Key Message
This Science Brief provides information for health care professionals about Vaccine-Induced Immune Thrombotic Thrombocytopenia (VITT), also known as Vaccine-Induced Prothrombotic Immune Thrombocytopenia (VIPIT) and Thrombotic Thrombocytopenia Syndrome (TTS). This is a rare adverse eventfollowing adenovirus vector COVID-19 vaccines, including the AstraZeneca/COVISHIELD and Janssen/Johnson & Johnson COVID-19 vaccines.
This brief describes the pathophysiology, presentation, diagnostic work-up and treatment of VITT.
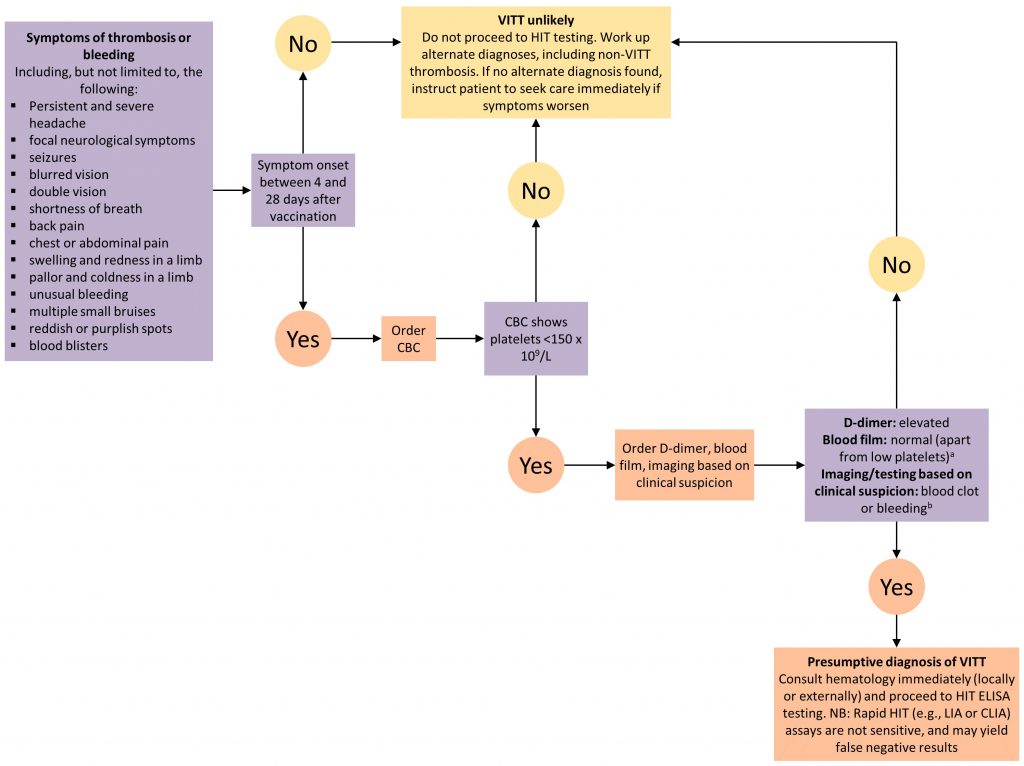
Figure 1. Decision Tree for Diagnosing and Ruling Out VITT
aBlood film to rule out platelet clumping as a cause of low platelet count; bNot all cases of VITT initially present with a clot or bleeding. Patients with all of the features of presumptive VITT (low platelets, high D-dimer, presenting 4 to 28 days post-vaccination) but NO blood clot or bleeding merit hematology consultation (locally or externally) to consider starting treatment until the results of confirmatory testing are back. VITT, vaccine-induced immune thrombotic thrombocytopenia. CBC, complete blood count. HIT, heparin induced thrombocytopenia. ELISA, enzyme linked immunosorbent assay. LIA, latex immunoturbidometric assay. CLIA, chemiluminescent immunoassay.
Lay Summary
What do we know so far?
The AstraZeneca/COVISHIELD COVID-19 vaccine appears to be associated with rare cases of serious blood clots, including blood clots in the brain and other critical organs. Similar cases have also been reported following the Janssen/Johnson & Johnson COVID-19 vaccine. These blood clots have two important features: they can occur 4 to 28 days after vaccination, and they are associated with low platelets (tiny blood cells that help form blood clots to stop bleeding). Doctors are calling this “vaccine-induced immune thrombotic thrombocytopenia” (VITT), “vaccine-induced prothrombotic immune thrombocytopenia” (VIPIT), or “thrombotic thrombocytopenic syndrome” (TTS). These blood clots are different from the blood clots most people are familiar with; they are more aggressive and are more likely to cause death or severe disability, even with early diagnosis and treatment.
Published estimates of the incidence of VITT range from 1 case per 26,000 to 1 case per 127,000 doses of AstraZeneca/COVISHIELD administered. The estimates vary by country, with countries like Norway and Denmark reporting the highest rates. As of April 28, 2021, the rate of VITT in Canada has been estimated to be approximately 1 per 100,000 doses. Nearly all reported cases have occurred after the first dose. There have been few reported cases of VITT with the Janssen/Johnson & Johnson vaccine, so it is difficult to calculate a precise rate, but the incidence of VITT appears to be approximately 1 case per 500,000 vaccine doses administered.
Are certain people more likely to get VITT?
At this time, we do not know if certain patients are more likely to get VITT. Currently, we do not have any evidence that VITT is more common in people who have had blood clots before, people with a family history of blood clots, people on birth control or other hormones, people with autoimmune disease, people with low platelets or other platelet disorders, or pregnant people, because VITT does not develop through the same process as more common types of bleeding or clotting problems. It may be possible, however, that people with a history of heparin induced thrombocytopenia (HIT) or cerebral sinus vein thrombosis (CSVT) with low platelets are at increased risk of VITT; they should receive an mRNA vaccine (Pfizer or Moderna) rather than an adenoviral vector vaccine.
What should you look out for if you received the AstraZeneca/COVISHIELD or Janssen/Johnson & Johnson COVID-19 vaccine?
You should speak to a health care professional if you have unusual or severe symptoms after any COVID-19 vaccine. If you experience the following symptoms that start between 4 and 28 days after vaccination, it might indicate that you have VITT: a severe headache that does not go away; a seizure; difficulty moving part of your body; new blurry vision or double vision that does not go away; difficulty speaking; shortness of breath; severe chest, back, or abdominal pain; unusual bleeding or bruising; new reddish or purplish spots, or blood blisters; or new severe swelling, pain, or colour change of an arm or a leg. These symptoms can also be a sign of other serious conditions and should be assessed in an emergency department.
What should you do if you have concerning symptoms after the AstraZeneca/COVISHIELD or Janssen/Johnson & Johnson COVID-19 vaccine?
If you have severe symptoms such as those listed above, you should go to the nearest emergency department immediately. If you have other symptoms that are not severe, you can discuss them (virtually or in-person) with your primary healthcare professional. You should tell the health care providers who see you that you received the AstraZeneca/COVISHIELD or Janssen/Johnson & Johnson COVID-19 vaccine and give them the date you got vaccinated. If the healthcare professional who assesses you is concerned, you may have scans done and additional bloodwork collected. When recognized early, VITT can be successfully treated.
Do healthcare professionals know how to diagnose and treat VITT?
Health care professionals and scientists in Ontario have been working with experts in Canada, and around the world, to better understand VITT. The Ontario COVID-19 Science Advisory Table has summarized what we know about VITT right now and has published guides for healthcare professionals outside and inside of hospitals to help them diagnose and treat VITT.
Why is Ontario still using the AstraZeneca/COVISHIELD and Janssen/Johnson & Johnson COVID-19 vaccines?
Health Canada has authorized the AstraZeneca/COVISHIELD COVID-19 vaccine, as well as the Janssen/Johnson & Johnson vaccine for use in Canadians aged 18 years and above. The National Advisory Committee on Immunization (NACI) makes a strong preferential recommendation for mRNA vaccines for all Canadians. NACI has recommended that the AstraZeneca/COVISHIELD and Janssen/Johnson & Johnson vaccine may be offered to Canadians 30 years of age and older, if the benefits outweigh risks of waiting for an mRNA vaccine, the decision to receive the vaccine is informed by risks and consequences of VITT, and the delay to receive an mRNA vaccine is substantial.
There have been over 1.1 million cases of COVID-19 diagnosed in Canada so far, COVID-19 has killed over 24,000 Canadians, about 1 in 100 Canadians who get COVID-19 end up needing intensive care. The AstraZeneca/COVISHIELD and Janssen/Johnson & Johnson vaccines are both effective at reducing hospitalization and severe illness from COVID-19, and at reducing the chance you could pass the SARS-CoV-2 virus on to others. Health care professionals, scientists, and government agencies in Ontario – and around the world – will continue to monitor the safety of these and all COVID-19 vaccines.
Could other COVID-19 vaccines available in Ontario cause VITT?
There have been no confirmed cases of VITT with the Pfizer or Moderna COVID-19 vaccines.
Summary
Background
Adenoviral vector COVID-19 vaccines, including the AstraZeneca/COVISHIELD vaccine and the Janssen/Johnson & Johnson vaccine, are associated with immune thrombosis that is similar to heparin-induced thrombocytopenia (HIT).
In March 2021, the United Kingdom, European Union, and Scandinavian countries began reporting rare cases of thrombosis (including splanchnic thrombosis and cerebral sinus vein thrombosis (CSVT)) and thrombocytopenia in patients who received the AstraZeneca/COVISHIELD COVID-19 vaccine. Further cases were reported in Canada and other countries, and in the United States after administration of the Janssen/Johnson & Johnson COVID-19 vaccine.1 Women and young people appear to be slightly overrepresented in reported cases, and thrombosis seems to occur 4 to 28 days after vaccination. Affected individuals have antibodies targeted against platelet factor 4 (PF4) that induce massive platelet activation, reducing the platelet count and causing thrombosis.2–4 (The delayed onset of symptoms after vaccination is likely due to the lag between antigen presentation and development of specific antibodies.) This phenomenon is similar to HIT, but, unlike HIT, VITT does not require heparin as a trigger. It has been referred to as Vaccine-Induced Immune Thrombotic Thrombocytopenia (VITT), Vaccine-Induced Prothrombotic Immune Thrombocytopenia (VIPIT), and Thrombosis Thrombocytopenia syndrome (TTS). In this Science Brief, the term VITT will be used.
Questions
How frequent is VITT?
Are certain patients predisposed to VITT?
When should I suspect my patient has VITT?
How do I diagnose VITT? How do I rule it out?
How do I treat VITT?
Is VITT a reportable event?
Can patients who develop VITT safely receive a second dose of the same COVID-19 vaccine? Can they receive another COVID-19 vaccine?
Findings
How frequent is VITT?
Published estimates of the incidence of VITT range from 1 case per 26,000 to 1 case per 127,000 doses of AstraZeneca/COVISHIELD administered.4–7 The rate of VITT in Canada as of April 28, 2021 has been estimated to be approximately 1 per 100,000 doses.8 The estimates have increased as we have learned more about VITT, and they vary by country with countries like Norway and Denmark reporting the highest rates.4They may continue to increase with better recognition of the disease. Nearly all reported cases have occurred after the first dose.6 There have been few reported cases of VITT with the Janssen/Johnson & Johnson vaccine thus far, so it is challenging to calculate a precise frequency, but the incidence of VITT appears to be approximately 1 case per 500,000 vaccine doses administered.9
There is no evidence that the AstraZeneca/COVISHIELD or Janssen/Johnson & Johnson COVID-19 vaccines increase the overall risk of thrombosis (e.g., deep vein thromboses, pulmonary emboli, myocardial infarction, stroke) without thrombocytopenia, beyond what is seen in the general population. However, there is an observed increase in thrombosis with thrombocytopenia, including an observed increase in unusual clots like CSVT.
AstraZeneca/COVISHIELD and Janssen/Johnson & Johnson COVID-19 vaccines are highly effective in reducing hospitalization and severe illness from COVID-19 and in reducing transmission to others. Health Canada, the United Kingdom Medicines and Healthcare Products Regulatory Agency, and the European Medicines Agency have recommended to continue administering adenoviral vector COVID-19 vaccines.10–12Physicians, scientists, and regulatory agencies worldwide will continue to carefully monitor the safety of the AstraZeneca/COVISHIELD and Janssen/Johnson & Johnson COVID-19 vaccines.
Are certain patients predisposed to VITT?
At this time, it is not clear if certain patients are predisposed to VITT. Early reported cases were predominantly in younger women, however these individuals may have been overrepresented in the vaccinated population in reporting countries. Cases have now been reported in men and in older adults. Since VITT appears immune-mediated and linked to a very specific antigen, an individual with classical risk factors for blood clots, including thrombophilia, a family history of blood clots, a personal history of arterial or venous clots, autoimmune disease, low platelets without a history of clotting, a disorder of platelet function, or who is on birth control or other hormones, or who is pregnant, is probably not at increased risk of VITT. Accordingly, there are no new contraindications to receiving the AstraZeneca/COVISHIELD or Janssen/Johnson & Johnson COVID-19 vaccine. However, Health Canada recommends that individuals who have experienced a previous CVST with thrombocytopenia or HIT should only receive the AstraZeneca/COVISHIELD or Janssen/Johnson & Johnson COVID-19 vaccine if the potential benefits outweigh the potential risks; they may be at increased risk of VITT.13,14
The National Advisory Committee on Immunization (NACI) makes a strong preferential recommendation for mRNA vaccines for all Canadians. NACI has recommended that the AstraZeneca/COVISHIELD or Janssen/Johnson & Johnson vaccine may be offered to Canadians 30 years of age and older, if the benefits outweigh risks of waiting for an mRNA vaccine, the decision to receive the vaccine is informed by risks and consequences of VITT, and the delay to receive an mRNA vaccine is substantial.8 NACI outlines that risk-benefit decisions should be informed by several factors including the local COVID-19 epidemic conditions, local vaccine supply, an individual’s risk of severe illness and death if they develop COVID-19, and their risk of exposure to the SARS-CoV-2 virus.
When should I suspect my patient has VITT?
Patients with VITT may present with CSVT, or with other arterial or venous clots. Any patient with unusual symptoms following vaccination should be assessed by a health care provider. Some symptoms make it more likely that a patient has VITT: persistent and severe headache; focal neurological symptoms (including blurred or double vision); shortness of breath; chest, back, or abdominal pain; unusual bleeding, bruising, petechiae, or blood blisters; swelling and redness in a limb; or pallor and coldness in a limb. VITT seems to occur between 4 and 28 days post-vaccination. Symptoms that begin in this time frame should raise the clinical suspicion of VITT.
Patients with symptoms suspicious of VITT should urgently seek care at their nearest emergency department. Patients with non-severe symptoms may have initial investigations done in the primary care or outpatient setting (see Figure 1).
How do I diagnose VITT? How do I rule it out?
Clinicians should ask patients about their COVID-19 vaccine history and should draw a complete blood count (CBC). VITT is unlikely if symptom onset falls outside of the 4 to 28 day time frame OR if the platelet count is ≥150 x 109/L.2–4,15,16 VITT is more likely if symptom onset falls within the 4 to 28 day time frame AND the platelet count is < 150 x 109/L, and such patients should be evaluated at their nearest emergency department for suspected VITT. This will expedite further diagnostic workup, treatment, and urgent hematology consultation (local or external).
Patients with suspected VITT should go on to have bloodwork drawn including a D-dimer level and a blood film (also referred to as peripheral blood smear) to rule out platelet clumping. They should also have diagnostic imaging/testing to investigate for arterial and/or venous blood clots or bleeding, based on their clinical symptoms.
Unenhanced CT brain is a reasonable first diagnostic imaging test if CSVT is suspected, given CSVT’s nonspecific clinical presentation and the importance of ruling out alternate diagnoses. However, CSVT can only be ruled out with both parenchymal imaging and vascular imaging, with a CT head / MR head and a CT venogram / MR venogram.17 When clinical suspicion of CSVT is high, this potential diagnosis should be investigated urgently with same-day neuroimaging. In centres where imaging is not emergently available and there is a high clinical suspicion of VITT, appropriate treatment should be initiated while imaging is arranged.
Thrombocytopenia with an elevated D-dimer, a normal blood film (apart from thrombocytopenia), and confirmation of a blood clot or bleeding on diagnostic imaging makes the diagnosis of VITT presumptive. VITT can also manifest with a low fibrinogen as evidence of more disseminated coagulation consumption.
There have been reports of patients with all of the features of presumptive VITT (low platelets, high D-dimer, symptoms starting 4 to 28 days post-vaccination) but no confirmed blood clot. These patients may have an early VITT syndrome. Their workup and initial management should be similar to presumptive VITT; in consultation with a hematologist, anticoagulation may be started until the results of confirmatory testing are received.18 There have been no reports of patients with VITT who have normal platelet counts >150 x 109/L. However, given the rapid evolution of knowledge, it is appropriate to monitor patients with symptoms starting 4 to 28 days post-vaccination whose platelets are >150 x 109/L if there is clinical concern regarding an alternate diagnosis. If no other diagnosis is made and the patient is discharged home, they should be instructed to return for a repeat assessment and repeat CBC if their symptoms change or worsen.
The confirmatory diagnosis of VITT is made by using tests that are also used for HIT, but with some important caveats. This testing should be done even if the patient has had no previous exposure to heparin. Like HIT, VITT testing involves two steps: identification of antibodies against the complex of platelet factor 4 and heparin; and confirmatory functional testing of the antibodies’ ability to activate platelets.16,19 The HIT ELISA (enzyme linked immunosorbent assay) antibody test appears to be sensitive for VITT because of specific parameters of the assay that also make it applicable to VITT; if it is positive, VITT is confirmed, and if it is negative, VITT is unlikely.16
Importantly, other HIT antibody tests, like the Rapid HIT tests (e.g., latex immunoturbidometric assay (LIA), chemiluminescent immunoassay (CLIA) are not sensitive for VITT, and are likely to yield false negative results. It is important to consult with a hematologist, and the testing laboratory, to ensure that an ELISA method is used for antibody testing. A number of large laboratories test for HIT antibodies using the ELISA method in Ontario, but only one laboratory in Canada performs confirmatory functional testing (the McMaster University Platelet Immunology Laboratory). Therefore, presumptive VITT should prompt an urgent hematology consultation (in person, virtually, or by phone) to arrange HIT ELISA testing, initiate confirmatory functional testing at the national reference laboratory, and start appropriate empiric treatment of blood clots (see below). All testing (HIT ELISA and functional testing) must be sent prior to administration of IVIG treatment, as IVIG can interfere with the results.16
How do I treat VITT?
Patients with presumptive and confirmed VITT should be treated similarly to HIT. Treatment should ideally occur in an emergency department or hospital setting, where the patient can be closely monitored.
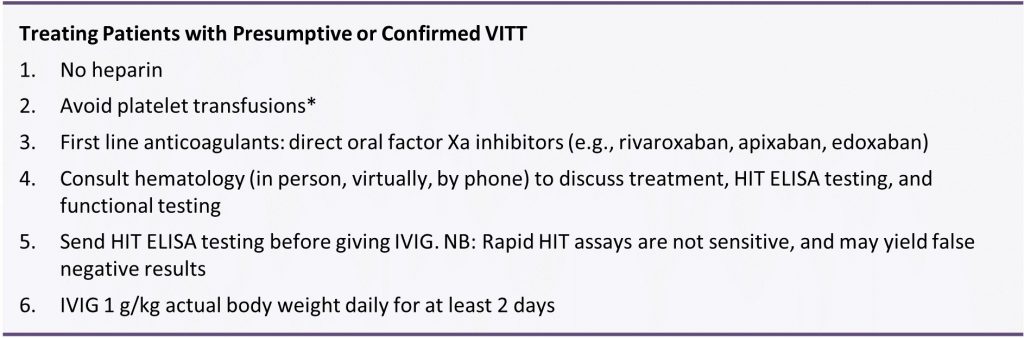
*Platelet transfusions could theoretically worsen the clotting; if patients present with a life-threatening bleed, platelets should only be transfused under the guidance of a hematologist.
Until VITT has been ruled out, anticoagulation with heparin (unfractionated heparin and low molecular weight heparins) should be avoided. Platelet transfusions should be avoided.
Alternative anticoagulants that are safe to use in HIT, and likely safe to use in VITT, include direct thrombin inhibitors and factor Xa inhibitors. Direct oral factor Xa inhibitors (e.g., rivaroxaban, apixaban, edoxaban) should be started empirically while awaiting further advice from a hematologist; these agents are used in the treatment of HIT. The dose of direct oral factor Xa inhibitor is identical to the dose used to treat uncomplicated deep vein thromboses. If the patient has severe renal impairment that makes direct oral anticoagulants unsafe, or is too unwell or unstable to take oral medication, advice from a hematologist should be sought to guide use of parenteral anticoagulants that are safe to use in HIT (e.g., argatroban). In pregnant and lactating patients with presumptive or confirmed VITT, direct oral factor Xa inhibitors are not recommended; advice from a hematologist should be sought to guide use of safe non-heparin anticoagulants.
In patients with presumptive or confirmed VITT, it is important to dampen the prothrombotic response and increase platelet counts with intravenous immunoglobulin (IVIG). Administration of high dose IVIG (1 g/kg of actual body weight daily for at least two days) is appropriate and can be guided by the consulting hematologist.
Patients with all of the features of presumptive VITT (low platelets, high D-dimer, symptoms starting 4 to 28 days post-vaccination) but who have NO evidence of thrombosis or bleeding may have an early VITT syndrome. In these patients, it is important to consult hematology and consider starting anticoagulation and/or IVIG until the results of confirmatory laboratory testing are available.
Is VITT a reportable event?
All suspected adverse events following immunization (AEFI), including thrombosis, thrombocytopenia, and both presumptive and confirmed VITT, should be reported using the provincial AEFI form and sent to the local Public Health Unit. More information on how to report AEFIs can be found on the Public Health Ontario website. Ontario conducts vaccine surveillance safety in collaboration with the Public Health Agency of Canada, and prompt reporting is essential to learn more about this rare but serious thrombotic phenomenon.
Can patients who develop VITT safely receive a second dose of the same vaccine? Can they receive another COVID-19 vaccine?
Patients who have experienced major venous or arterial thrombosis with thrombocytopenia following vaccination with the AstraZeneca/COVISHIELD COVID-19 vaccine or the Janssen/Johnson & Johnson vaccine should not receive a second dose of either of these vaccines.13,14 There have been no confirmed cases of VITT with mRNA-based COVID-19 vaccines (e.g., Pfizer and Moderna). Therefore, a second dose of mRNA-based COVID-19 vaccines may be safe.
Interpretation
VITT is a rare adverse event following the AstraZeneca/COVISHIELD and Janssen/Johnson & Johnson vaccines. This brief describes the pathophysiology, presentation, diagnostic work-up and treatment of VITT, including a decision tree for diagnosing and ruling out VITT.
References
1. See I, Su JR, Lale A, et al. US case reports of cerebral venous sinus thrombosis with thrombocytopenia after Ad26.COV2.S vaccination, March 2 to April 21, 2021. JAMA. Published online April 30, 2021. https://doi.org/10.1001/jama.2021.7517
2. Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S. Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination. N Engl J Med. Published online April 9, 2021. https://doi.org/10.1056/NEJMoa2104840
3. Scully M, Singh D, Lown R, et al. Pathologic antibodies to platelet factor 4 after ChAdOx1 nCoV-19 vaccination. N Engl J Med. Published online April 16, 2021. https://doi.org/10.1056/NEJMoa2105385
4. Schultz NH, Sørvoll IH, Michelsen AE, et al. Thrombosis and thrombocytopenia after ChAdOx1 nCoV-19 vaccination. N Engl J Med. Published online April 9, 2021. https://doi.org/10.1056/NEJMoa2104882
5. Pottegård A, Lund LC, Karlstad Ø, et al. Arterial events, venous thromboembolism, thrombocytopenia, and bleeding after vaccination with Oxford-AstraZeneca ChAdOx1-S in Denmark and Norway: population based cohort study. BMJ. 2021;373:n1114. https://doi.org/10.1136/bmj.n1114
6. Government of United Kingdom. Coronavirus vaccine – weekly summary of Yellow Card reporting. GOV.UK. Published April 29, 2021. https://www.gov.uk/government/publications/coronavirus-covid-19-vaccine-adverse-reactions/coronavirus-vaccine-summary-of-yellow-card-reporting
7. Australian Government. COVID-19 vaccine weekly safety report – 06-05-2021. Therapeutic Goods Administration (TGA). Published May 6, 2021. Accessed May 7, 2021. https://www.tga.gov.au/periodic/covid-19-vaccine-weekly-safety-report-06-05-2021
8. Advisory Committee Statement (ACS). Recommendations on the Use of COVID-19 Vaccines. National Advisory Committee on Immunization (NACI); 2021:120. https://www.canada.ca/content/dam/phac-aspc/documents/services/immunization/national-advisory-committee-on-immunization-naci/recommendations-use-covid-19-vaccines/recommendations-use-covid-19-vaccines-en.pdf
9. Oliver S. Risk/Benefit Assessment of Thrombotic Thrombocytopenic Events after Janssen COVID-19 Vaccines. Advisory Committee on Immunization Practices (ACIP); 2021:76. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-04-23/06-COVID-Oliver-508.pdf
10. European Medicines Agency. AstraZeneca’s COVID-19 vaccine: benefits and risks in context. European Medicines Agency. Published April 23, 2021. https://www.ema.europa.eu/en/news/astrazenecas-covid-19-vaccine-benefits-risks-context
11. Health Canada. Health Canada provides update on the AstraZeneca and COVISHIELD COVID-19 vaccines. Government of Canada. Published April 16, 2021. https://healthycanadians.gc.ca/recall-alert-rappel-avis/hc-sc/2021/75389a-eng.php
12. Government of United Kingdom. MHRA issues new advice, concluding a possible link between COVID-19 Vaccine AstraZeneca and extremely rare, unlikely to occur blood clots. GOV.UK. Accessed May 4, 2021. https://www.gov.uk/government/news/mhra-issues-new-advice-concluding-a-possible-link-between-covid-19-vaccine-astrazeneca-and-extremely-rare-unlikely-to-occur-blood-clots
13. Health Canada. Product Monograph Including Patient Medication Information: AstraZeneca COVID-19 Vaccine. Government of Canada; 2021:26. https://covid-vaccine.canada.ca/info/pdf/astrazeneca-covid-19-vaccine-pm-en.pdf
14. Health Canada. Product Monograph Including Patient Medication Information: Janssen COVID-19 Vaccine. Government of Canada; 2021:24. https://covid-vaccine.canada.ca/info/pdf/janssen-covid-19-vaccine-pm-en.pdf
15. Nopp S, Moik F, Jilma B, Pabinger I, Ay C. Risk of venous thromboembolism in patients with COVID-19: A systematic review and meta-analysis. Res Pract Thromb Haemost. Published online September 25, 2020. https://doi.org/10.1002/rth2.12439
16. Nazy I, Sachs UJ, Arnold DM, et al. Recommendations for the clinical and laboratory diagnosis of vaccine-induced immune thrombotic thrombocytopenia (VITT) for SARS-CoV-2 infections: Communication from the ISTH SSC Subcommittee on Platelet Immunology. J Thromb Haemost. Published online April 22, 2021. https://doi.org/10.1111/jth.15341
17. Saposnik G, Barinagarrementeria F, Brown RD, et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(4):1158-1192. https://doi.org/10.1161/STR.0b013e31820a8364
18. Thaler J, Ay C, Gleixner KV, et al. Successful treatment of vaccine-induced prothrombotic immune thrombocytopenia (VIPIT). J Thromb Haemost. https://doi.org/10.1111/jth.15346
19. Greinacher A, Selleng K, Warkentin TE. Autoimmune heparin-induced thrombocytopenia. J Thromb Haemost. 2017;15(11):2099-2114. https://doi.org/10.1111/jth.13813
Document Information & Citation
Updated on May 10, 2021.
Author Contributions: MP, PJ and AMM conceived the Science Brief. MP wrote the first draft of the Science Brief. All authors contributed to the conception of the Science Brief, revised it critically for important intellectual content and approved the final version.
Citation: Pai M, Chan B, Stall NM, et al. Vaccine-induced immune thrombotic thrombocytopenia (VITT) following adenovirus vector COVID-19 vaccination. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;2(17). https://doi.org/10.47326/ocsat.2021.02.17.2.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners can be found at https://covid19-sciencetable.ca/. The declarations of interest of external authors can be found under Additional Resources.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners.
