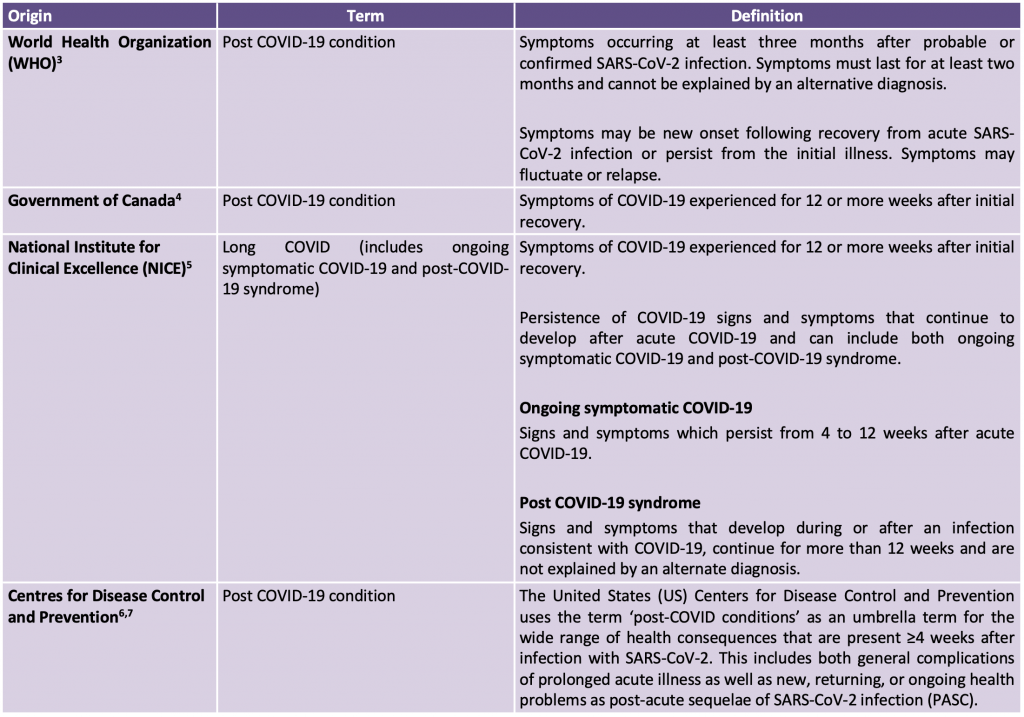
The post COVID-19 condition encompasses a range of symptoms and sequelae that arise following acute SARS-CoV-2 infection. This heterogeneity poses considerable challenges in attempting to create a definition that encompasses the spectrum of symptoms and sequelae associated with the post COVID-19 condition. As a result, numerous clinical definitions for this condition have been proposed (Table 1). Some definitions define it as the attributable effects of the post COVID-19 condition related exclusively to symptoms beyond 12 weeks, while others define it as the attributable effects related to symptoms in addition to the development of new, returning, or ongoing health problems as post-acute sequelae of SARS-CoV-2 infection beyond four weeks. The establishment of a globally accepted definition of the post COVID-19 condition is critical to its diagnosis and treatment in clinical practice, to effective tracking and evaluation of care at a health systems level, and to further study its expected burden for the purposes of health resource planning, disability and unemployment benefits, and social services. To date, there is still no universally accepted definition of the post COVID-19 condition. In this Brief, we report the evidence across all definitions to provide a comprehensive overview of the potential risks associated with the post COVID-19 condition and simultaneously recognize the uncertainty of these reported risks created by using various definitions in the published literature.
The Post COVID-19 Condition: A New Disease Framework and Potential Underlying Causes
The systemic manifestations of the post COVID-19 condition are believed to be related primarily to the expression of the angiotensin-converting enzyme 2 (ACE2) receptor in multiple organ systems, through which SARS-CoV-2 enters the cell.8 Emerging evidence suggests that a combination of viral and host factors may bridge the pathophysiologic mechanisms linking SARS-CoV-2 infection to direct cellular and organ damage with the development of the post COVID-19 condition. These viral-dependent and viral-independent mechanisms have been categorized to include the following major domains: 1) viral persistence; 2) persistent inflammation; 3) autoimmunity; and 4) coagulopathy.8–11 Their mechanisms include ongoing cellular damage, tissue hypoxia (lack of oxygen), perivascular inflammation, inflammatory cytokine production (e.g., IL-6, IL-1β, and TNF-ɑ) following robust immune activation, a maladaptive autoimmune response leading to the production of autoantibodies directed against self-tissue antigens that persist after the virus has been eliminated, and increased tendency to develop blood clots leading to microvascular coagulopathy.8–10 How long this tendency to develop blood clots is sustained and its relevance specifically to the development of the post COVID-19 condition remains unclear.8 Recent evidence also suggests a possible link between Epstein-Barr virus (EBV) reactivation and the development of the post COVID-19 condition, which is similar to other conditions such as myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).12 However, it remains possible that EBV viremia resulting from reactivation may be a consequence of the severity of initial COVID-19 rather than represent a direct causal mechanism.13
Emerging research has helped illuminate potential mechanisms that may explain some of the neurocognitive manifestations of the post COVID-19 condition. The UK BioBank studied 785 sets of brain scans (an average of three years apart) from people before and after the onset of the COVID-19 pandemic. Among these participants, 51% (n=401) were infected with SARS-CoV-2 (most displaying mild to moderate severity of symptoms) and 49% (n=384) were not. Those who were infected demonstrated loss of cortical thickness and diffuse atrophy in certain areas of the brain (often associated with worsening brain health), and increased tissue damage in the regions of the brain responsible for smell and taste. Further, infected participants also demonstrated greater cognitive decline compared to those who were not infected with SARS-CoV-2.14 A prospective observational cohort study of individuals with polymerase chain reaction (PCR) confirmed SARS-CoV-2 infection and mild COVID-19 presentation examined neurological impairment four months after infection using neuropsychological, ocular, and neurological tests, immune marker assays, structural magnetic resonance imaging (MRI), and 18FDG-PET neuroimaging.15 In approximately 25% of individuals, a specific vasoconstrictive deficit (atypical difficulty in using visual and spatial information to guide complex behaviours) was detected, which was associated with changes in molecular and structural brain imaging as well as correlation with upregulation of peripheral immune markers.
Research has also attempted to characterize the post COVID-19 condition using biomarkers. A preliminary study of 63 people with PCR-confirmed SARS-CoV-2 infection detected the SARS-CoV-2 spike antigen from the serum of 65% of those with the post COVID-19 condition up to 12 months later, whereas spike protein was not detected in people without the post COVID-19 condition.16 A separate study examined specific T cell responses in a cohort of seronegative, mostly non-hospitalized people with PCR-confirmed COVID-19 and/or the post COVID-19 condition.17 Overall, 42-53% of people with the post COVID-19 condition were found to lack SARS-CoV-2 antibodies but nonetheless had detectable SARS-CoV-2-specific T cell responses. Release of a cytokine known as interleukin-2 by T cells (but not interferon-γ release) was found to be both sensitive (75%, SD=13) and specific (88%, SD=7) for previous SARS-CoV-2 infection more than 6 months after a positive PCR test. These findings may have important implications for disability claims where there is a lack of prior testing for SARS-CoV-2 infection. Further research is needed to confirm the reliability of these biomarkers.
There remain challenges in disentangling the general effects of any acute or critical illness from the direct effects of SARS-CoV-2 infection in driving the diverse range of health outcomes and potential pathophysiological mechanisms thought to be part of the post COVID-19 condition. People with COVID-19 and critical illness develop severe long-term complications related to the post-acute respiratory distress syndrome (ARDS), post-sepsis syndrome, and sequelae of chronic critical illness. The post-intensive care syndrome (PICS) is also a well-recognized condition with known new or worsening abnormalities in physical, cognitive, and psychiatric domains after critical illness and ARDS that can persist for five or more years after the initial illness.9,10,18 PICS is observed in all critical illnesses requiring hospital care and is likely related to the effects of factors such as prolonged hospitalization, limited mobility, and/or mechanical ventilation. New research approaches are needed to distinguish clinical phenotypes among people with the post COVID-19 condition across a spectrum of illness severity, and to determine to what extent these are due to PICS. This will have implications for the evaluation of multidisciplinary longitudinal interventions and for advancing the care of this condition.
Taken together, there are multiple underlying mechanisms that contribute to development of the post COVID-19 condition, although it remains unclear which specific mechanisms are responsible for the diverse range of symptoms among people with the condition.
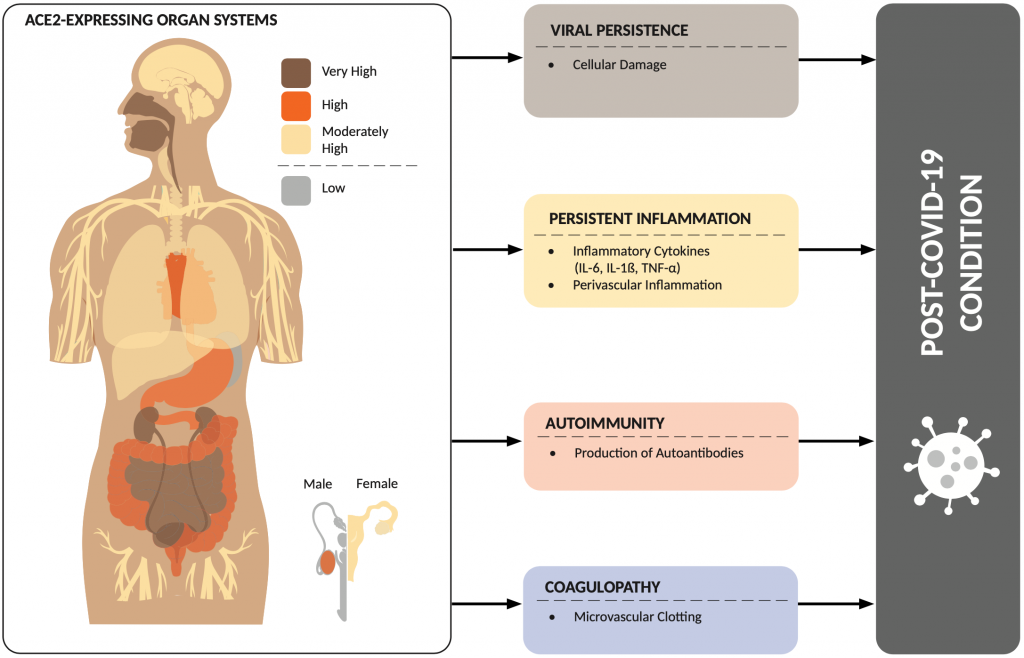
The SARS-CoV-2 virus enters the cell through angiotensin-converting enzyme 2 (ACE2) receptor, which is widely expressed in multiple organ systems and may explain the diverse range of symptoms experienced by those with the post COVID-19 condition. A combination of viral-dependent and viral-independent mechanisms leading to development of the post COVID-19 condition include: 1) viral persistence; 2) persistent inflammation; 3) autoimmunity; and 4) coagulopathy.
Prevalence of the Post COVID-19 Condition
The reported prevalence of the post COVID-19 condition varies widely, which creates significant uncertainty in arriving at a true estimate of how common the condition may be. Perhaps most importantly, it is essential to know the underlying prevalence of symptoms such as fatigue and shortness of breath that comprise the post COVID-19 condition in people who lived through the pandemic and who were not infected with SARS-CoV-2. The “true” prevalence of the condition could then be estimated using analytical strategies to compare nearly identical people at nearly identical points in time who were and were not infected during the pandemic, including whether they required any type of hospitalization during these study periods. To date, very few of these appropriate comparator studies have been published, which has led to reporting of wider ranges of its prevalence.
Following the release of their clinical case definition, the WHO estimated that 10 to 20% of all people with SARS-CoV-2 infection in the early periods of the pandemic would develop the post COVID-19 condition — symptoms occurring three or more months after acute infection that last for at least two months and are not explained by an alternative condition.3,19 Using more contemporary data among adults who were triple vaccinated, 4.5%, 4.2%, and 5.0% of people self-reported having symptoms of the post COVID-19 condition beyond 12 weeks after confirmed SARS-CoV-2 infection compatible with the Omicron BA.1, Omicron BA.2 or Delta variants, respectively.20 In double vaccinated adults, 4.0% of people self-reported having symptoms of the post COVID-19 condition after confirmed SARS-CoV-2 infection for the Omicron BA.1 variant, compared with 9.2% for the Delta variant.20 These findings were supported by a recent systematic review of 9 studies that examined the prevalence of the post COVID-19 condition following SARS-CoV-2 infection in non-hospitalized people, which reported a prevalence estimate ranging from 10-35%.21
Using the CDC definition, the findings of a systematic review of 886,388 confirmed SARS-CoV-2 cases across 29 studies early in the pandemic estimated a global pooled prevalence of new or persistent symptoms at four or more weeks from infection of 43% (54% among hospitalized and 34% among non-hospitalized people).22Examining this through the lens of overall population impact, the United Kingdom (UK) Office for National Statistics (ONS) reported that symptoms persisting for four or more weeks after suspected SARS-CoV-2 infection were present in 2.8% of the 64 million people living in private households in the UK,23 which was based on weighted survey data from a population-representative sample.
It is challenging to provide precise prevalence estimates of the post COVID-19 condition given the varying definitions used to inform these estimates in the published literature (Table 1). Further heterogeneity is related to other important factors that impact prevalence estimates across studies including: 1) severity of initial infection (ranging from asymptomatic to critical illness); 2) duration of follow-up used to measure outcomes; 3) bias in recruitment, including sampling strategy (e.g., population-based versus self-reporting via an app); 4) study sample size; 5) eligibility criteria for enrolment (e.g., positive COVID-19 test versus plausible symptoms with an epidemiologic-link) and its relation to evolving health system capacity for SARS-CoV-2 testing during respective waves; 6) the episodic nature of symptoms for some individuals; 7) the impact of emerging therapeutics and viral variants on the development of the post COVID-19 condition; 8) COVID-19 vaccination status; and 9) eligibility and access to SARS-CoV-2 tests (PCR and rapid antigen tests). In addition, many of the more severe persistent symptoms reported among the subset who were hospitalized may be related to general findings in people with a critical illness (e.g., individuals with PICS).
Current evidence suggests that with a 12-week criterion for symptoms, the post COVID-19 condition likely affects between approximately 2 and 10% of vaccinated persons infected with contemporary variants, but more research is required to confirm these estimates.
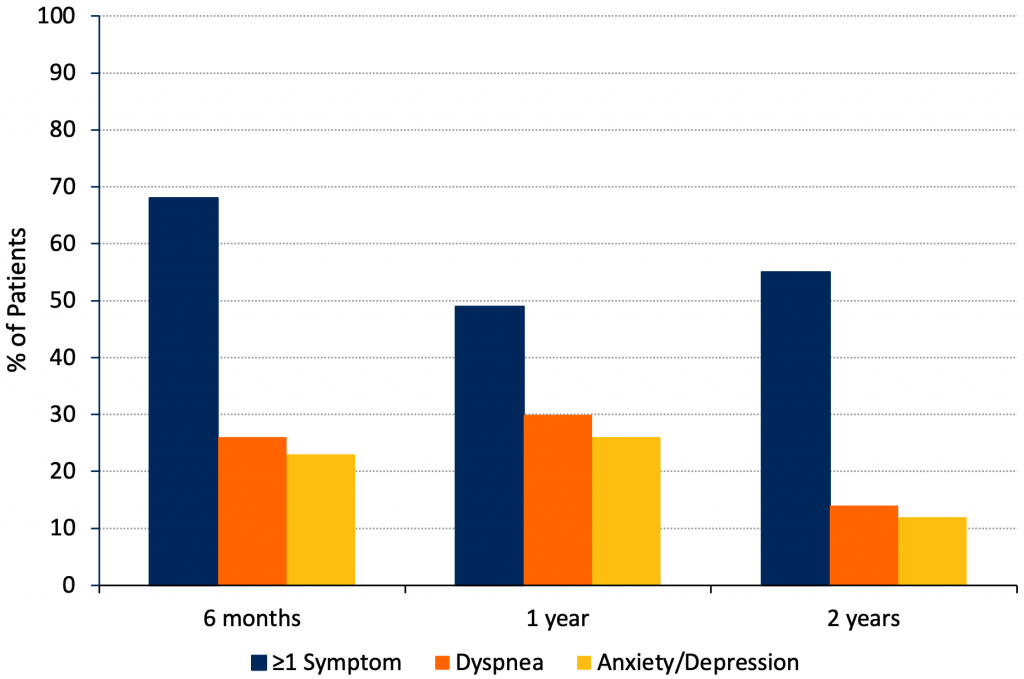
Control Comparisons
Few studies on the post COVID-19 condition used comparative control groups to measure the prevalence of symptoms attributable to SARS-CoV-2 infection, its impact on quality of life, and health services use.24 This is perhaps one of the most significant limitations in our ability to accurately estimate the true prevalence of the post COVID-19 condition. The study with the longest follow-up period to date included a cohort of 1,192 hospitalized people with COVID-19 in Wuhan, China, who were matched on age, sex, and comorbidities to controls without COVID-19.25 At two years follow-up, 65% of people with prior COVID-19 experienced one or more of 15 identified symptoms of the post COVID-19 condition, compared to 32% of controls. The reasons for the high prevalence of symptoms in controls are unclear, which may be related to the lasting effects of the pandemic on people’s health or other influencing factors. The proportion of people with prior COVID-19 with at least one or more symptoms decreased significantly from 68% at six months follow-up to 55% at two years. A significantly greater proportion of COVID-19 survivors experienced a reduced quality of life-related to increased pain or discomfort compared with controls, as well as anxiety or depression and problems with usual activities.
A limited number of studies compared prevalence estimates of the post COVID-19 condition in both people with the condition and control groups without it. A retrospective matched cohort study examined 486,149 adults with confirmed SARS-CoV-2 infection and 1,944,580 propensity-score matched controls without COVID-19.26Of the 384,137 infected people and 1,501,689 controls with a minimum of 12 weeks follow-up, 5.4% of infected people and 4.3% of controls reported at least one symptom of the post COVID 19 condition according to the WHO case definition (from a list of over possible 100 symptoms). An observational cohort study used data collected from a larger population-based cohort study in the Netherlands to estimate the prevalence of the post COVID-19 condition among people with prior SARS-CoV-2 infection compared to controls.27 In 4,321 participants with confirmed SARS-CoV-2 infection and 8,462 matched controls without COVID-19 (matched by age, sex, and time), 21.4% of participants with confirmed SARS-CoV-2 infection experienced at least one symptom of the post COVID-19 condition compared to 8.7% of controls at 90-150 days follow-up (symptoms included chest pain, difficulties with breathing, pain when breathing, painful muscles, loss of taste or smell, tingling extremities, lump in throat, feeling hot and cold alternately, heavy arms or legs, and general tiredness). The Alpha variant was dominant during the study period. At the start of the study period, 3.8% of the sample had two doses of COVID-19 vaccines, which increased to 9.8% at the end of the study when the final participants were included.
Overall, these findings suggest an increase in the prevalence of symptoms of the post COVID-19 condition in people who had SARS-CoV-2 infection compared to controls, although the true magnitude of these estimates remains uncertain.
Incidence of the Post COVID-19 Condition Following Infection with Different Variants of Concern
Few studies compared the incidence of the post COVID-19 condition for different variants of concern (VOC).28A case-control observational study of 56,003 UK adults who tested positive for SARS-CoV-2 infection examined the relative odds of having the post COVID-19 condition related to Omicron compared to Delta.29Among Omicron cases, 4.5% (n=2,501) experienced the post COVID-19 condition compared to 10.8% (n=4,469) infected with Delta. Overall, people infected with Omicron were less likely to experience the post COVID-19 condition compared to those infected with Delta (odds ratio (OR) 0.24 (95% CI 0.20-0.32) to 0.50 (95% CI 0.43-0.59), which also depended on the age of the person and timing of their vaccination relative to their infection. For example, the benefits of vaccination were more pronounced in people who were vaccinated more than three months before SARS-CoV-2 infection, compared to those who were vaccinated within three months of infection. A similar study from the Office of National Statistics, which used survey data from a population-representative sample, reported that there was no statistical evidence of a difference in risk between first infections with Omicron BA.1 or BA.2 variants compared with Delta among triple-vaccinated adults after adjustment for socio-demographic characteristics and time since last vaccine dose.20 However, among adults who were double vaccinated, the odds of reporting symptoms of the post COVID-19 condition after confirmed SARS-CoV-2 infection consistent with the Omicron variant were 48.2% lower than for infections with the Delta variant after adjustment for socio-demographic characteristics.
Based on the very limited number and nature of the available studies, currently it appears that the risk of developing the post COVID-19 condition after SARS-CoV-2 infection is lower with the Omicron variant compared to the Delta variant.
Vaccination and the Post COVID-19 Condition
The Public Health Agency of Canada (PHAC) and the UK Health Security Agency (UKHSA) recently reviewed the evidence examining the effects of vaccination on the post COVID-19 condition among previously unvaccinated people prior to as well as after SARS-CoV-2 infection and among those with established post COVID-19 condition.30,31
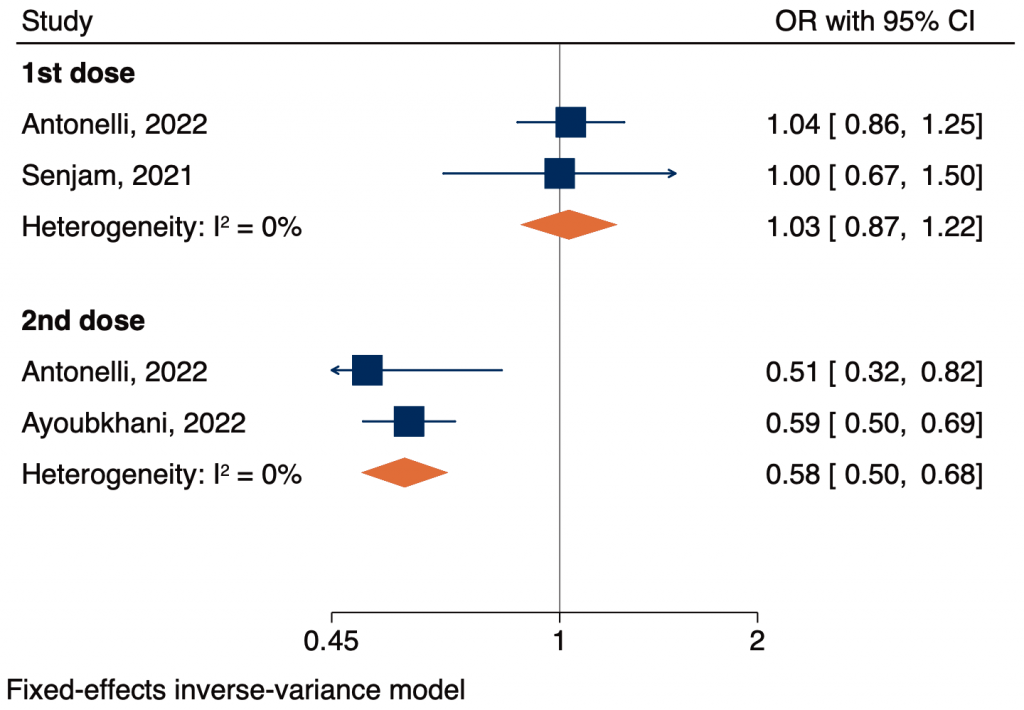
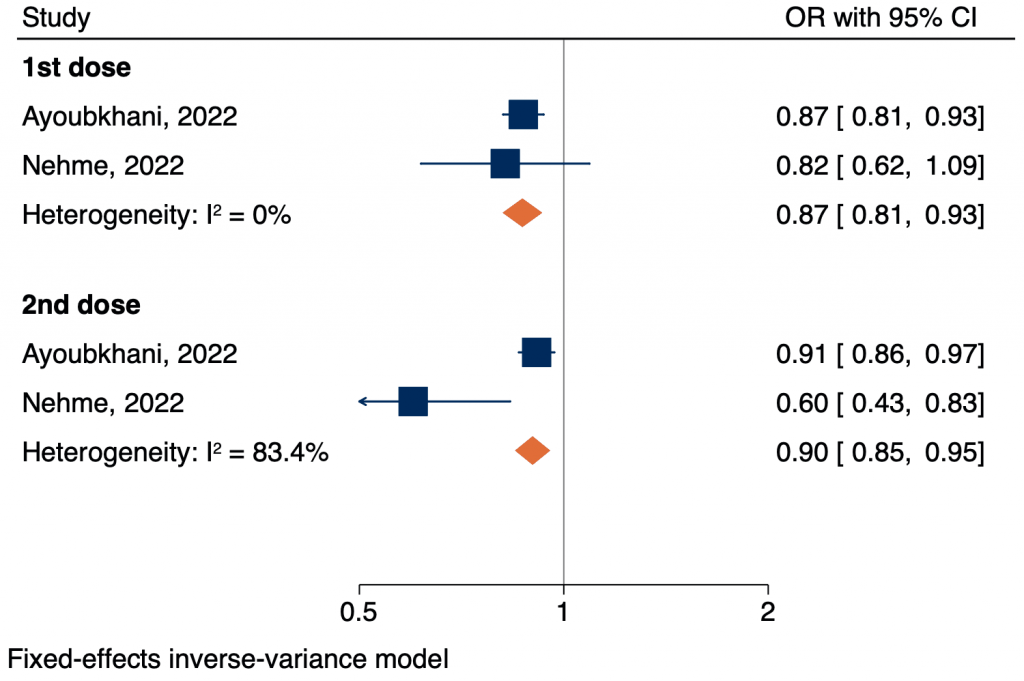
PHAC reviewed 17 studies that reported on symptoms assessed at 12 or more weeks after SARS-CoV-2 infection, and 6 studies that reported on symptoms assessed between 4-12 or more weeks after SARS-CoV-2 infection. In addition to its effects on reducing SARS-CoV-2 infections, it was found that vaccination against COVID-19 with one or two doses of vaccine prior to SARS-CoV-2 infection was associated with a reduction in risk of developing lingering symptoms at either time point by approximately 50%. Vaccination in close proximity after SARS-CoV-2 infection also appeared beneficial in reducing the risk of developing the post COVID-19 condition, although the magnitude of that benefit is uncertain, as is the optimal timing of vaccination, because the findings were based on only three studies.32–34 The largest of the three studies was a cohort study of 28,356 community-dwelling adults, which demonstrated that the first vaccine dose up to 6 months after SARS-CoV-2 infection was associated with a 12.8% decrease (95% CI 18.6 to –6.6), and a second dose was associated with an additional 8.8% decrease (95% CI −14.1 to −3.1) in the odds of developing the post COVID-19 condition.33 Finally, the effect of vaccination after the development of the post COVID-19 condition was examined in 10 studies. Most studies (70%, n=7/10) reported an improvement or resolution of symptoms in those who received one or two doses of vaccine, compared to those who were unvaccinated. Collectively, the evidence from the PHAC and UKHSA reviews is suggestive of a benefit of vaccination before and after SARS-CoV-2 infection as well as possibly among people with established post COVID-19 condition.31
The above reviews pooled results to provide approximate estimates of the effects of vaccination. We performed a fixed-effects meta-analysis of existing studies to provide a more accurate measure of whether vaccine administration before or after acute SARS-CoV-2 infection was associated with any protective effects on the development of the post COVID-19 condition. We were able to provide estimates of vaccine effects administered before and after SARS-CoV-2 infection from a total of four observational studies (Figures 2 and 3).35–38 However, the certainty of the evidence for both meta-analyses was rated as low, which limits our confidence in these estimates. We found that a single dose of vaccination before SARS-CoV-2 infection was not associated with a change in risk of any post COVID-19 symptom when compared with unvaccinated individuals (OR 1.03, 95% CI 0.87-1.22). Those who received two doses of a COVID-19 vaccine had 42% lower odds of experiencing any symptom when compared to unvaccinated people (OR 0.58, 95% CI 0.50-0.62). We found that a single dose of vaccination after SARS-CoV-2 infection was associated with a 13% decrease of any post COVID-19 symptom when compared with unvaccinated individuals after SARS-CoV-2 infection (OR 0.87, 95% CI 0.81-0.93). Those who received two doses of a COVID-19 vaccine had 10% lower odds of experiencing any symptom when compared to unvaccinated people (OR 0.90, 95% CI 0.85-0.95).
Overall, there appears to be some benefit of vaccination in preventing the development of the post COVID-19 condition when given before or after SARS-CoV-2 infection, and possibly after the development of the post COVID-19 condition. These findings support continued efforts to recommend vaccination against SARS-CoV-2.
Risk Factors
There is limited evidence that biological markers, symptoms, clinical findings, or baseline risk can accurately predict who will develop the post COVID-19 condition. Although some studies suggest certain biomarkers measured in blood samples may identify or predict those who will develop the condition,39 the evidence in this field remains uncertain. However, the results of our meta-analysis (Figure 4) in combination with a recent study reporting on risk factors provide some insight. A large retrospective matched cohort study examined risk factors for the post COVID-19 condition in 486,149 adults with confirmed SARS-CoV-2 infection and 1,944,580 propensity-score matched controls without COVID-19.26 Among the cohort of people with confirmed SARS-CoV-2 infection, risk factors significantly associated with the post COVID-19 condition (p<0.05) included female sex, belonging to an ethnic minority, socioeconomic deprivation, smoking, obesity, and a wide range of comorbidities. The risk was also found to increase along a gradient of decreasing age.
We pooled estimates from 18 observational studies and found nine potential risk factors associated with the post COVID-19 condition (Figure 4). It is important to note that some risk factor estimates are based on data from multiple studies, whereas others are limited to a small number. It is also not possible to separate specific risks for people admitted to the ICU from those who were not. The certainty of evidence per risk factor based on our GRADE assessments ranged from very low to low, which is an indication that our certainty in the estimate is limited. Therefore, the variation in risk associated with each factor may be substantially different from the pooled estimate.
Taken together, emerging evidence suggests that female sex, socioeconomic determinants of health, and comorbid conditions appear to be independent risk factors for the development of the post COVID-19 condition.
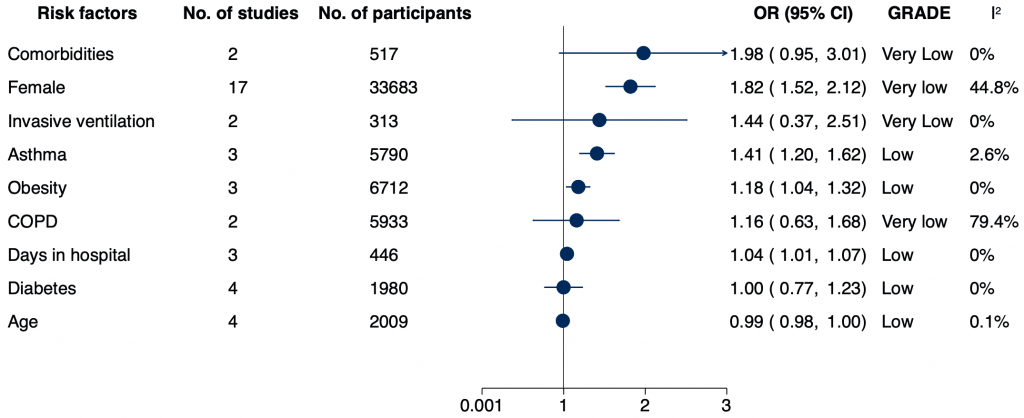
COPD – chronic obstructive pulmonary disease; REML – restricted maximum likelihood. Interpretation of GRADE ratings: ‘High’- We are very confident that the variation in risk associated with the prognostic factor lies close to that of the estimate; ‘Moderate’ – We are moderately confident that the variation in risk associated with the prognostic factor is likely to be close to the estimate, but there is a possibility that it is substantially different; ‘Low’ – Our certainty in the estimate is limited: the variation in risk associated with the prognostic factor may be substantially different from the estimate; ‘Very low’ – We have very little certainty in the estimate: the variation in risk associated with the prognostic factor is likely to be substantially different from the estimate.
Symptoms of the Post COVID-19 Condition
Several systematic reviews pooled data across multiple studies to estimate an overall prevalence of symptoms among people with the post COVID-19 condition.22,40–47 A large systematic review and meta-analysis examined 41 studies to estimate the prevalence of individual symptoms of the post COVID-19 condition across participants with SARS-CoV-2 that experienced symptoms at least 28 days after the index date (first PCR test/diagnosis, date of hospitalization, discharge date, or date of clinical recovery/negative test).22 The five most frequently observed symptoms were fatigue (23%, 95% CI 17-30), memory deficits (14%, 95% CI 10-19), shortness of breath (13%, 95% CI 0.11-0.15), sleep problems (11%, 95% CI 5-23), and joint pain (10%, 95% CI 4-22) (Figure 5). The meta-analysis included 4,165 non-hospitalized people from five studies, 67,161 hospitalized people from 22 studies, and 1,608,677 SARS-CoV-2 positive people from 23 studies in which hospitalization status was not reported.
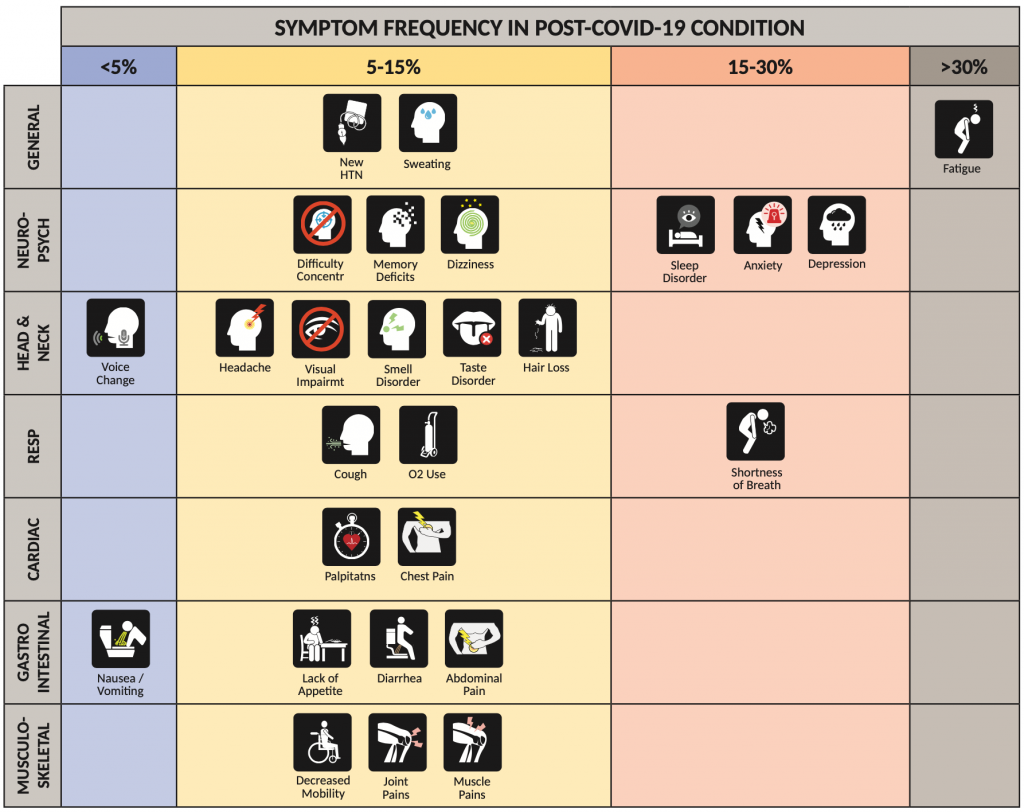
Figure presenting the prevalence of symptoms of the post COVID-19 condition according to organ system. Symptoms in red-shaded regions have >20% prevalence; symptoms in the orange-shaded region have 10-20% prevalence; symptoms in the yellow-shaded regions have 5-10% prevalence; and symptoms in the blue-shaded region have <5% prevalence. CI, confidence interval. Data sourced from Chen et al.22
Still, determining precise estimates of symptom prevalence in people with the post COVID-19 condition remains challenging and is related to the same limitations in estimating the overall prevalence of the condition, including differences in the set of symptoms used to define the condition. Despite findings from the above meta-analysis, there are reported differences in the prevalence of symptoms across the entire spectrum of illness severity in other studies,22 consistent with our understanding of complications after critical illness and ARDS.18 Notably, many of these symptoms were also observed in people who survived critical illness from Severe Acute Respiratory Syndrome (SARS) caused by viral infection with SARS-CoV-1.48 Data comparing prevalence estimates among rigorously identified control groups to those previously infected with SARS-CoV-2 are also lacking.
More than 100 symptoms have been reported among people with the post COVID-19 condition spanning all organ systems. Although the true prevalence of each symptom remains unknown, these symptoms hold the potential to substantially impact people’s quality of life, function, and their ability to work.
Identification of Symptom Clusters
Beyond reporting of individual symptoms, several studies identified “symptom clusters” associated with the post COVID-19 condition. These symptom clusters were defined as the presence of two or more symptoms that were related to each other and were independent of other clusters.49–51 These initial studies suggest a practical approach that categorizes people’s individual symptoms into symptom clusters. The use of symptom clusters as phenotypes may be more practical to use clinically in the assessment, prediction, and treatment of these potentially different phenotypes of the post COVID-19 condition instead of trying to catalogue the diverse array of individual symptoms that a person may report. For example, a “respiratory” cluster characterized predominantly by shortness of breath may suggest that clinicians focus their investigations on pulmonary parenchymal, pulmonary vascular, airway, extrathoracic, diaphragmatic, and cardiac causes of shortness of breath and its related symptoms. The use of symptom clusters may facilitate more uniform estimates of symptom prevalence in future studies compared to an accounting of individual symptoms; however, it should be acknowledged that this benefit may be gained at the expense of oversimplifying the myriad mechanisms that contribute to these complex symptom clusters.
Development of Incident Chronic Conditions following SARS-CoV-2 Infection
Emerging evidence suggests that some people will develop new chronic health conditions, such as diabetes, cerebrovascular disease, cardiovascular disease, or psychiatric illness, that contribute to the additional burden of persisting symptoms and sequelae due to acute SARS-CoV-2 infection.52–56 Similar to other identified risks, there remains substantial uncertainty about the incidence and magnitude of these risks due to limitations in the quality of the evidence that informs them. For example, many of these studies were conducted in mainly older Caucasian and Black males from the United States Veterans Affairs Hospitals; therefore, the generalizability to other populations such as younger adults, females, and other racialized groups remains unknown. Further, some of these findings may be biased using historical comparator groups where healthcare delivery and access may have subsequently changed over time, including during the pandemic, and through increased surveillance and detection related to the need for healthcare support during and after acute infection.
Cardiovascular and Related Conditions
Two cohort studies of more than 300,000 people hospitalized with PCR-confirmed SARS-CoV-2 infection used national healthcare databases from the US Department of Veterans Affairs and found an increased risk of a broad range of cardiovascular complications beyond 30 days of infection up to one year, compared to more than 10 million controls using data from before (e.g., historical) and during (e.g., contemporary) the pandemic. These complications included cerebrovascular disease (e.g., stroke and transient ischemic attacks), dysrhythmias (e.g., atrial fibrillation), ischemic heart disease, heart failure and cardiomyopathies, thromboembolic disorders (e.g., pulmonary embolism and deep vein thrombosis), inflammatory diseases of the heart or pericardium (e.g., pericarditis, myocarditis) and diabetes. For example, previous SARS-CoV-2 infection was associated with a 50% increased risk of stroke (hazard ratio (HR) 1.52, 95% CI 1.43-1.62), translating to a reported excess burden of 4.03 (95% CI 3.32-4.79) cases per 1,000 persons at one year, and a 72% increased risk of heart failure (HR 1.72, 95% CI 1.65-1.80), translating to a reported excess burden of 11.61 (95% CI 10.47-12.78) cases per 1,000 persons at one year.53 There was a 40% increased risk of developing diabetes beyond 30 days of infection (HR 1.40, 95% CI 1.36-1.44), translating to a reported excess burden of 13.46 (95% CI 12.11-14.84) cases per 1,000 people at one year, and an 85% increased risk of the incident need for diabetes medications (HR 1.85, 95% CI 1.78-1.92), translating to a reported excess burden of 12.35 (95% CI 11.36-13.38) cases per 1,000 people at one year. The risks of diabetes appeared to increase in a graded fashion according to the initial severity of acute SARS-CoV-2 infection, but have also been identified among individuals with asymptomatic infections.54
Neurocognitive and Mental Health Disease
An analysis of retrospective cohort studies examined neurological and psychiatric sequelae of COVID-19 occurring primarily in outpatients up to two years after COVID-19 diagnosis.57 People with a confirmed diagnosis of COVID-19 were propensity-score matched with a contemporary control group diagnosed with any other upper or lower respiratory infection. Across 14 neurological and psychiatric sequelae, the majority had an HR significantly greater than one, which indicates elevated risk (e.g., anxiety disorders, cognitive deficits, dementia, epilepsy or seizures, insomnia, ischemic stroke, mood disorder, myoneural junction or muscle disease, nerve, nerve root and plexus disorders, and psychotic disorders). The risk of common psychiatric disorders returned to baseline after one to two months (e.g., mood disorders at 43 days, anxiety disorders at 58 days); however, risks of cognitive deficits (e.g., brain fog), dementia, psychotic disorders, and epilepsy or seizures were still increased at the end of the two-year follow-up period.
A meta-analysis of 43 studies comprising 13,232 people found that approximately one in five individuals exhibited cognitive impairment 12 or more weeks following SARS-CoV-2 infection (pooled proportion 22% (95% CI 17-28); approximately 30% of the people were hospitalized). The prevalence varied depending on whether cognitive impairment was identified through self-report or objective clinical measures. Studies that objectively assessed cognitive impairment reported that 36% of people had cognitive impairment, as compared to 18% of people in whom cognitive impairment was subjectively ascertained through self-report.45
A cohort study of 153,848 hospitalized people with SARS-CoV-2 infection used national healthcare databases from the US Department of Veterans Affairs and found a 35% increased risk of anxiety disorders beyond 30 days of infection up to one year (HR 1.35, 95% CI 1.30-1.39), translating to a reported excess burden of 11.06 (95% CI 9.64-12.53) cases per 1,000 people at 12 months; a 39% increased risk of depressive disorders beyond 30 days of infection (HR 1.39, 95% CI 1.34-1.43), translating to a reported excess burden of 15.12 (95% CI 13.38-16.91) cases per 1,000 people at 12 months; and a 20% increased risk of substance use disorders (HR 1.20, 95% CI 1.15-1.26), translating to a reported excess burden of 4.34 (95% CI 3.22-5.51) cases per 1,000 people at 12 months, compared to more than 10 million contemporary and historical controls, and 72,207 people with seasonal influenza.56
A cohort study of 32,525 adults who survived hospital admission for COVID-19 used linked primary care and national electronic health record databases in England to measure the associated risks of new-onset neuropsychiatric conditions in the 12 months after discharge from a COVID-19-related hospitalization, compared to 16,679 people who were hospitalized for other types of severe acute respiratory infections and over eight million general population controls. There was an approximately two-fold increased risk of anxiety in those hospitalized for COVID-19 (HR 2.36, 95% CI 2.03-2.74). Similarly, increased risks were found for dementia among those hospitalized for COVID-19 (HR 2.55, 95% CI 2.17-3.00).58
Respiratory Disease
A systematic review of seven studies that included 380 people examined the prevalence of a restrictive and obstructive pattern and altered diffusion capacity on pulmonary lung function testing (PFT) in people with prior SARS-CoV-2 infection. Most studies measured these abnormalities approximately 30 days after infection or discharge from hospital. The authors reported a prevalence of reduced diffusion capacity in 39% of people (pooled prevalence 0.39, 95% CI 0.24-0.56), restrictive patterns in 15% of people (pooled prevalence 0.15, 95% CI 0.09-0.22), and obstructive patterns in 7% of people (pooled prevalence 0.07, 95% CI 0.04-0.11). In that review, the authors were unable to account for pre-existing lung disease, nor did they report the severity of the restrictive and obstructive patterns.59 These studies did not include comparator groups, and therefore, the attributable effect of infection on long-term impairments in lung function remains uncertain, especially in non-critically ill populations.
Frailty
Emerging literature suggests that the post COVID-19 condition may affect the risk of becoming frail. A prospective cohort study of 428 survivors of ICU admission with COVID-19 at a single university hospital in Sao Paolo, Brazil assessed frailty using the Clinical Frailty Scale (CFS).60 Overall, 31% were frail at day 90 following discharge — 70% of whom were not previously frail. A separate prospective cohort study included 288 COVID-19 survivors aged 50 years or older (71% were hospitalized for acute COVID-19) who presented for follow-up 3 or more months after acute COVID-19.61 Prior to the development of COVID-19, 6% (n=17) of the cohort were considered frail using a CFS score of ≥4; after COVID-19, 21% (n=60) developed frailty. Additionally, there is a proposed role of “inflammaging” and immunosenescence in the immunopathogenesis of the post COVID-19 condition, and these processes may also increase one’s risk of frailty.62,63 Inflammaging is a chronic state of low-grade inflammation present among those with advanced age, in the absence of overt infection, which may contribute to clinical manifestations of other age-related conditions (e.g., SARS-CoV-1, ARDS, and post-ICU syndrome). Additional studies, particularly those with control comparison groups, are needed to further confirm and validate these results and examine the impact of the post COVID-19 condition on the development of frailty across the spectrum of illness severity in non-hospitalized, hospitalized, and critically ill people.
Impact of Vaccination on the Development of Chronic Conditions
A matched cohort study used data from a large US national health network comprising 1,578,719 people with PCR-confirmed SARS-COV-2 infection to evaluate the associated effects of vaccination on the development of chronic health conditions (e.g., hypertension, diabetes, and heart disease) at 90 days. Among the 1.6% (n=25,225) of the cohort who were vaccinated at the time and had a breakthrough infection, vaccination was found to be protective against the development of multiple chronic conditions and the likelihood of experiencing new or persistent symptoms, compared to those who were unvaccinated. For example, the incidence of hypertension was 6.42 per 1,000 people (rate ratio (RR) 0.33, 95% CI 0.26-0.42); diabetes 2.69 per 1,000 people (RR 0.28, 95% CI 0.20-0.38), and heart disease 7.19 per 1,000 people (RR 0.35, 95% CI 0.29-0.44). Similar findings were observed at four weeks follow-up and suggest that these differences may be attributable to the effects of vaccination.64
Taken together, there appears to be a substantial increase in the risk of developing multiple chronic health conditions following SARS-CoV-2 infection, which define the development of the post COVID-19 condition according to the CDC. It will be critically important to achieve global consensus on the inclusion or exclusion of these sequelae to support research, clinical care and policy efforts aimed at improving care for people with the post COVID-19 condition.
Considerations in Pregnancy
Little is known about the potential spectrum of long-term effects of SARS-CoV-2 infection during pregnancy, especially on the development of the post COVID-19 condition. However, SARS-CoV-2 infection at any time during pregnancy is associated with an increased risk of maternal death (adjusted HR 2.45, 95% CI 1.91-3.13) and blood clots (aHR 3.08, 95% CI 1.09-8.74), as well as preterm birth (aHR 2.09, 95% CI 1.75-2.47). Hospitalization for COVID-19 may also increase the risk of pregestational diabetes (aHR 7.03, 95% CI 2.22-22.2), which in turn may pose an increased risk for future development of diabetes and cardiovascular disease.65 For infants born following SARS-CoV-2 infection during pregnancy, neurodevelopmental disorders may be more common at one year (aOR 1.86, 95% CI 1.03-3.36 for SARS-CoV-2 infection any time during pregnancy; adjusted OR 2.34, 95% CI 1.23-4.44 for infection during the third trimester).66 As increasingly transmissible variants emerge, more research is urgently needed on long-term risks for women who are infected while pregnant and their infants.
Patterns of Health System Utilization Among People with the Post COVID-19 Condition
Ontario-Specific Data
A population-based matched cohort study of 530,232 community-dwelling adults (265,116 with prior PCR-confirmed SARS-CoV-2 infection) in Ontario examined rates of healthcare utilization — a composite of the number of outpatient clinical encounters, homecare encounters, emergency department visits, days hospitalized, and days in long-term care — beginning 56 days after infection. The mean rate of health care utilization was 11% higher in test-positive individuals (RR 1.11, 95% CI 1.10-1.13). Individual components of healthcare use were as follows: ED visits RR 1.03 (95% CI 1.02-1.05); days hospitalized RR 1.49 (95% CI 1.41-1.57); outpatient clinic encounters RR 1.05 (95% CI 1.04-1.05); homecare encounters RR 1.00 (95% CI 0.96-1.05); and days in long-term care RR 2.55 (95% CI 2.28-2.86). These findings translate to an absolute increase in mean person-specific rate of healthcare utilization of 1.4 additional encounters (95% CI 1.2-1.6) per person-year, and an estimated additional 245,000 healthcare encounters per year among those in the top 50% of healthcare use.67
Primary Care Use
A cohort study of over 450,000 people who tested positive for SARS-CoV-2 and were followed for an average of 9 months in England compared their primary care use before the pandemic to the period following their positive test. The rates of primary care use were higher among people who were hospitalized with COVID-19 (adjusted incidence rate ratio (IRR) 1.73, 95% CI 1.68-1.77) and those managed in the community (IRR 1.18, 95% CI 1.17-1.19) compared with 12 months before the diagnosis of COVID-19.68 A cohort study of over 1.4 million people tested for SARS-CoV-2 infection in Norway examined primary care use before and up to six months after a person’s positive test as well as in those with a negative test. A positive test was associated with a 14% (95% CI 7-20) increase in the use of primary care among older women (aged 45-70 years); there was no observed increase in primary care or specialist care use beyond 4 months.69
Mortality and Acute Care Use
A cohort study of 66,287 people with a positive PCR test for SARS-CoV-2 and more than 250,000 controls who tested negative found that those who tested positive had a 3-fold increased risk of dying in the following 12 months compared with those who remained uninfected (HR 3.1, 95% CI 2.9-3.3).70 The risk of dying was highest in the first five weeks following infection. A separate cohort study of 73,435 non-hospitalized people within the Veterans Affairs health system in the US compared mortality at six months following SARS-CoV-2 infection to those without hospitalization or SARS-CoV-2 infection. The adjusted excess death was estimated at 8.30 (95% CI 7.09-9.58) per 1,000 people.71
A cohort study of 47,780 hospitalized adults with COVID-19 in the UK who survived to discharge with a mean follow-up of 140 days reported rates of hospital readmission and mortality of 3.5 and 7.7 times greater than general population controls, respectively.72 The rates of hospital readmission were 766.0 (95% CI 753.4-778.8) per 1,000 person-years in those with prior COVID-19 requiring hospitalization, compared to 218.9 (95% CI 212.4-225.4) per 1,000 person-years in controls. The rates of mortality were 320.0 (95% CI 311.9-328.3) per 1,000 person-years in those with prior COVID-19 requiring hospitalization, compared to 41.3 (95% CI 38.6-44.3) per 1000 person-years among controls. A cohort of over 164,000 hospitalized adults with COVID-19 matched to adults hospitalized with influenza, and to general population controls compared the medium- and long-term risks of hospital admission and death across these three study groups.73 The main findings were that people discharged following hospitalization for COVID-19 had a 2-fold higher associated risk for rehospitalization and death than the general population (HR 2.22, 95% CI 2.14-2.30), and slightly lower risks compared to those hospitalized for influenza (HR 0.95, 95% CI 0.91-0.98). These outcomes were most pronounced in the first 30 days following discharge yet remained substantially elevated over time.73
There is considerable variation in published rates of ED visits and hospitalization across studies and jurisdictions resulting in uncertainty in acute healthcare use among people with the post COVID-19 condition. This observed variation is likely related partly to factors ranging from variant type and to differences in how health care systems managed the pandemic, which further emphasizes the importance of evaluating a health system’s unique contextual factors when measuring rates of ED visits and hospitalization. For example, no studies undertook sub-group analyses for participant subsets, such as rates by pandemic wave, by variant, by vaccine status, by pre-existing comorbidities, or by health care system features, such as the extent to which people had access to hospital care. The pandemic itself resulted in massive shifts in how healthcare was delivered, which may also influence rates of healthcare use among all people, not just those with the post COVID-19 condition. Presently, there are no international studies that compare rates of healthcare between countries to help delineate the potential effects of the post COVID-19 condition on healthcare use from changes in healthcare use directly related to the effects of the pandemic itself. This lack of evidence further increases the uncertainty in estimating healthcare use associated with the post COVID-19 condition, which may be directly impacted by differences in healthcare system resources and organization of care between countries.
People hospitalized with prior SARS-CoV-2 infection appear to have higher rates of mortality, use of emergency department (ED) resources, need for re-hospitalization, and visits to their primary care provider compared to those without infection. These rates are highest in the 30-day period immediately following hospital discharge, yet the risk remains elevated over time. Despite the use of comparison groups across multiple studies, the magnitude of these risks remains uncertain due to the potential for major shifts in healthcare use before and during the pandemic and the inclusion of heterogeneous populations with varying degrees of illness severity.
Prognosis
Anecdotal accounts and published studies suggest that symptoms of the post COVID-19 condition can persist for months, and some may be permanent. While few prognostic studies of the post COVID-19 condition exist, some studies measured its prevalence at numerous follow-up periods, which allows some limited insight into its prognosis.
A longitudinal cohort study examined multiple health outcomes for 1,192 individuals who survived hospitalization due to COVID-19 and were discharged prior to June 2020 from Jin Yin-tan Hospital in Wuhan, China.74 The prevalence of 15 symptoms of the post COVID-19 condition was measured at various follow-up times. The proportion of participants having any one of the 15 symptoms was 68% at six months, 49% at 12 months, and 55% at two years (Figure 6). This suggests that symptoms of the post COVID-19 condition may persist for greater than two years in those previously hospitalized with COVID-19. However, it is unknown if the same is true for non-hospitalized people. It is also unknown if these symptoms are reversible with treatment, or if they will spontaneously resolve at some point in the future.
A 2020 survey of 3,762 participants with confirmed (n=1,020) or suspected (n=2,742) COVID-19 (91.6% non-hospitalized) was conducted to measure the return to baseline health over a study period of seven months.51Respondents were considered recovered if they identified themselves as no longer experiencing symptoms at the time of survey completion. A total of 6.8% of respondents (n=257) recovered after day 28 of illness, and 65.2% (n=2,454) were still experiencing symptoms for at least six months. The probability of symptoms lasting beyond 35 weeks was 91.8% (95% CI 89.5-93.5), and the five most common symptoms reported at this time were brain fog, fatigue, memory issues, post-exertional malaise, and select sensorimotor symptoms (e.g., weakness, numbness, and tingling).
The prognosis of the post COVID-19 condition remains unknown as there is a very limited number of longitudinal studies, few studies of non-hospitalized persons, and a lack of control groups in existing studies. In addition, very few studies followed study participants to the time of symptom resolution. To better our understanding of the natural course of the condition among those with the condition, prognostic studies that include a control group and follow the cohort until symptom resolution are needed.
Impact on Quality of Life, Function, and the Ability to Work
Multiple studies suggest that the associated effects of the post COVID-19 condition appear to extend beyond the development of burdensome symptoms and incident chronic health conditions; it is associated with reduced health-related quality of life (HRQOL) and a person’s ability to function and work.
Quality of Life
The WHO defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.”75 Measures of health-related quality of life (HRQOL) encompass those aspects of an individual or a population’s overall quality of life (QOL) that can be clearly shown to affect their physical or mental health. Studies use a variety of methods to measure QOL, such as validated self-reported tools like the EQ-5D-5L and the EQ-VAS.41,76,77
The proportion of people with the post COVID-19 condition who indicated a reduction in their QOL ranged between 30%-59% in a report published by Public Health Ontario that examined six related systematic reviews.24 In one of the six systematic reviews, the authors meta-analyzed QOL data from 12 studies involving 4,828 people with the post COVID-19 condition with follow-up periods ranging from 30 to 180 days. The unadjusted pooled prevalence of reduced QOL using the self-reported EQ-VAS was 59% (95% CI 42-75; pooled mean score 81.1 (95% CI 75.6-86.5); scored on a scale of 0-100 where higher scores represent better health experience). The authors also examined the proportion of the study population with any impairments across each of the five domains of the EQ-5D-5L questionnaire and prevalence estimates showed impairments in mobility (36%, 95% CI 10-67; e.g., problems with walking around), personal care (8%, 95% CI 1-21; e.g., problems with washing), and usual activities (28%, 95% CI 2-65; e.g., problems with usual activity), and the presence of pain/discomfort (42%, 95% CI 28-55) and anxiety/depression (38%, 95% CI 19-58). A larger proportion of people with the post COVID-19 condition who were admitted to the ICU during their acute COVID-19 reported a poor quality of life compared to those who did not require ICU-level care.77 These findings were similar to a separate systematic review of 39 studies involving 8,293 people that evaluated the impacts of the post COVID-19 condition on QOL between 4 to 12 weeks and >12 weeks after initial SARS-CoV-2 infection.76 The overall mean prevalence of reduced QOL measured using the EQ-5D-5L was reported in 40% of respondents at 4 to 12 weeks, and 57% at >12 weeks.
These reviews suggest a marked reduction in QOL associated with a substantial proportion of individuals with the post COVID-19 condition. However, the included studies did not compare results to population means, most people included in the reviews were hospitalized, and in one review that included critically ill people, poor quality of life was more common among people with the post COVID-19 condition who were admitted to the ICU during their acute infection compared to those who were not admitted to the ICU. As discussed previously, the long-term sequelae of critical illness, ARDS and prolonged ICU admission are well characterized and known to be associated with a greatly reduced QOL.
Taken together, the overall effect of the post COVID-19 condition on people’s QOL remains uncertain but appears to be associated with overall reductions. Further evidence is required to confirm the magnitude and duration of reduced QOL among people with the post COVID-19 condition, including across different illness severities.
Function and the Completion of Activities of Daily Living
Symptoms and sequelae of the post COVID-19 condition may limit an individual’s ability to perform activities of daily living (ADLs). These are activities required to independently care for oneself.78,79 There are two classes of ADLs: 1) basic ADLs, which relate to personal care and mobility (e.g., personal hygiene, dressing, eating, ambulating, and toileting) and 2) instrumental ADLs, which include more complex activities required for a person to interact with their environment (e.g., grocery shopping or banking).78,79
A multicenter study of 1,969 people hospitalized with a PCR-confirmed diagnosis of COVID-19 during the first wave of the pandemic measured functional limitations of people at a mean of 8.4 months after discharge.80Overall, 27.5% (n=542) of people reported limitations in performing their basic ADLs, and 19.7% (n=389) reported limitations in performing their instrumental ADLs. The reasons for a lower prevalence of impairments in instrumental ADLs than in basic ADLs are unclear and may suggest the predominance of physical over cognitive limitations among those included in the study. A systematic review of 9 studies involving 1,465 people (81% were hospitalized) found that ADL performance declined following acute SARS-CoV-2 infection, resulting in a loss of independence for many people.78
The existing research on the effects of the post COVID-19 condition on ADLs remains extremely limited and is primarily reported among people previously hospitalized with acute COVID-19, some of whom were also admitted to the ICU. Therefore, it is not possible to draw conclusions about functional impairments that are specific to the post COVID-19 condition that may not also be related to the effects of hospitalization or critical illness.
Worker Absenteeism, Return to Work, and Workload Accommodations
Worker absenteeism poses substantial challenges to individuals with the post COVID-19 condition, their workplaces, the economy, and the government. A review performed up to July 2021 found 102 primary studies that examined the effects of the post COVID-19 condition on socioeconomic domains found that 50% of the studies reported some degree of impairment in social and family life, long absences from work, the need for adjusted workloads, and loss of employment.81 For example, among studies of non-hospitalized people with mild to moderate SARS-CoV-2 infection, 12% to 23% remained absent from work or had long absence periods of three to seven months following infection. Among studies of previously hospitalized people with COVID-19, work absence was reported in 9% to 40% of those who were previously employed two to three months after discharge. Among studies of non-hospitalized people with mild to moderate disease, these proportions ranged between 8% to 45%.81 In the Wuhan cohort study of 1,192 individuals in the first wave who survived hospitalization due to COVID-19, 12% and 11% of people were unable to return to their original work at 12 months and two years follow-up, respectively. In the UK, approximately 2.9 million people (7% of the UK working-age population) have had or are still experiencing the post COVID-19 condition. Economic inactivity has risen by over 120,000 people (0.29% of the UK working-age population), contributing to the current labour shortage in the UK, and approximately 80,000 people (0.19% of the UK working-age population) have left employment due to the post COVID-19 condition.82 The US Census Bureau estimated that the number of 16-and-older Americans with a disability has increased by approximately two million since early 2020 and that between 2 and 4 million people are not able to work.83–85
The collective evidence to date suggests that a substantial proportion of individuals with the post COVID-19 condition miss work, though estimates of worker absenteeism vary widely across studies, and the duration of the impact of the post COVID-19 condition on one’s ability to work remains unknown.
Treatment of the Post COVID-19 Condition
There are presently no known treatments specifically for the post COVID-19 condition, including those that improve quality of life, functioning, or a person’s ability to work. However, several therapies are currently recommended for the treatment of the most common symptoms (e.g., shortness of breath, fatigue, racing heart) of the post COVID-19 condition by various guidelines and by experts in the management of the condition.5,7,9,10,86–89 The discussion of these is beyond the scope of this Brief.
Models of Care
Several models of care for people with the post COVID-19 condition have been proposed based on experiences with early care delivery. The primary care provider (PCP)90 model involves direct assessment of people who may have the post COVID-19 condition by their PCP (provided that the person has one) to identify their care needs. Based on these assessments, PCPs may provide self-management support, manage medications and comorbidities, and/or refer people to specialists for ongoing assessment and management of certain select elements of the post COVID-19 condition they do not feel comfortable managing or that are out of scope for their practice.90 The specialized post COVID-19 condition clinic model involves a dedicated multidisciplinary team of health providers often with specific expertise in rehabilitation medicine who support people and their multifactorial care needs. The hybrid care model involves both specialized clinics and primary care depending on a person’s needs, which may also include the use of virtual care.90
There is no evidence evaluating which care model is most effective in supporting people with the post COVID-19 condition, nor are there any studies examining the cost-effectiveness of different care models. Further, careful consideration and engagement with rural, remote, and Indigenous communities on models of care will be important. Health human resources (HHR) are not equally distributed across the province. Rural and remote regions often have disparate access, and in many cases, chronic shortages of healthcare providers, despite the increased need for services due to the burden of health in these regions. Implementation of care models should also consider those not rostered to or those lacking a PCP.
Two clinical trials evaluating the effectiveness and experience with different care models are currently underway. The STIMULATE-ICP study is using interviews with people and health care professionals, follow-up surveys on the outcomes of care and cost, clinical data, and routine hospital data to examine the “usual care” pathway in post COVID services in England.91 The LOCOMOTION Trial in the UK uses self-monitoring surveys built into mobile apps, data from post COVID-19 condition clinics, and interviews with people to learn about treatment for the post COVID-19 condition and provide education for healthcare professionals.92
The optimal care delivery model for people with the post COVID-19 condition remains unknown, pending the publication of evidence studying their effects across different jurisdictions.
Barriers to Supporting People with the Post COVID-19 Condition
There are several system-level barriers to assessing and supporting people with the post COVID-19 condition.93 These include 1) a lack of proven therapies to treat the post COVID-19 condition; 2) limited access to care including long wait times and possible staffing shortages; and 3) inconsistent application of insurance policies for reimbursement, especially for disability claims. Further, variable use or lack of diagnostic and physician fee codes limits our ability to track and evaluate care delivery and outcomes at a population level for the purposes of identifying where care gaps exist more broadly.
In Canada, current average wait times to access multidisciplinary clinics that treat the post COVID-19 condition are reported to be between 3-6 months. In the US, UK, and Italy, wait times are reported to be between 7-9 months. The related factors identified that contribute to lengthy wait times are: 1) a limited number of clinics due to insufficient funding; 2) increasing demand amidst a high number of existing patients; 3) low staffing; 4) lengthy triage processes from referral to therapy; and 5) a limited ability to access existing clinics.94–96 Limited resources for primary care, along with fragmented care resulting from complicated care coordination processes with specialists, may also contribute to delays in receiving treatment for the post COVID-19 condition.90 In rural, remote, and indigenous communities, there also exist significant limitations in available HHR, with a disparity in regional distribution of those HHR.
There are also numerous factors that must be considered to ensure equitable provision of care for people with the post COVID-19 condition. COVID-19 disproportionately affects marginalized populations.97 In turn, these populations may be at higher risk of developing the post COVID-19 condition due to a higher prevalence of underlying risk factors, and may also face greater barriers in receiving adequate healthcare and financial support if they go on to develop the post COVID-19 condition.98–100
Although many healthcare services in Ontario are universally accessible through the Ontario Health Insurance Plan (OHIP), including counselling by primary care providers, some services, such as those provided by some private physiotherapy and psychosocial counselling, may be limited to those who have private insurance or financial means to pay for them. An inability to pay for food and housing and an inability to work due to disability, also poses serious personal and financial risks. Social Assistance is provided in Ontario through The Ontario Disability Support Plan (ODSP) and Ontario Works (OW) to support people in financial need who meet the eligibility criteria,101 and many people own private insurance policies for long-term disability in the event they are unable to work. It is unknown how many people with the post COVID-19 condition in Ontario have applied for ODSP or OW. There may be barriers to receiving financial support through private insurance for disability related to COVID-19 due to 1) lack of medical evidence of SARS-CoV-2 infection, including the lack of a positive COVID-19 test. From an equity standpoint, this may be of particular concern after the first part of the Omicron wave where nearly 40% of the Canadian public was infected, but very few had access to PCR testing;102 2) the presence of subjective symptoms such as fatigue, brain fog, and depression that are more challenging to measure and are themselves additional barriers to accessing timely and effective medical care; 3) denial of post COVID-19 claim by insurance companies even when evidence of symptoms is provided; and 4) in other jurisdictions there are reported difficulty obtaining new health, disability, and life insurance policies as COVID-19 is considered a pre-existing condition.99,103 We have incomplete evidence about how this will be handled in a Canadian context
It will be important for health systems and policymakers to be proactive in preparing a comprehensive strategy to address these multiple potential barriers. These may include increasing the number of specialized clinics and support for primary care, supporting research efforts to discover new therapies and measure the impacts of post COVID-19 condition among those with prior disability and among low-income and marginalized populations, and development of policy to ensure fair and equitable adjudication of insurance and disability claims.
Administrative and Fee Coding
A potential barrier to supporting people with the post COVID-19 condition is the lack of specific diagnostic codes that can be used to track and evaluate care outcomes. A dedicated diagnostic code that is feasible to use across all care settings would help standardize coding and in turn facilitate research and evaluation at a population level.
Though ICD diagnostic codes have been developed to track the post COVID-19 condition in Canada (U07.4 – post COVID-19 condition), it has not yet been implemented for use in the outpatient setting, which limits its use in studying healthcare delivery and outcomes of people with the post COVID-19 condition across the care continuum. Without a universally deployed diagnostic code, identifying and characterizing healthcare use and outcomes (especially for non-hospitalized people) with the post COVID-19 condition remains extremely challenging.
Further, the lack of a dedicated OHIP physician fee code limits reimbursement of healthcare services, which in turn may influence care delivery and reimbursement for private insurance claims.98,99 Although the literature in this area is limited, some studies report that inconsistent insurance reimbursement and billing codes presented a significant barrier to the follow-up of services.98 Virtual care was used widely during the pandemic and continues to be used in the care of people with the post COVID-19 condition. However, there is currently insufficient evidence to evaluate its effectiveness in delivering high-quality care among people with the condition. Virtual care may be beneficial for people with the post COVID-19 condition given that some affected by it may have difficulty attending multiple in-person appointments with various specialists related to geography, impairment in mobility or post-exertional malaise. When reductions on telephone reimbursement of virtual care in Ontario come into effect in the near future, it will be important to evaluate the impact of virtual care and changes in physician reimbursement on care delivery to people with the post COVID-19 condition. This evaluation may be especially important to consider among those with certain disabilities and impairments in function, those who live in rural and remote regions, and Indigenous communities.104
There are also calls for increased government funding to support the expansion of multidisciplinary post COVID-19 condition clinics.99 The creation of specific post-COVID-19 condition fee codes would facilitate better tracking of healthcare needs and services, and may also incentivize the provision of care for low-income and marginalized populations.98,99 The introduction of a complexity modifier to the capitation payment system for primary care physicians has been proposed as a potential means to address structural inequities in access to care; it is one example of how to influence physician practice behaviour using economic levers.
Unanswered Questions
- Will distinguishing lingering symptoms of acute COVID-19 from new symptoms that arise after the resolution of the acute disease further our understanding of potential disease mechanisms?8
- What is the prevalence and impact of the post COVID-19 condition on marginalized and at-risk populations, such as those with low income, those on social assistance, those with prior disability and Indigenous populations?
- Do treatments given at the time of acute COVID-19, or after the development of the post COVID-19 condition (e.g., dexamethasone, remdesivir, tocilizumab, monoclonal antibodies, Paxlovid) alter the prevalence, associated impairments, or duration of the post COVID-19 condition?
- What are the patterns of other measures of health system utilization among people with the post COVID-19 condition, such as the use of certain diagnostic tests (e.g., pulmonary function tests, echocardiograms, computed tomography (CT) scans, and magnetic resonance imaging (MRI) scans, etc.), the use of specialist physician care (including palliative care), home care, and the use of medical, cardiac, and pulmonary rehabilitation services?
Interpretation
The post COVID-19 condition is a common, complex, and heterogeneous condition that develops in people with prior SARS-CoV-2 infection. There are over 100 symptoms reported in people with the post COVID-19 condition spanning multiple physiologic systems. These burdensome symptoms appear to be associated with poor quality of life, reduced function, and impairments in people’s ability to work and care for themselves. Many people also appear to develop new chronic health conditions following SARS-CoV-2 infection, which hold the potential to have a further impact on the health system through increased healthcare service needs and potential disability. Taken together, the post COVID-19 condition is likely to impart a significant burden on our citizens, our health systems, and potentially our economy.
Uncertainty remains around the magnitude of these risks due to limitations in the quality of available published evidence. The lack of a globally accepted definition continues to hinder efforts to estimate prevalence and risk more accurately, which is critical to health system planning and resource allocation. There are major theoretical equity concerns related to rates of infection and, therefore, subsequent development of the post COVID-19 condition as well as barriers in access to care support among marginalized, disabled, and racialized/ethnic populations. One of the most important questions is whether incident chronic conditions that arise following SARS-CoV-2 infection be considered under the umbrella of the post COVID-19 condition or post-acute sequelae of SARS-CoV-2 infection? Through the lens of the affected person, caregiver, and health system planner, it may be an arbitrary distinction given that many of these chronic conditions are also associated with poor quality of life, burdensome symptoms, increased need for healthcare services, and often a shortened survival.
Many other limitations in our understanding of the post COVID-19 condition remain. Current evidence is not sufficient to make definitive conclusions about how many people with the post COVID-19 condition have overlapping impairments in their quality of life and ability to work or function. Although our understanding of the underlying pathophysiologic mechanisms that lead to its development is still limited, ongoing research in this area continues to provide further evidence for potential therapeutic targets. The evidence for the effects of vaccination against SARS-CoV-2 continues to evolve yet demonstrates promise as part of a multi-pronged approach to treatment. It is still unclear which models of care are most effective in supporting the care of people with the post COVID-19 condition and their caregivers.
Health systems around the world continue to bear witness to the devastating effects of the COVID-19 pandemic. Amidst it all, people collaborated on a global scale to discover preventive strategies and vaccines, new therapies, and innovative care pathways. One of our next great challenges will be the management of successive acute COVID-19 waves with a potential long tail of hardship from the post COVID-19 condition. Substantial investments in research, clinical care pathways and health policy are needed to ensure sustainable care for people with the post COVID-19 condition in the long term.
Methods Used for This Science Brief
We searched PubMed, Google Scholar, the COVID-19 Rapid Evidence Reviews, the Joanna Briggs Institute’s COVID-19 Special Collection, LitCovid in PubMed, the Oxford COVID-19 Evidence Service, the World Health Organization’s Global Literature on Coronavirus Disease, and other COVID-19 specific resources listed by the Guidelines International Network and the McMaster Health Forum. In addition, we reviewed Evidence Synthesis Briefing Notes published by the COVID-19 Evidence Synthesis Network and Public Health Ontario and retrieved reports citing relevant articles through Google Scholar and reviewed references from identified articles for additional studies. The comprehensive search was last updated on May 20, 2022, and new studies identified in weekly reviews of the literature were added up to August 30, 2022. The methods for the evidence scans performed by the COVID-19 Evidence Synthesis Network can be found in the methods sections of the Briefing Notes. We conducted our meta-analyses using STATA Release 16.0 software (StataCorp LLC, College Station, TX) using a random-effects model to quantify the risk factors and a Mantel-Haenszel fixed-effects model on the impact of vaccination. We used the QUIPS tool to evaluate the risk of bias of the included studies,105 and we evaluated the level of certainty in the evidence of each factor by using Grading of Recommendations, Assessment, Development and Evaluations (GRADE) criteria.106
The outcomes of the post COVID-19 condition are described in existing literature using sample populations with either previous SARS-CoV-2 infection or established post COVID-19 condition. Distinguishing how these outcomes were measured is critical to accurately interpreting the findings of this Science Brief. Measurements of outcomes are classified in Table 2.
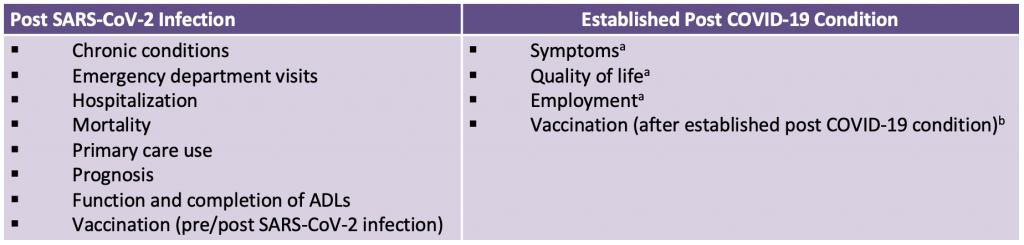
Table classifying the outcomes of the post COVID-19 condition that are examined in this Science Brief as being measured in individuals after SARS-CoV-2 infection or in individuals with established post COVID-19 condition. aResearchers used modified versions of the WHO definition for the post COVID-19 condition that varied in duration of symptoms (28 or more days) and symptoms classified as part of the condition. bResearchers used a mixture of the WHO and CDC definitions of the post COVID-19 condition.
CanCOVID performed research evidence scans for this Science Brief, which was last updated on June 13, 2022. CanCOVID is a network of active researchers, academics, patient partners, decision-makers, and industry partners dedicated to an evidence-informed response to the COVID‑19 pandemic.
References
1. Ritchie H, Mathieu E, Rodés-Guirao L, et al. Coronavirus Pandemic (COVID-19).; 2020. https://ourworldindata.org/covid-cases
2. Razak F, Katz GM, Cheung AM, et al. Understanding the post COVID-19 condition (long COVID) and the expected burden for Ontario. Ont COVID-19 Sci Advis Table. 2021;2(44). https://doi.org/10.47326/ocsat.2021.02.44.1.0
3. World Health Organization. A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. Published October 6, 2021. https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1
4. Public Health Agency of Canada. Post-COVID-19 condition (long COVID). Published August 20, 2021. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/symptoms/post-covid-19-condition.html
5. National Institute for Health Care and Excellence. COVID-19 rapid guideline: Managing the long-term effects of COVID-19. NICE. Published December 18, 2020. Accessed August 10, 2021. https://www.nice.org.uk/guidance/ng188/chapter/1-Identifying-people-with-ongoing-symptomatic-COVID-19-or-post-COVID-19-syndrome
6. CDC. Post-COVID conditions. Centers for Disease Control and Prevention. Published July 11, 2022. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html
7. CDC. Evaluating and caring for patients with post-COVID conditions: Interim guidance. Centers for Disease Control and Prevention. Published February 11, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-background.html
8. Mehandru S, Merad M. Pathological sequelae of long-haul COVID. Nat Immunol. 2022;23(2):194-202. https://doi.org/10.1038/s41590-021-01104-y
9. Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601-615. https://doi.org/10.1038/s41591-021-01283-z
10. Crook H, Raza S, Nowell J, Young M, Edison P. Long covid—mechanisms, risk factors, and management. BMJ. 2021;374:n1648. https://doi.org/10.1136/bmj.n1648
11. Su Y, Yuan D, Chen DG, et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell. 2022;185(5):881-895.e20. https://doi.org/10.1016/j.cell.2022.01.014
12. Ruiz-Pablos M, Paiva B, Montero-Mateo R, Garcia N, Zabaleta A. Epstein-Barr virus and the origin of myalgic encephalomyelitis or chronic fatigue syndrome. Front Immunol. 2021;12. https://doi.org/10.3389/fimmu.2021.65679
13. Peluso MJ, Deeks SG. Early clues regarding the pathogenesis of long-COVID. Trends Immunol. 2022;43(4):268-270. https://doi.org/10.1016/j.it.2022.02.008
14. Douaud G, Lee S, Alfaro-Almagro F, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. Published online March 7, 2022. https://doi.org/10.1038/s41586-022-04569-5
15. de Paula JJ, Paiva RERP, Souza-Silva NG, et al. Selective visuoconstructional impairment following mild COVID-19 with inflammatory and neuroimaging correlation findings. Mol Psychiatry. Published online June 14, 2022:1-11. https://doi.org/10.1038/s41380-022-01632-5
16. Swank Z, Senussi Y, Alter G, Walt DR. Persistent circulating SARS-CoV-2 spike is associated with post-acute COVID-19 sequelae. medRxiv. Pathology; 2022. https://doi.org/10.1101/2022.06.14.22276401
17. Krishna BA, Lim EY, Mactavous L, et al. Evidence of previous SARS-CoV-2 infection in seronegative patients with long COVID. eBioMedicine. 2022;81. https://doi.org/10.1016/j.ebiom.2022.104129
18. Herridge MS, Azoulay É. The COVID-19 continuum of illness. Lancet Respir Med. 2022;10(7):630-631. https://doi.org/10.1016/S2213-2600(22)00219-3
19. World Health Organization. Coronavirus disease (COVID-19): Post COVID-19 condition. Published December 16, 2021. https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-post-covid-19-condition
20. Self-reported long COVID after infection with the Omicron variant in the UK: 18 July 2022. Office for National Statistics. Published July 18, 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/selfreportedlongcovidafterinfectionwiththeomicronvariant/18july2022
21. van Kessel SAM, Olde Hartman TC, Lucassen PLBJ, van Jaarsveld CHM. Post-acute and long-COVID-19 symptoms in patients with mild diseases: A systematic review. Fam Pract. 2022;39(1):159-167. https://doi.org/10.1093/fampra/cmab076
22. Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: A meta-analysis and systematic review. J Infect Dis. Published online April 16, 2022:jiac136. https://doi.org/10.1093/infdis/jiac136
23. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 6 May 2022. Published May 6, 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/6may2022#measuring-the-data
24. Public Health Ontario. Post-acute COVID-19 syndrome (PACS) in adults. Public Health Ontario; 2022:49. https://www.publichealthontario.ca/-/media/Documents/nCoV/ipac/2022/04/post-acute-covid-syndrome-pacs.pdf?sc_lang=en
25. Huang L, Li X, Gu X, et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: A longitudinal cohort study. Lancet Respir Med. Published online May 11, 2022. https://doi.org/10.1016/S2213-2600(22)00126-6
26. Subramanian A, Nirantharakumar K, Hughes S, et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat Med. 2022;28(8):1706-1714. https://doi.org/10.1038/s41591-022-01909-w
27. Ballering AV, Zon SKR van, Hartman TC olde, Rosmalen JGM. Persistence of somatic symptoms after COVID-19 in the Netherlands: An observational cohort study. The Lancet. 2022;400(10350):452-461. https://doi.org/10.1016/S0140-6736(22)01214-4
28. Self-reported long COVID after infection with the Omicron variant in the UK: 6 May 2022. Office for National Statistics. Published May 6, 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/selfreportedlongcovidafterinfectionwiththeomicronvariant/6may2022#measuring-the-datahttps://www.medrxiv.org/content/10.1101/2022.05.12.22274990v1.full-
29. Antonelli M, Pujol JC, Spector TD, Ourselin S, Steves CJ. Risk of long COVID associated with Delta versus Omicron variants of SARS-CoV-2. The Lancet. 2022;399(10343):2263-2264. https://doi.org/10.1016/S0140-6736(22)00941-2
30. UKHSA COVID-19 Evidence Team. The effectiveness of vaccination against long COVID: A rapid evidence briefing. UKHSA COVID-19 Evidence Team; 2022. https://ukhsa.koha-ptfs.co.uk/cgi-bin/koha/opac-retrieve-file.pl?id=fe4f10cd3cd509fe045ad4f72ae0dfff
31. Public Health Agency of Canada. Archived 1: Evidence brief on the associations and safety of COVID-19 vaccination and post COVID-19 condition. Published March 22, 2022. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/canadas-reponse/summaries-recent-evidence/evidence-brief-associations-safety-covid-19-vaccination-post-condition.html
32. Peghin M, Martino MD, Palese A, et al. Post–COVID-19 syndrome and humoral response association after 1 year in vaccinated and unvaccinated patients. Clin Microbiol Infect. 2022;28(8):1140-1148. https://doi.org/10.1016/j.cmi.2022.03.016
33. Ayoubkhani D, Bermingham C, Pouwels KB, et al. Changes in the trajectory of long Covid symptoms following COVID-19 vaccination: Community-based cohort study. medRxiv. Published online December 9, 2021:2021.12.09.21267516. https://doi.org/10.1101/2021.12.09.21267516
34. Simon MA, Luginbuhl RD, Parker R. Reduced incidence of long-COVID symptoms related to administration of COVID-19 vaccines both before COVID-19 diagnosis and up to 12 weeks after. medRxiv. Published online November 18, 2021:2021.11.17.21263608. https://doi.org/10.1101/2021.11.17.21263608
35. Ayoubkhani D, Bermingham C, Pouwels KB, et al. Trajectory of long COVID symptoms after COVID-19 vaccination: Community based cohort study. BMJ. 2022;377:e069676. https://doi.org/10.1136/bmj-2021-069676
36. Antonelli M, Penfold RS, Merino J, et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID symptom study app: A prospective, community-based, nested, case-control study. Lancet Infect Dis. 2022;22(1):43-55. https://doi.org/10.1016/S1473-3099(21)00460-6
37. Senjam SS, Balhara YPS, Kumar P, et al. Assessment of post COVID-19 health problems and its determinants in North India: A descriptive cross section study. medRxiv. Published online October 7, 2021:2021.10.03.21264490. https://doi.org/10.1101/2021.10.03.21264490
38. Nehme M, Braillard O, Salamun J, et al. Symptoms after COVID-19 vaccination in patients with post-acute sequelae of SARS-CoV-2. J Gen Intern Med. 2022;37(6). https://doi.org/10.1007/s11606-022-07443-2
39. Klein J, Wood J, Jaycox J, et al. Distinguishing features of long COVID identified through immune profiling. medRxiv. Published online August 10, 2022:2022.08.09.22278592. https://doi.org/10.1101/2022.08.09.22278592
40. Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global prevalence of post-acute sequelae of COVID-19 (PASC) or long COVID: A meta-analysis and systematic review. medRxiv. Published online November 16, 2021:2021.11.15.21266377. https://doi.org/10.1101/2021.11.15.21266377
41. Groff D, Sun A, Ssentongo AE, et al. Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection: A systematic review. JAMA Netw Open. 2021;4(10):e2128568. https://doi.org/10.1001/jamanetworkopen.2021.28568
42. Lopez-Leon S, Wegman-Ostrosky T, Perelman C, et al. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. medRxiv. Published online January 30, 2021:2021.01.27.21250617. https://doi.org/10.1101/2021.01.27.21250617
43. Alkodaymi MS, Omrani OA, Fawzy NA, et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: A systematic review and meta-analysis. Clin Microbiol Infect. 2022;28(5):657-666. https://doi.org/10.1016/j.cmi.2022.01.014
44. Premraj L, Kannapadi NV, Briggs J, et al. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: A meta-analysis. J Neurol Sci. 2022;434. https://doi.org/10.1016/j.jns.2022.120162
45. Ceban F, Ling S, Lui LMW, et al. Fatigue and cognitive impairment in Post-COVID-19 Syndrome: A systematic review and meta-analysis. Brain Behav Immun. 2022;101:93-135. https://doi.org/10.1016/j.bbi.2021.12.020
46. Fernández-de-las-Peñas C, Navarro-Santana M, Gómez-Mayordomo V, et al. Headache as an acute and post-COVID-19 symptom in COVID-19 survivors: A meta-analysis of the current literature. Eur J Neurol. 2021;28(11):3820-3825. https://doi.org/10.1111/ene.15040
47. Badenoch JB, Rengasamy ER, Watson C, et al. Persistent neuropsychiatric symptoms after COVID-19: A systematic review and meta-analysis. Brain Commun. 2022;4(1):fcab297. https://doi.org/10.1093/braincomms/fcab297
48. Tansey CM, Louie M, Loeb M, et al. One-year outcomes and health care utilization in survivors of severe acute respiratory syndrome. Arch Intern Med. 2007;167(12):1312-1320. https://doi.org/10.1001/archinte.167.12.1312
49. Whitaker M, Elliott J, Chadeau-Hyam M, et al. Persistent COVID-19 symptoms in a community study of 606,434 people in England. Nat Commun. 2022;13(1):1957. https://doi.org/10.1038/s41467-022-29521-z
50. Huang Y, Pinto MD, Borelli JL, et al. COVID symptoms, symptom clusters, and predictors for becoming a long-hauler: Looking for clarity in the haze of the pandemic. medRxiv. Published online March 5, 2021:2021.03.03.21252086. https://doi.org/10.1101/2021.03.03.21252086
51. Davis HE, Assaf GS, McCorkell L, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. Published online July 15, 2021. https://doi.org/10.1016/j.eclinm.2021.101019
52. Tu TM, Seet CYH, Koh JS, et al. Acute ischemic stroke during the convalescent phase of asymptomatic COVID-2019 infection in men. JAMA Netw Open. 2021;4(4):e217498. https://doi.org/10.1001/jamanetworkopen.2021.7498
53. Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28(3):583-590. https://doi.org/10.1038/s41591-022-01689-3
54. Xie Y, Al-Aly Z. Risks and burdens of incident diabetes in long COVID: A cohort study. Lancet Diabetes Endocrinol. 2022;0(0). https://doi.org/10.1016/S2213-8587(22)00044-4
55. Katsoularis I, Fonseca-Rodríguez O, Farrington P, et al. Risks of deep vein thrombosis, pulmonary embolism, and bleeding after COVID-19: Nationwide self-controlled cases series and matched cohort study. BMJ. 2022;377:e069590. https://doi.org/10.1136/bmj-2021-069590
56. Xie Y, Xu E, Al-Aly Z. Risks of mental health outcomes in people with covid-19: Cohort study. BMJ. 2022;376:e068993. https://doi.org/10.1136/bmj-2021-068993
57. Taquet M, Sillett R, Zhu L, et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: An analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry. Published online August 17, 2022. https://doi.org/10.1016/S2215-0366(22)00260-7
58. Clift AK, Ranger TA, Patone M, et al. Neuropsychiatric ramifications of severe COVID-19 and other severe acute respiratory infections. JAMA Psychiatry. 2022;79(7):690-698. https://doi.org/10.1001/jamapsychiatry.2022.1067
59. Torres-Castro R, Vasconcello-Castillo L, Alsina-Restoy X, et al. Respiratory function in patients post-infection by COVID-19: A systematic review and meta-analysis. Pulmonology. 2021;27(4):328-337. https://doi.org/10.1016/j.pulmoe.2020.10.013
60. Taniguchi LU, Avelino-Silva TJ, Dias MB, Jacob-Filho W, Aliberti MJR, on behalf of COVID-19 and Frailty (CO-FRAIL) Study Group and EPIdemiology of Critical COVID-19 (EPICCoV) Study Group for CH das C. Patient-centered outcomes following COVID-19: Frailty and disability transitions in critical care survivors. Crit Care Med. 2022;50(6):955-963. https://doi.org/10.1097/CCM.0000000000005488
61. Müller I, Mancinetti M, Renner A, et al. Frailty assessment for COVID-19 follow-up: A prospective cohort study. BMJ Open Respir Res. 2022;9(1):e001227. https://doi.org/10.1136/bmjresp-2022-001227
62. Guaraldi G, Milic J, Cesari M, et al. The interplay of post-acute COVID-19 syndrome and aging: A biological, clinical and public health approach. Ageing Res Rev. 2022;81:101686. https://doi.org/10.1016/j.arr.2022.101686
63. Bektas A, Schurman SH, Franceschi C, Ferrucci L. A public health perspective of aging: Do hyper-inflammatory syndromes such as COVID-19, SARS, ARDS, cytokine storm syndrome, and post-ICU syndrome accelerate short- and long-term inflammaging? Immun Ageing. 2020;17(1):23. https://doi.org/10.1186/s12979-020-00196-8
64. Zisis SN, Durieux JC, Mouchati C, Perez JA, McComsey GA. The protective effect of coronavirus disease 2019 (COVID-19) vaccination on postacute sequelae of COVID-19: A multicenter study from a large national health research network. Open Forum Infect Dis. 2022;9(7):ofac228. https://doi.org/10.1093/ofid/ofac228
65. Ferrara A, Hedderson MM, Zhu Y, et al. Perinatal complications in individuals in California with or without SARS-CoV-2 infection during pregnancy. JAMA Intern Med. 2022;182(5):503-512. https://doi.org/10.1001/jamainternmed.2022.0330
66. Edlow AG, Castro VM, Shook LL, Kaimal AJ, Perlis RH. Neurodevelopmental outcomes at 1 year in infants of mothers who tested positive for SARS-CoV-2 during pregnancy. JAMA Netw Open. 2022;5(6):e2215787. https://doi.org/10.1001/jamanetworkopen.2022.15787
67. McNaughton CD, Austin PC, Sivaswamy A, et al. Post-acute health care burden after SARS-CoV-2 infection: A retrospective cohort study of long COVID among 530,892 adults. medRxiv. Published online May 7, 2022:2022.05.06.22274782. https://doi.org/10.1101/2022.05.06.22274782
68. Whittaker HR, Gulea C, Koteci A, et al. GP consultation rates for sequelae after acute COVID-19 in patients managed in the community or hospital in the UK: Population based study. BMJ. 2021;375:e065834. https://doi.org/10.1136/bmj-2021-065834
69. Skyrud KD, Hernæs KH, Telle KE, Magnusson K. Impacts of mild COVID-19 on elevated use of primary and specialist health care services: A nationwide register study from Norway. PLOS ONE. 2021;16(10):e0257926. https://doi.org/10.1371/journal.pone.0257926
70. Uusküla A, Jürgenson T, Pisarev H, et al. Long-term mortality following SARS-CoV-2 infection: A national cohort study from Estonia. Lancet Reg Health Eur. 2022;18:100394. https://doi.org/10.1016/j.lanepe.2022.100394
71. Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. 2021;594(7862):259-264. https://doi.org/10.1038/s41586-021-03553-9
72. Ayoubkhani D, Khunti K, Nafilyan V, et al. Post-COVID syndrome in individuals admitted to hospital with COVID-19: Retrospective cohort study. BMJ. 2021;372:n693. https://doi.org/10.1136/bmj.n693
73. Bhaskaran K, Rentsch CT, Hickman G, et al. Overall and cause-specific hospitalisation and death after COVID-19 hospitalisation in England: A cohort study using linked primary care, secondary care, and death registration data in the OpenSAFELY platform. PLOS Med. 2022;19(1). https://doi.org/10.1371/journal.pmed.1003871
74. Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. The Lancet. 2021;0. https://doi.org/10.1016/S0140-6736(20)32656-8
75. World Health Organization. Constitution of the World Health Organization. https://www.who.int/about/governance/constitution
76. Jennings G, Monaghan A, Xue F, Mockler D, Romero-Ortuño R. A systematic review of persistent symptoms and residual abnormal functioning following acute COVID-19: Ongoing symptomatic phase vs. post-COVID-19 syndrome. J Clin Med. 2021;10(24):5913. https://doi.org/10.3390/jcm10245913
77. Malik P, Patel K, Pinto C, et al. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)—A systematic review and meta-analysis. J Med Virol. 2022;94(1):253-262. https://doi.org/10.1002/jmv.27309
78. Pizarro-Pennarolli C, Sánchez-Rojas C, Torres-Castro R, et al. Assessment of activities of daily living in patients post COVID-19: A systematic review. PeerJ. 2021;9:47. https://doi.org/10.7717/peerj.11026
79. Edemekong PF, Bomgaars DL, Sukumaran S, Levy SB. Activities of daily living. StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK470404/
80. Fernández-de-las-Peñas C, Martín-Guerrero JD, Navarro-Pardo E, Rodríguez-Jiménez J, Pellicer-Valero OJ. Post-COVID functional limitations on daily living activities are associated with symptoms experienced at the acute phase of SARS-CoV-2 infection and internal care unit admission: A multicenter study. J Infect. 2022;84(2):248-288. https://doi.org/10.1016/j.jinf.2021.08.009
81. Nittas V, Gao M, West EA, et al. Long COVID through a public health lens: An umbrella review. Public Health Rev. 2022;43:1604501. https://doi.org/10.3389/phrs.2022.1604501
82. Reuschke D, Houston D. The impact of Long COVID on the UK workforce. Appl Econ Lett. 2022;0(0):1-5. https://doi.org/10.1080/13504851.2022.2098239
83. US Census Bureau. Week 46 household pulse survey: June 1 – June 13. Census.gov. Published June 22, 2022. https://www.census.gov/data/tables/2022/demo/hhp/hhp46.html
84. Fox J. Long COVID is showing up in the employment data. Bloomberg.com. Published June 15, 2022. https://www.bloomberg.com/opinion/articles/2022-06-15/long-covid-is-showing-up-in-the-employment-data
85. Bach K. New data shows long Covid is keeping as many as 4 million people out of work. Brookings. Published August 24, 2022. https://www.brookings.edu/research/new-data-shows-long-covid-is-keeping-as-many-as-4-million-people-out-of-work/
86. Herrera JE, Niehaus WN, Whiteson J, et al. Multidisciplinary collaborative consensus guidance statement on the assessment and treatment of fatigue in postacute sequelae of SARS-CoV-2 infection (PASC) patients. PM&R. 2021;13(9):1027-1043. https://doi.org/10.1002/pmrj.12684
87. Post COVID-19 condition: Guidance for primary care. Ontario Health; 2021:3. https://www.ontariohealth.ca/sites/ontariohealth/files/2021-12/PostCovidConditionsClinicalGuidance_EN.pdf
88. Rehabilitation & allied health practice considerations: Post – COVID-19. Alberta Health Services; 2022. https://www.albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-rehab-allied-health-practice-considerations-post-covid.pdf
89. Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute COVID-19 in primary care. BMJ. 2020;370:m3026. https://doi.org/10.1136/bmj.m3026
90. Vu T, McGill SC. CADTH horizon scan: An overview of post–COVID-19 condition (long COVID). Can J Health Technol. 2021;1(9). https://doi.org/10.51731/cjht.2021.160
91. STIMULATE-ICP: Understanding Long COVID to improve diagnosis, treatment and care. https://www.stimulate-icp.org/care
92. Sivan DM. Long COVID multidisciplinary consortium: Optimising treatments and services across the NHS (LOCOMOTION). clinicaltrials.gov; 2021. Accessed August 24, 2022. https://clinicaltrials.gov/ct2/show/NCT05057260
93. Evidence Synthesis Briefing Note: The assessment and treatment of post-COVID-19 condition. Evidence Synthesis Network; 2022. https://esnetwork.ca/wp-content/uploads/2022/05/85.-Evidence-Synthesis-BN_The-Assessment-and-Treatment-of-Post-COVID-19-Condition_14-APR-2022.pdf
94. Daynes E, Gerlis C, Singh SJ. The demand for rehabilitation following COVID-19: A call to service providers. Physiotherapy. 2021;113:A1-A3. https://doi.org/10.1016/j.physio.2021.05.004
95. Baraniuk C. COVID-19: How Europe is approaching long covid. BMJ. 2022;376:o158. https://doi.org/10.1136/bmj.o158
96. Parkin A, Davison J, Tarrant R, et al. A multidisciplinary NHS COVID-19 service to manage post-COVID-19 syndrome in the community. J Prim Care Community Health. 2021;12:21501327211010990. https://doi.org/10.1177/21501327211010994
97. Verma AA, Hora T, Jung HY, et al. Characteristics and outcomes of hospital admissions for COVID-19 and influenza in the Toronto area. CMAJ Can Med Assoc J J Assoc Medicale Can. 2021;193(12):E410-E418. https://doi.org/10.1503/cmaj.202795
98. Parker AM, Brigham E, Connolly B, et al. Addressing the post-acute sequelae of SARS-CoV-2 infection: A multidisciplinary model of care. Lancet Respir Med. 2021;9(11):1328-1341. https://doi.org/10.1016/S2213-2600(21)00385-4
99. Jiang DH, McCoy RG. Planning for the post-COVID syndrome: How payers can mitigate long-term complications of the pandemic. J Gen Intern Med. 2020;35(10):3036-3039. https://doi.org/10.1007/s11606-020-06042-3
100. Kaur S, Singh B. An overview of the impact of COVID-19 on the Indian health insurance sector and post COVID-19 management. Int Manag Rev. 2022;18:5.http://www.americanscholarspress.us/journals/IMR/pdf/IMR-SP-2022/SpecV18-art9.pdf
101. Government of Ontario. Social assistance. ontario.ca. http://www.ontario.ca/page/social-assistance
102. Caminsky N. Nearly 40% of Canadian adults have had an Omicron infection: Canadian blood services. COVID-19 Immunity Task Force. Published June 7, 2022. https://www.covid19immunitytaskforce.ca/nearly-40-of-canadian-adults-have-had-an-omicron-infection-canadian-blood-services/
103. Levitt H. Insurers are denying long-term disability benefits to those afflicted with Long COVID. Here’s how to fight back. Financial Post. Published September 28, 2021. https://financialpost.com/fp-work/insurers-are-denying-long-term-disability-benefits-to-those-afflicted-with-long-covid-heres-how-to-fight-back
104. Ministry of Health and Long-Term Care Government of Ontario. Ontario Health Insurance Plan: Temporary increases for primary health care services. Published 2022. https://www.health.gov.on.ca/en/pro/programs/ohip/bulletins/redux/bul220403.aspx
105. Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280-286. https://doi.org/10.7326/0003-4819-158-4-201302190-00009
106. What is GRADE? BMJ Best Practice. https://bestpractice.bmj.com/info/toolkit/learn-ebm/what-is-grade/
Document Information & Citation
Author Contributions: KLQ, GMK, PB, and FAR conceived the Science Brief. KLQ, GMK, and PB wrote the first draft of the Science Brief. KLQ, GMK, and PB performed the analyses. All authors revised the Science Brief critically for important intellectual content and approved the final version.
Citation: Quinn KL, Katz GM, Bobos P, et al. Understanding the post COVID-19 condition (long COVID) in adults and the expected burden for Ontario. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2022;3(65). https://doi.org/10.47326/ocsat.2022.03.65.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners can be found at https://covid19-sciencetable.ca/. The declarations of interest of external authors can be found under Additional Resources.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners.
