OUTDATED
This version is outdated. Please see https://doi.org/10.47326/ocsat.2021.02.20.2.0 for the latest version of this Science Brief.
Key Message
What do we know so far?
The AstraZeneca COVID-19 vaccine appears to be associated with autoimmune thrombosis that mimics heparin-induced thrombocytopenia (HIT). The United Kingdom, European Union, and Scandinavian countries have reported rare cases of cerebral sinus vein thrombosis (CSVT) and thrombocytopenia in patients who received the AstraZeneca COVID-19 vaccine. The majority of affected patients thus far are women under the age of 55 years, and CSVT seems to occur 4 to 20 days after vaccination. The likely mechanism is antibodies that induce massive platelet activation, reducing the platelet count and causing thrombosis.1 This phenomenon mimics heparin-induced thrombocytopenia (HIT) yet it does not require heparin as a trigger. It has been named vaccine-induced prothrombotic immune thrombocytopenia (VIPIT). The incidence of VIPIT appears to be between 1 in 125,000 and 1 in 1 million.2
Are certain patients predisposed to VIPIT?
At this time, it is not clear if certain patients are predisposed to VIPIT. The cases to date are predominantly in younger women, however these individuals may have been overrepresented in the vaccinated populations in European Union countries.2 Since VIPIT is immune-mediated, an individual with a thrombophilia, a family history of blood clots, or a personal history of arterial or venous clots would likely not be at increased of VIPIT. Accordingly, there are no new contraindications to receiving the AstraZeneca COVID-19 vaccine.
What should primary care providers and patients look out for post-vaccination?
Patients with VIPIT may present with CSVT, or with other arterial or venous clots. Some symptoms make it more likely that a patient has VIPIT: persistent and severe headache, focal neurological symptoms, seizures, or blurred or double vision (suggesting CSVT or arterial stroke); shortness of breath or chest pain (suggesting pulmonary embolism or acute coronary syndrome); abdominal pain (suggesting portal vein thrombosis); or limb swelling, redness, pallor, or coldness (suggesting deep vein thrombosis or acute limb ischemia).
What should primary care providers and patients do if concerning symptoms arise?
All patients with unusual, non-severe symptoms following vaccination should have an assessment (virtual or in-person) with their primary care provider, and a diagnosis of VIPIT should be considered; initial investigations may be done in the primary care setting. Patients with severe symptoms should immediately present to the nearest emergency department.
Figure 1 presents a decision tree for diagnosing and ruling out VIPIT. Clinicians should ask patients about their COVID-19 vaccine history and should draw a complete blood count (CBC). VIPIT is unlikely if symptoms of blood clotting fall out of the 4-to-20-day time frame following COVID-19 vaccination OR if the platelet count is ≥ 150 x 109/L.3
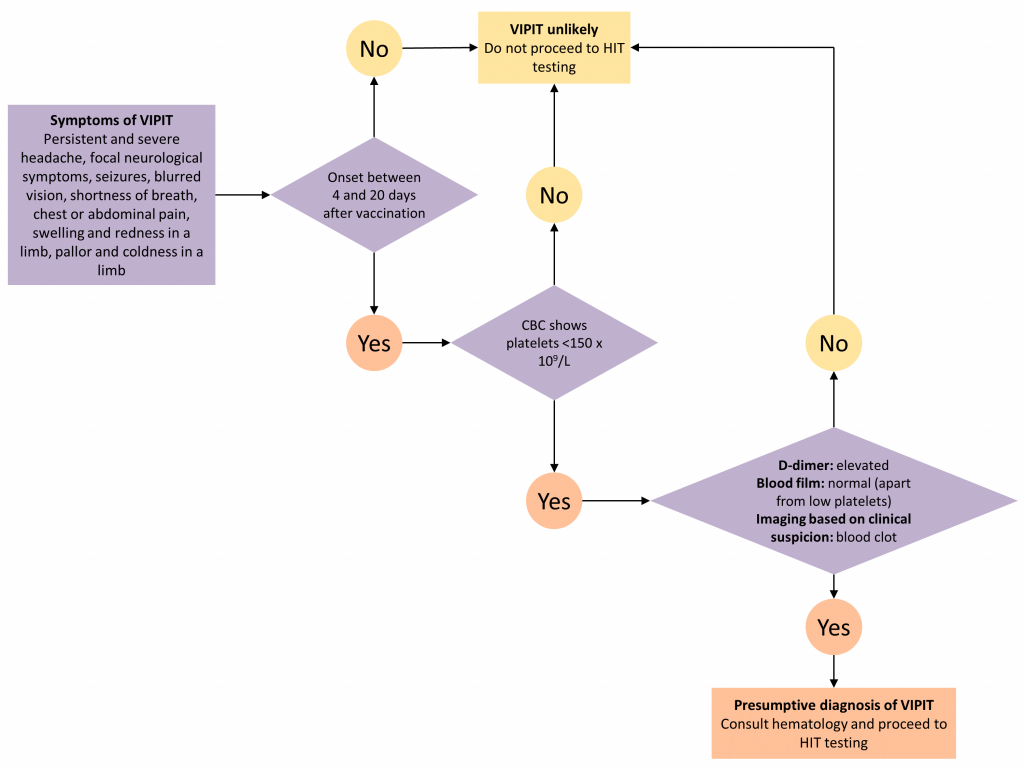
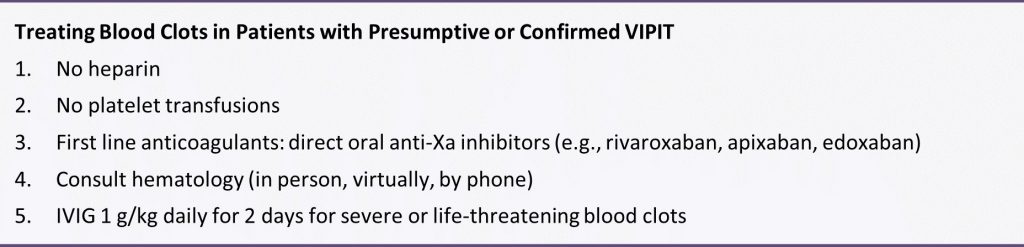
VIPIT is more likely if symptoms of blood clotting fall in the 4-to-20-day time frame AND the platelet count is < 150 x 109/L, and such patients should be evaluated at their nearest emergency department for suspected VIPIT. This will expedite further diagnostic workup, treatment, and urgent hematology consultation. The Box presents the treatment principles for patients with presumptive and confirmed VIPIT.
Is VIPIT a reportable event?
All suspected adverse events following immunization (AEFI), including thrombosis, and both presumptive and confirmed VIPIT, should be reported using the provincial AEFI form and sent to the local Public Health Unit. More information on how to report AEFIs can be found on the Public Health Ontario website. Ontario conducts vaccine surveillance safety in collaboration with the Public Health Agency of Canada, and prompt reporting is essential to learn more about this rare but serious thrombotic phenomenon.
References
1. Updated GTH statement on vaccination with the AstraZeneca COVID-19 vaccine, as of March 22, 2021. Published March 18, 2021. Accessed March 24, 2021. https://gth-online.org/wp-content/uploads/2021/03/GTH_Stellungnahme_AstraZeneca_3_24_2021.pdf
2. PINHO AC. COVID-19 Vaccine AstraZeneca: benefits still outweigh the risks despite possible link to rare blood clots with low platelets. European Medicines Agency. Published March 18, 2021. Accessed March 24, 2021. https://www.ema.europa.eu/en/news/covid-19-vaccine-astrazeneca-benefits-still-outweigh-risks-despite-possible-link-rare-blood-clots
3. Warkentin TE. Heparin-induced thrombocytopenia: pathogenesis and management. Br J Haematol. 2003;121(4):535-555. https://doi.org/10.1046/j.1365-2141.2003.04334.x
Document Information & Citation
Citation: Pai M, Grill A, Ivers N, et al. Vaccine-induced prothrombotic immune thrombocytopenia VIPIT following AstraZeneca COVID-19 vaccination: interim guidance for healthcare professionals in the outpatient setting. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;1(20). https://doi.org/10.47326/ocsat.2021.02.20.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners can be found at https://covid19-sciencetable.ca/. The declarations of interest of external authors can be found under additional resources.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners.
